There's still life in it after 16 June. And while we’re valuing things, is the iconic patient management system vendor worth a whopping $500m?
Two loosely related stories this week on value and general practice.
We are going to start with RACGP membership.
Is membership of the RACGP “good value” after 16 June, the date after which a GP will no longer require membership of one of the two colleges to report and monitor their CPD, and through that process maintain specialist status and the ability to charge higher Medicare rebates?
It’s a question I couldn’t possibly answer: I’m not a GP, and there exists a whole spectrum of tangible and emotional value propositions by which a GP might measure their value of membership.
The only sure thing you can say is, whatever the value was before 16 June, depending on how you view the whole CPD situation, after that date there are significant arguments to suggest the value of membership for some GPs will have lessened significantly.
How does the college present value in these times of change?
It is certainly cognisant of the CPD issue in its current pitch for members. And it’s perhaps interesting that now they don’t have a CPD hook, their major pitch seems to be advocacy.
Current college president, Dr Karen Price, says in a prominent spot on the college’s website: “As an RACGP member, your voice makes a significant difference in our ability to advocate for the best possible outcomes for you and your patient.
“You may be aware of the legislative changes affecting CPD that will come into effect this year, changes that mean you have choices when it comes to your membership. I want to assure you that the RACGP – your college – will always support you to advance your career and continue to deliver the highest quality of care to patients.”
It probably doesn’t help that there has been so much disaffection among the GP community about the college’s advocacy performance in Canberra that a new GP group has emerged with a singular focus on lobbying and advocacy, claiming that the RACGP has largely failed there – ironically, in large part because it is conflicted by its tight relationship with the federal government on CPD, but also in training and education.
The new group, the Australian Society of General Practitioners (ASGP), has to date been spurned by the RACGP as a group that could splinter the power of the college to advocate. But the ASGP maintains that with a sole focus on lobbying in Canberra for better pay for GPs and for Canberra taking the profession a lot more seriously in its planning for a chronic-care-focused future – and no reliance on any government department for funding for its existence, which the RACGP has – it has a much better chance of succeeding in advocacy where the RACGP has failed for so many years.
Notably, the ASGP does not spurn the RACGP. Its founder and president, Dr Chris Irwin, says he is a proud member of the college and he sees value in being a member. He just doesn’t see that value being in advocacy.
If as a GP you arrive at the conclusion that CPD and advocacy aren’t value propositions that merit being an RACGP member, what is left?
There is still quite a bit. Following are some tangible and not so tangible value propositions.
(Tip: this list is long and impressive but a bit boring, so if you want to skip through it to the conclusion, the conclusion is that actually, for the money, membership of the RACGP isn’t such bad value. You can read on from the bottom of this dot point list, if you like).
- Ability to participate in or contribute to:
- Several expert committees that will have some say and influence on how general practice proceeds clinically, digitally and otherwise. These committees are seen as important influencers by the government on several fronts. For example, the Department of Health will nearly always seek counsel with an RACGP and ACRRM expert committee on major changes to things such as digital health access and clinical guidelines
- GP research, or the administration and development of key areas of research, as the college receives and administrates a lot of funding
- Policy development: college members and leadership are often involved in government programs on development of healthcare policy for obvious reasons
- Advocacy: the college does attempt to advocate a lot on behalf of GPs, albeit while conflicted. As Dr Irwin points out, it is inhibited in how far it can go, and has been pretty bad at it if you consider the history of MBS freezes and ability to influence compliance processes
- A lot more in the vein of all of the above: as the largest GP college, it is highly influential and involved in a lot of healthcare policy setting, community medicine research, and the like. If you join, you may not get directly involved in all of this, but you’d be helping support it
- More immediately tangible benefits include:
- Postnominals: this has become a somewhat controversial topic as the CPD deadline approaches and some members consider leaving as the college at first zigged and zagged around the question, and clearly in the past had allowed members who had lapsed to use the postnominal FRACGP. But if you aren’t a financial member, the college says you aren’t entitled to use FRACGP after your name anywhere. In fact, it trademarked FRACGP in 2014, which means if you do it, you’d be exposing yourself to legal action. That’s problematic in a whole lot of ways for the college, which we discuss in more detail below, but for members, postnominals are useful only for employment situations really. Patients don’t know what they are and don’t care. Outside of that, being able to use them is an emotional thing that is important to a lot of GPs because it’s signifying achievement of a specialisation as a GP
- Subscription to a monthly clinical journal (Australian Journal of General Practice): if you aren’t a member, you won’t to get this journal, but you will get its commercial equivalent, Medicine Today, free anyway, if you are a practising GP. It’s pretty good.
