The international language of SNOMED can make our data meaningful and precise without clinicians needing to change a thing.
When we think about health data what do we actually mean? Is health data words, or codes, or both, and who is it for?
Let’s start with words.
There is a scene in The Hobbit in which Bilbo Baggins says “Good morning” to Gandalf. Gandalf replies:
“What do you mean? Do you wish me a good morning, or mean that it is a good morning whether I want it or not? Or perhaps you mean to say that you feel good on this particular morning. Or are you simply stating that this is a morning to be good on?”
This is reminiscent of the unique challenges we face when we try to make sense of the words contained in health records. For those of us who deal with health data downstream, after clinicians and patients have gone home, we know well that the same meaning is often expressed with different words. And in the current context of pressured health budgets, no one can afford to waste time and resources pouring through records manually or calling clinicians to ask them what they meant.
Enter SNOMED-CT.
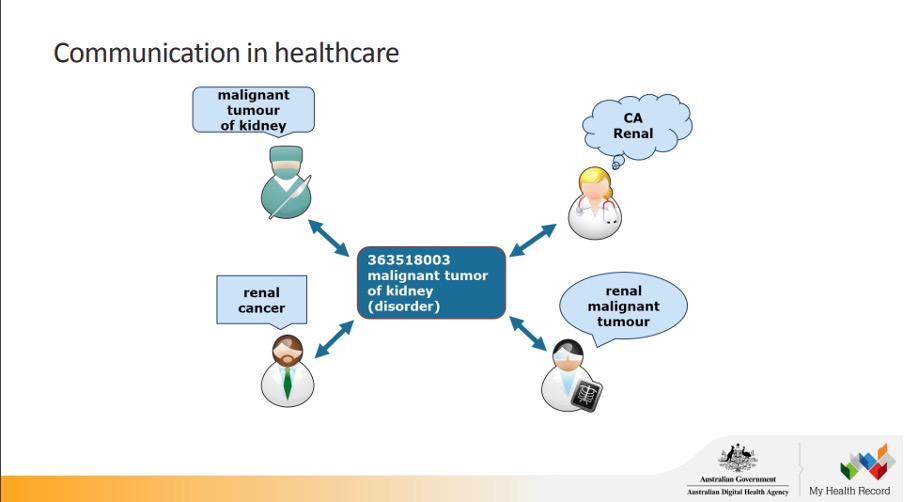
In the document library of the Australian Digital Health Agency, there is a very helpful resource for SNOMED-CT beginners, which includes the below slide, demonstrating how four different clinicians can all mean the same thing, but use different words to say it.
One of my colleagues frequently bemoans the fact that an orthopaedic surgeon he works for always uses different words and phrases to describe exactly the same procedures on patients who have exactly the same health profiles. As a data analyst, he finds this very frustrating because he needs to know exactly what the surgeon meant for each patient. He often tells me that usually, he’s got a pretty good idea of what the surgeon meant, having seen hundreds of his records over a long period, but he also knows that there is no place for guesswork in health data analytics.
Think about the word “cold” written in a health record. You can feel cold because someone left a window open and it’s snowing outside, you can have a cold, you can have a cold personality, and in a respiratory setting, a clinician may have used “cold” an acronym for “chronic obstructive lung disease”. SNOMED-CT has different codes for all of these meanings of “cold”, and more. It is the international language of health that provides meaning, and therefore has very wide utility.
Standing in the shoes of the health data analyst for a moment, it is easy to appreciate his frustration, because he can never make the mistake of mixing the data of a patient who needs to put a jumper on with one who has a serious respiratory illness. Precision is key.
From your perspective as clinicians, you probably often use different words to describe the same things that you see and do in clinical practice. This is usual clinician behaviour all over the world. We know that it is usually unconscious, or maybe clinicians just like to mix things up a bit.
Here in Australia, it is unfortunately also very likely that clinicians are partially driven to describe the same thing myriad different ways because of the need to mitigate ridiculous PSR processes that require you to particularise your templates for every patient, or risk repaying hundreds of thousands of dollars.
Some of you may also have heard about the global “clinical documentation improvement” mission. While it is certainly true that improvements can and should be made in the way clinicians record what they do, in modern, data-driven health systems, we really need to focus on allowing clinicians to record things in whatever way works for them, and then get out of their way so they can practise medicine more and worry about records less.
Ultimately, the words that populate medical records are of great importance only to clinicians and patients, both of whom can read, understand, and discuss their contents. But for the purposes of public health initiatives, codes are king, and to enable us to code well, it is enormously helpful if the words are in the right place.
Clinicians regularly put information in the wrong places in EMRs. This can be everything from putting mobile phone numbers into Medicare number data fields, to writing a War and Peace-size entry in the principal diagnosis data field. This is why the world is shifting to the standardised health information model known as openEHR, and good EMRs now make it easier and more intuitive for clinicians to insert text in the right place. Additionally, atoms of data rather than huge swathes of text are the direction the world is heading in, which of course will also enable secure messaging and interoperability.
Interestingly, in Australia, a side benefit of these new global standards (assuming we adopt them at some point) will be that Medicare’s “adequate and contemporaneous records” standard will become an anachronism.
The elephant in the room in all of this is of course the issue of MBS codes and what we plan to do with them. My research found that MBS codes are actually bedrock data, central to the operation of the entire Australian health system, and letting them go will be neither quick nor easy. So, a better approach will be to gracefully integrate the MBS into Australia’s overarching digital health strategy, which is underpinned by SNOMED-CT. What a coincidence!
The sooner we prioritise adoption of international standards and leverage Australia’s huge investment in SNOMED-CT, the sooner we can set our health system on the right reform path.
Dr Margaret Faux is a health system administrator, lawyer and registered nurse with a PhD in Medicare compliance, and is the CEO of AIMAC, which offers courses and explainers on legally correct Medicare billing.


