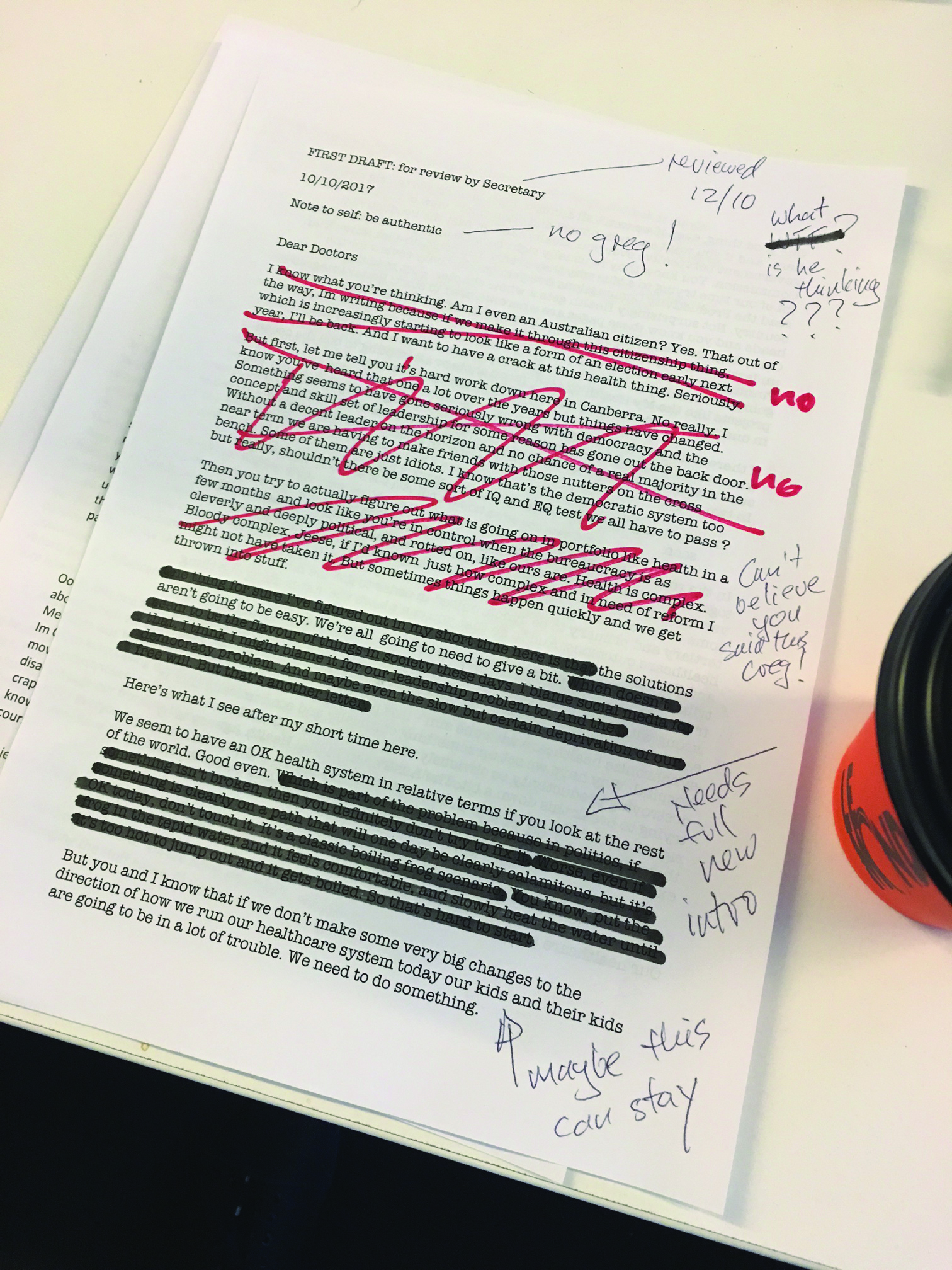
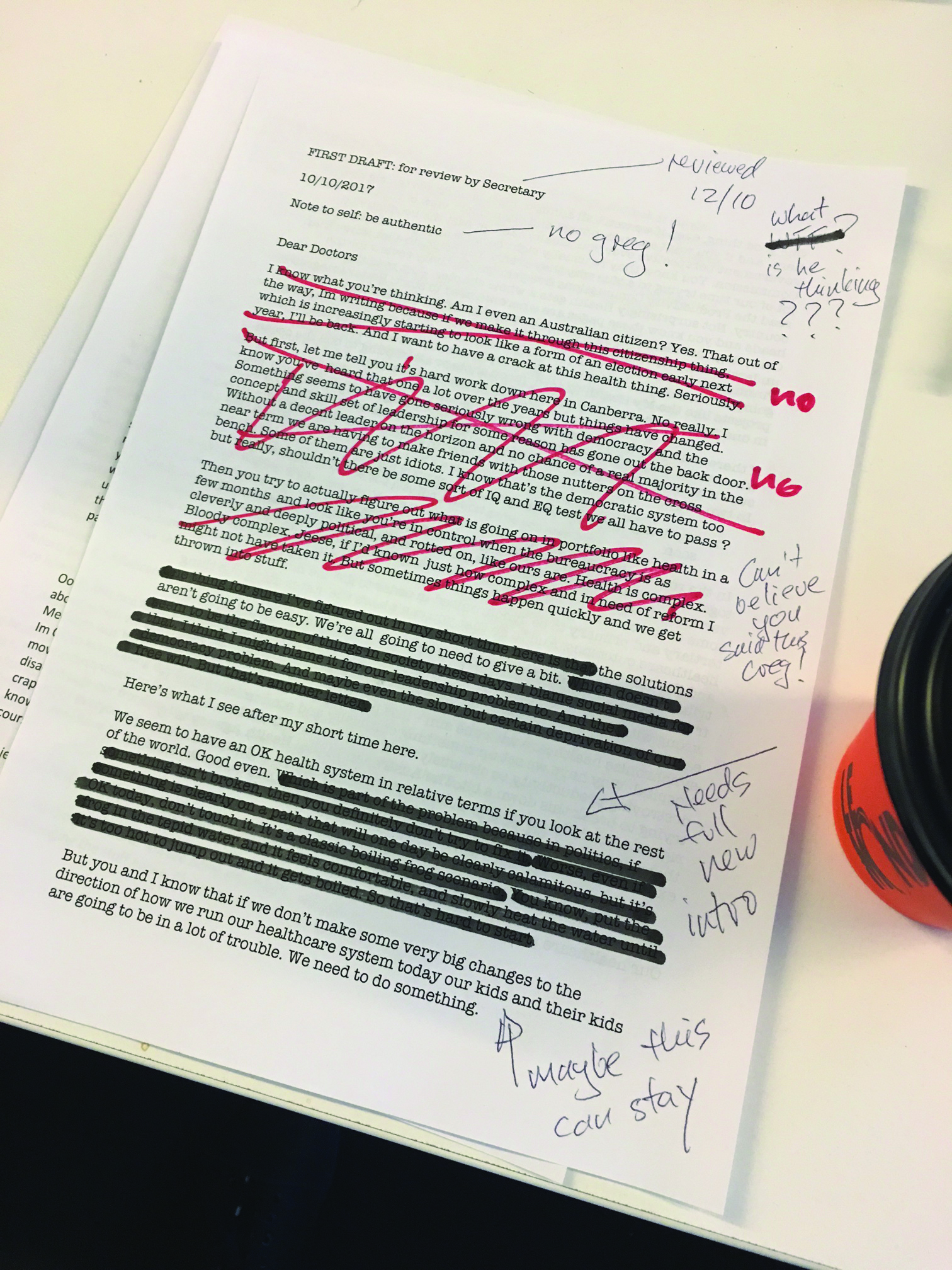
The Medical Republic is in possession of the first draft of Greg Hunt’s letter published in the MJA last week
The Medical Republic is in possession of the first draft of Greg Hunt’s letter published in the MJA last week and there’s been quite a bit of editing done.
Dear doctors,
I know what you’re thinking. Am I even an Australian citizen? Yes. With that out of the way, I’m writing because if this citizenship thing winds up forcing us to an election early next year, as it is increasingly looking like, I’ll be back. And I want to have a crack at this health thing. Seriously.
But first, let me tell you it’s hard work down here in Canberra. No really. I know you’ve heard that one a lot over the years, but things have changed. Something has gone with the concept of leadership. Without a chance of a proper majority in the near term, we are having to make friends with those nutters on the crossbench. I know that’s the democratic system, but really, shouldn’t there be some sort of IQ and EQ test we all have to pass?
Then you try to actually figure out what is going on in a portfolio like health in a few months and look like you’re in control when the bureaucracy is as cleverly and deeply political as ours is. Health is complex. Bloody complex. If I’d known just how complex and in need of reform our health system was, I might not have taken the job.
One thing I’ve figured out is that the solutions aren’t going to be easy. We’re all going to need to give a bit. Which doesn’t seem to be a popular concept in society these days. I blame social media for that. I think I might blame social media for our leadership problem, too. And the democracy problem. And maybe even the slow but certain deprivation of our free will. But that’s another letter.
Here’s what I see after my short time here.
We seem to have an OK health system in relative terms, if you look at the rest of the world. Good, even. Which is part of the problem, because in politics, if something isn’t broken, then you definitely don’t try to fix it.
Worse, even if something is clearly on a path that will one day be clearly calamitous, but it’s OK today, don’t touch it. It’s a classic boiling-frog scenario.
But you and I both know that if we don’t make some very big changes to how we run our healthcare system today, our kids and their kids are going to be in a lot of trouble.
One good thing, even if we won’t all admit it, most of us do see the big picture here. And if you want an open, honest and often smart view of the truth from a government perspective, you can’t go past the Productivity Commission.