- A daily news service: newsGP. When we say “news” … newsGP does provide a daily service of RACGP-approved information, but only “good” news as far as the RACGP is concerned (it won’t report on anything that the college is doing that you should be upset about), so we are going to say that this service isn’t actually providing a tonne of value
- RACGP Plus, which provides a range of services that the college has negotiated for members at a discounted rate including financial services, travel, cars, and equipment … some are quite good discounts on good brands
- CPD reporting and tracking: yes, if you’re a member, you won’t have to go to the trouble of self-reporting your own CPD. How much trouble does that save? It’s not entirely clear until we see the alternative services emerge, but most will be free (such as that offered in the AMA Doctorportal). Using the AMA service as an example, about the same time and effort you’d go to if you are an RACGP member, so there doesn’t seem to be a lot of additional value offered here now.
- Free and paid education platforms that are pretty good. GPlearning is a CPD platform with lots of CPD on it that is easy to use and entirely online for 24-hour access, and CHECK is a program of free CPD modules regularly delivered to members via print and email.
- Practice management assistance: in the form of online toolkits, and a practice management conference each year, that a member still has to pay for, but at a lower costs to non members.
- Annual conference: again, a member still has to pay to attend the conference, but they get a discount, and when asked what value members get out of the annual conference, the most frequent reply is the ability to catch up with friends and peers (education and learning is rarely given as a reason, but that’s the case with most association conferences).
- A free recruitment service for practices and members: we aren’t aware of how effective this is, but each week there are as many jobs as you’ll see on the key commercial services that charge for the service.
- Discounts of some key clinical texts including The Australian Medicines Handbook (the college is a part owner of this group) and therapeutic guidelines
- Emotional benefit:
- For a proportion of members there is a clear benefit to simply contributing to the GP community and although some people might argue there is a lot of dysfunction in the RACGP community, and it is a very old-fashioned institution now, not listening to its members, and losing its influence and power in the healthcare ecosystem, there is still some value in contributing obviously for some GPs.
- Postnominals: as above, you can’t put FRACGP after your name if you aren’t a member. Feels like emotional blackmail on the part of the college, but there it is.
One of the interesting aspects of RACGP membership until now is that before 16 June, you didn’t really have to think about any of these other many points of value. If you weren’t a member, you couldn’t get your CPD reported and your higher Medicare rebates. A lot of members would have automatically had that in mind at renewal each year. Non-renewal wasn’t an option.
Now it is an option, I wonder how all these points of value would be considered when thinking about renewal.
It’s only $1495 as a full-time member and $945 as a part-time member. You can nearly halve that after a tax deduction for professional body membership.
At about $750 per year, and as a GP community observer, not a GP, I’m going to make my own assessment: that isn’t actually bad value. There’s a lot on offer.
But as an observer, I’m not thinking about the value of the offer. I don’t think the value of the offer is the problem. It’s clearly pretty good value if you look at all those things listed above.
There is something else at play here that I think the RACGP executive and board is missing and it’s pretty big.
RACGP membership might be good value but the RACGP has treated its members with disdain. That’s OK if you’re customers have no option but bad as ongoing business model now RACGP members do have choice.
If I were a GP, the reason I wouldn’t renew would be because the college treats me as currency – a form of finacial instrument – not as a valued member of their community.
Members have never had a decent say in how the money has been spent by the executive and the leadership of the college, and let’s face it, a lot of the money has been spent badly, so this puts the college in a poor position when asking members to stick with them now.
In countless surveys, members have expressed dismay at how their voice as members seems to have little or no impact on the leadership. The leadership has paid lip service largely to listening via things like the annual post AGM convocation (which has ironically been scrapped in the last year). It has in large part ignored its members because the CPD situation has allowed it too. The board didn’t need to listen as membership revenue was guaranteed. And largely they didn’t listen.
For the college leadership to not to listen now, after the CPD changes, would be foolish. The college is now in open waters. Proper market forces are in play. Members can walk if they want too. But the executive and leadership don’t seem to have woken up to that properly yet.
The executive and leadership could do a mea culpa on their past, and start on a path of listening and valuing their members.
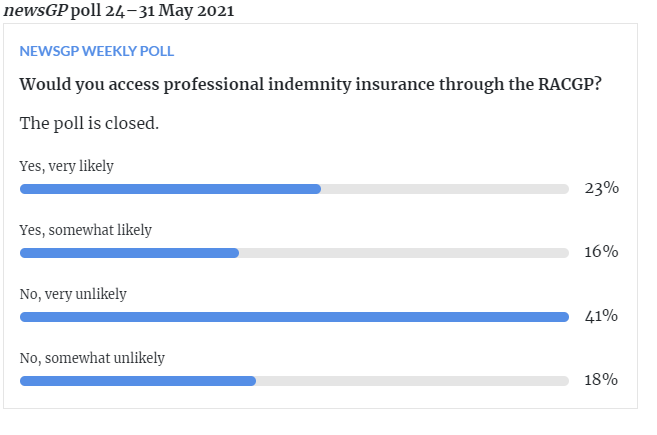
But they haven’t, so far – unless you count a weekly survey they’re now running via newsGP. This one on indemnity is an interesting proposition (but looks unlikely to get off the ground):
Surely if they don’t start listening now, eventually members will leave the college in droves?
That they haven’t been listening to date is clear by how they have treated the whole CPD and postnominal saga.
On CPD, the college played dumb and would not answer the many questions put to it by the media and some members around whether members could actually leave and still retain their higher Medicare rebates. The college knew a long time ago members could leave, but they attempted to not answer the questions, preferring to leave members in the dark, and playing for time.
How is that valuing members?
On the heels of the CPD confusion came the postnominals fuss.
From TMR’s investigations, it is more than clear that in the past the college had allowed members to use their postnominal if they were no longer a financial member. We had several incoming calls from annoyed members and past members pointing out past communications and practice. We found it hard to get the college to clarify initially.
Was it coincidental that renewal of college membership was approaching fast?
Then a college member sent us an email they had received from RACGP member services confirming they could take their postnominals with them, and when we sent that the college to check last week, the college got back and said, sorry, that was a mistake.
In the meantime, the college announced that it was “reviewing its guidelines” with respect to postnominals.
Again, a review of the postnominals problem would probably have been welcome by members a few months back when they had some semblance of time to consider the implications for their upcoming renewal of membership. As things stand, that review date hasn’t been announced, so it’s almost certainly going to be after membership renewal.
How is that valuing or listening to members?
The final argument here for the college having its business model upside down in terms of how it values its members is their trademark of FRACGP and their less than subtle declaration of that trademark to members in some recent press.
As a business you get a trademark to protect the integrity of your brand and stop “competitors” using that brand to obtain commercial value from using it. In that context, the RACGP is viewing its members as competitors, if they decide, even for a year or two, not to be members. That doesn’t add up.
This is one of the most stupid customer retention strategies I’ve ever seen and it goes some way to explaining to a lot of members that not only is their executive and leadership not listening to them much, they also aren’t very good at business.
First and foremost business is about “valuing your customer” (Actually, that’s not quite right: it’s first and foremost about valuing your staff, and if you do that, your customers are going to be looked after, if you are sensible enough to have in place a base strategy of offering continuous and improving customer value). Recent leaks from RACGP staff seem to suggest there isn’t a lot of valuing of staff going on, and that possibly is resonating in how members are viewed and treated (although that’s probably incorrectly pointing blame at the college’s hard working staff).
The RACGP has never had a real listening and valuing of members strategy, and now when it needs it more than ever, it is marching stubbornly in the opposite direction. If you leave, we are going to punish you! … that’s how much we value your custom, says the RACGP postnominals policy.
Any competent marketing person knows that you will from time to time lose a customer and that this customer is a very high likelihood of coming back if you play your cards right. Look at what you did wrong, or were doing, and fix it. Indeed, do more than fix it if you can.
Threatening members who leave with a law suit for infringing your trademark isn’t in line with this basic rule of marketing.
That the RACGP executive has gotten to this point is a pretty sad indictment of their capability in running a business and points almost certainly to an organisation that drifted along on a monopoly position for years based on CPD where they didn’t have to care about their customers.
The good news is that this is all pretty basic and the RACGP executive can fix it without too much trouble.
Just listen to your members and non-members and show them some genuine love.