You could do a lot worse than read the commission’s five-year productivity review. Health gets a whole chapter. Just read the sub-heads and you’ll know where we need to start: Better Integrated Care; Regional Flexibility is Critical; Funding Models are Problematic (LOL, understatement), Commit to Patient Centred Approach, Information Sharing is Pinning the Tail on the Donkey, and a few more. Most of it is in there, but I’m going to focus on just few of these topics, because, as we know from projects like the My Health Record, moon shots or attempting to boil the ocean, is not usually the best way to change the world.
If there were just four things we should and could change, what would they be? The “could” is the problem here, because I’m not really sure if we could change our funding system, but if we could, we definitely should.
1. Vertically integrate tertiary and primary care funding somehow – and soon
In the real world there aren’t two systems there is one, and it needs to work together, particularly in information sharing. If you want to see how a vertically integrated funding system can really work, go to the US and look at some of the better organised HMOs. You need all parts of the system – allied, tertiary and primary to be synchronised in order to get the most efficient healthcare outcomes.
And to do that you can’t have the states doing one thing and the commonwealth another. I have to say I’m a little shocked at just how tribal these two cultures seem to have become. These are all good people. We have set them against each other via a funding system when they should be working closely to synchronise healthcare with one aim – less people getting sick and going to hospital. Why then have we set up a system that is so obviously destroying productivity? Yes, with COAG and the like, we are trying to break this down a bit. The Australian Digital Health Agency is, by rights, a federally set up group, but reports to the states. But I’m afraid none of this goes far enough. We need to go further. I’m not sure how yet, but we have to examine it. And I will.
2. Move the primary sector to outcomes-based funding – properly
Our healthcare priorities have changed. That change is that we once needed a system skewed more to acute illness, but as our living standards have improved and our lifestyles become more affluent and sedentary, chronic health conditions are consuming more and more resources. Paying GPs using fee for service suited the old days. It doesn’t suit managing chronic health. GPs are the fulcrum of our healthcare system.
We need to sort out quickly how to pay them suitably for outcomes, not volume, and we need to do it in a way that doesn’t freak them out. We can excuse them for freaking out by the way, because, somewhat rudely, we haven’t given them a pay rise for the last few years and they have borne the brunt of that little budgetary trick. But it’s time to change things, and look at the GP profession for what it is. The cornerstone of our future of chronic care management, and likely the key to us eventually keeping system costs under control.
3. Data sharing might sound boring, but in a vertically integrated chronic care- focused system, it’s the sexiest thing about to happen
You can’t have an effective, outcomes-based, funding system, or any system full stop without good data. And frankly, the way we, in health, share data today, compared to say the finance sector is pretty bad. We all need to get a lot more active in changing what is a very fragmented and legacy-ridden system of sharing information. Our part is the Australian Digital Healthcare Agency (ADHA). I know what you’re thinking. You mean those show ponies who brought us the $1.2 billion NEHTA debacle? No, I don’t. Things are changing. The ADHA is not perfect I know, but it is there, and it is dedicated to this problem. But you can lead a horse to water, if you get my drift.
At the government level, this is one area where we are actually active and doing stuff. But we need more active engagement from not only grassroots GPs, but also the doctors and other parties that run the big private pathology, imaging and hospital companies. You know who you are. I know, and you know, that things have to change, even though it will mean a short-term profit issue for you. The system can’t become more efficient in sharing data without you. We get that this doesn’t actually add up for a private company.
However, 40% of secure messaging is pathology. And that 40% is a mess. And while you play the political game you aren’t yet seriously engaging in helping. If you were, you’d give up all your bespoke systems and let the system go open. We will try to bridge your market and profit issues if you work with us. Maybe we will even give you a break here or there on the MBS to help. Talk to us. We know we can’t just demand stuff – well, we can actually and if you don’t change we might start doing just that, which none of us really want – but we need more engagement from you. If the various commercial and private parts of our healthcare system can work closely with the public parts, just for this period of change, wouldn’t that be a good thing for us all? I love of bit community spirit, and I know you do too.
4. Medicare
There, I said it. It’ll be cut by the minders for sure, but I feel better for at least writing it in this first draft. The fact is, if you accept my second point above, which we all do behind closed doors, then Medicare as we know it, has to change. Medicare was born in the 1970s for good reasons. But it’s a fee for service insurance model. I’m OK to keep calling it Medicare if that makes us all feel good. But structurally, it has to move substantively to outcomes-based funding. And in a way that doesn’t disadvantage our frontline troops – GPs – or cause them undue stress. Sorry Bill, it might be politically clever to scare the crap out of everyone to win power, but you and I both know that Medicare has to move with the times. Some fee for service will remain in that model, of course.
Oh Jeez, the division bells are ringing, and Mal needs all hands on deck these days.
Please keep up the great work. You are doing great work. We will do our best to not set you up to fail by changing the stuff above. I know we all want the best. It’s a journey.
Please feel free to send me your thoughts. And I’ll get onto that letter to Mark Zuckerberg next month.
Yours sincerely
Greg Hunt (not)