The key here is genuinely caring and loving them, something which hasn’t been a factor for long time because it wasn’t required and leadership obviously didn’t see any need for a back-up should that situation ever change.
The value of RACGP membership on paper is pretty good, even if you do want to do your CPD or advocacy elsewhere at the same time.
But the RACGP is going to bleed members and credibility over the coming years in spades if it doesn’t start genuinely loving its members and soon to be lost members.
It all starts with listening.
Is Medical Director worth $500m and what does its sale to Telstra mean for GPs?
I’ve written numerous stories over the years about how much Medical Director (MD), one of our two largest GP patient management vendors, is worth, and more recently about what it might mean if it was sold to Telstra Health, as strong rumours suggest.
In my recent calculation (Our 11 most valuable digital health companies) , Medical Director is worth about $220 million.
Wrong apparently (it occurs quite a bit that I’m wrong as things go).
According to insiders at the Australian Financial Review this week, the going price for the company is going to be about $500 million, and Telstra Health, as previously reported by The Medical Republic, is the front runner in an auction that is due to end early next month.
$500 million?
That would make Frank and Lorraine Pyefinch, and Sonic Healthcare (the major shareholders of Best Practice (BP)), pretty happy I’d imagine, because based on that valuation, BP is worth at least $650 million and possibly up to $1 billion. This is based on it having a much better share of market of GPs, it still gaining share of market based on price and product, over MD, and a few other less well-known factors such as where it is in the development of its cloud version of its product offering.
When I wrote that article and did those valuations, I got a few calls from some of those vendors, who suggested I had under-priced them by quite a bit. I didn’t get a call from Medical Director (I rarely do, because of articles like this I guess), but I did from some market analysts who’d suggested I had over-priced them by quite a bit.
Far be it for me to question long-time financial analysts, who are qualified in the art of valuation, and who work for highly respected institutions such as Bank of America, which is advising Telstra on the sale.
But I will give it go.
Since its sale to private equity group Affinity more than five years ago for $140 million (notably Telstra was interested back then as well), MD has:
- Lost significant amounts of market share in the valuable GP market to BP. Accurate share figures over the years have been impossible to obtain (hopefully those doing the due diligence have their head around this issue) but when Affinity acquired the business five years ago it was generally thought that Best Practice was maybe a little behind in share from MD but catching fast, with each having about 42% each of the market, but now estimates range from 30/55 to 38/47 for MD/BP. That’s a lot of share loss.
- MD has increased both its revenue and profit in that time, which makes sense only if it has put its price up a lot, which it has. So MD is a lot more expensive than BP in most comparisons.
- Anecdotally, BP is a far more loved and trusted brand in the market these days.
- Helix, the cloud version of MD and which was the great marketing hope for MD, has failed to get any traction in the market. Hardly any GP practices use it. This might have been explained away as Helix being ahead of its time, but it doesn’t explain why the other two major cloud vendors, Clinic to Cloud and MediRecords, have managed in one way or another to secure contracts for huge numbers of users, albeit outside of the small to medium GP market, and Helix has failed.
- Note: I am a non-executive director of MediRecords and that prevents me from revealing a few things about that business, but what I can say is that while it has failed to get traction in the GP market as a cloud product, like Helix has failed, it has managed to secure some very large and interesting enterprise contracts that would not have been possible without the product being an agile and scalable patient-management enterprise solution. It beat Helix and MD to these contracts in one way or another.
- Employees who have left MD over the years haven’t been particularly complementary about how it was run, how it treated its customers, and about Helix, which some have claimed was never built as a cloud version of MD but was developed as solution for the bulk-billing model of past owner Primary Healthcare, that could never be adapted properly to being an all-purpose cloud-based ambulatory patient-management solution. I will emphasise here that these are all stories told by ex-employees, and that doesn’t necessarily mean these stories are true. But it doesn’t feel great.
Last but not least in the issues facing a valuation of $500 million is that MD is facing off against the greatest challenge in its commercial history: the rapid advance of disruptive open API, cloud-based solutions to healthcare interoperability.
Nearly all of MD’s revenue and installations are based on old server-bound software technology.
There is some irony here in that the managing director of MD (the MD of MD), Matthew Bardsley, is a cloud zealot. He believes entirely and preaches the future of interoperability in health via the cloud, and in disruptive healthcare business models.
But the vast majority of his company’s installed product base and revenue base is legacy. It, along with a lot of other Australian medical software vendors today, probably including its main competitor, Best Practice, have a giant technology debt.
Such technology debt can be overcome. And if you’re going to do it, the best place to do it from is a position of significant market leadership. While MD isn’t the market leader, it has got significant market share and there is daylight until number three in the market. BP and MD dominate.
But there are huge risks to such technology debt for a buyer. The obvious one is the vast sums of money needed to reinvest in overcoming the debt. If you pay $500 million for MD, you are going to need to pay something like another $50-$100 million to get yourself over your legacy technology position and transitioning your product suite to cloud without destroying your revenue base, as cloud is a different proposition in financial terms for buyers of a patient management system.
In the case of Telstra Health, this probably won’t be a problem. They have tonnes of capital.
The problem more likely is that with highly interoperable cloud-based technologies not quite at a tipping point in the Australian healthcare system, no one could really have confidence that the business model of these major PMS software vendors which is based currently on older server base products will transition easily to a cloud ecosystem.
If you’re a betting person (I always admit I am in moderation), if you have money, a very dominant market position and smarts, you are likely to make it to the other side, so this augurs well for both BP and MD. But it’s not going to happen without a fair bit of blood, sweat and tears, a lot of capital and a fair bit of risk.
Which I would have thought made $500 million look like a high price.
So what might behind a preparedness to outlay so much money on something that looks a little tired, over leveraged (a lot of cost has been removed from the business) and risky? (OK, that’s a little rough, MD makes a lot, has good market share, and is surely worth something like $200 million or more, which is quite a lot so it’s not a terrible business).
Here are three ideas:
- General practice is the most important transactional data point in our healthcare system now, and in the future this position will be amplified substantively as the need to optimise interoperability in patient data between GPs, allied providers, specialists, hospitals and the patients themselves, becomes the secret to system efficiency, security and safety. The GP node is the gatekeeper data position now in the future
- An open operating system, API, cloud world, tends to be a “winner takes all” world. It’s a world where once you have a platform that is used the most, network effects of users and data tend to reinforce one platform. This is why we have Amazon in retail, Facebook in social media, Google in search, Apple in consumer applications access and Microsoft in business apps, and its hard to name who is their main competition. In a cloud world, users reinforce the value of a platform to the point where there are usually few if any No 2s and if you’re number one, the world of opportunity to make money in all sorts of new ways tends to open up. You own distribution. And that means you can charge everyone who wants access, If Telstra buys MD, it must have this in the back of its mind for Australian healthcare, and if this reasoning for valuation turns out to be true, $500 million might end up looking like a bargain.
- The Department of Health looks set to introduce some firm deadlines for healthcare providers and vendors to transition everything they do to the far more interoperable world of the cloud. If we are going to use the UK and the US as examples of how long that timeframe might be, it’s likely about five years’. In the same period, the federal government has said it will spend at least $17 billion on aged care and to do that it knows that it has to digitise the aged care sector and connect it to the rest of the healthcare sector, mainly general practice. The enterprise contracts to make aged care interoperable in healthcare over the next few years are likely to be very lucrative and Telstra Health already has large positions in aged care digital solutions, as well as in other parts of the healthcare delivery chain, notably pharmacy and medication management. With MD as a part of its portfolio, technology-debt-ridden or not, Telstra would have a lot of the chips needed to win a lot of these contracts and to start connecting various parts of the system.
So perhaps $500 million is not so outrageous after all.
For GPs, both the price Telstra Health is prepared to pay, and that Telstra Health might own it, could hardly be bad, even if Telstra has in mind the “rule the world” platform aspirations within Australian healthcare that the global digital platforms have.
Apart from anything else, it will put a rocket under BP and Sonic to get on with the development of its cloud product, and alongside BP, most of the local medical software industry, legacy vendors and entrepreneurial new entries alike, will all probably be more valuable, and as a result be able to access funds to make the whole process of innovation go a lot faster.
Combined with the federal government’s determination to introduce a regime where providers and vendors will be forced in some way to move to far more interoperable cloud technology within about five years, the sale of MD to Telstra Health could constitute the starting gun on a whole new era of innovation in Australian healthcare.
Much of that innovation will be aimed at the gatekeepers of the most important information transactions in health moving forward: general practitioners.
Yay.


