In a series of articles, a lawyer who spent years researching this behemoth subject will explain what’s wrong and how to fix it.
It had been obvious to me for many years that there was a growing problem with Medicare that no one was talking about – it was the antithesis of rorting and more nuanced than the media could understand.
I had been administering Australian medical billing since Medicare began, had worked in the system as a registered nurse, and by 2012 I was a lawyer, and had had one too many conversations seeking clarity on some important aspect of Medicare billing law that no one could answer – including Medicare.
The doctors I did billing for believed the system was straightforward. For them it was just a matter of, well, here’s the item number, just get it paid.
But as an administrator with legal qualifications, I found medical billing anything but straightforward and spent hours trying to explain to doctors the important details and considerations involved when spending public money.
So in 2012, when the Medical Journal of Australia published an opinion piece by the former director of the PSR, alleging doctors were rorting Medicare to the tune of $2-3 billion per annum, a simmering sense of disquiet within me was piqued. The article not only attracted intense media coverage, but it also made me angry about what I perceived to be a sea of misconception. That was the day I picked up the phone, called my alma mater and began a PhD on Medicare claiming and compliance.
Public debate in this important area had for decades been dominated by health economists who had no clinical experience or knowledge, and doctors who had no understanding of economics. The people in the middle, who actually administered the Medicare scheme (medical receptionists and variously named medical billing and claims administrators), had no voice.
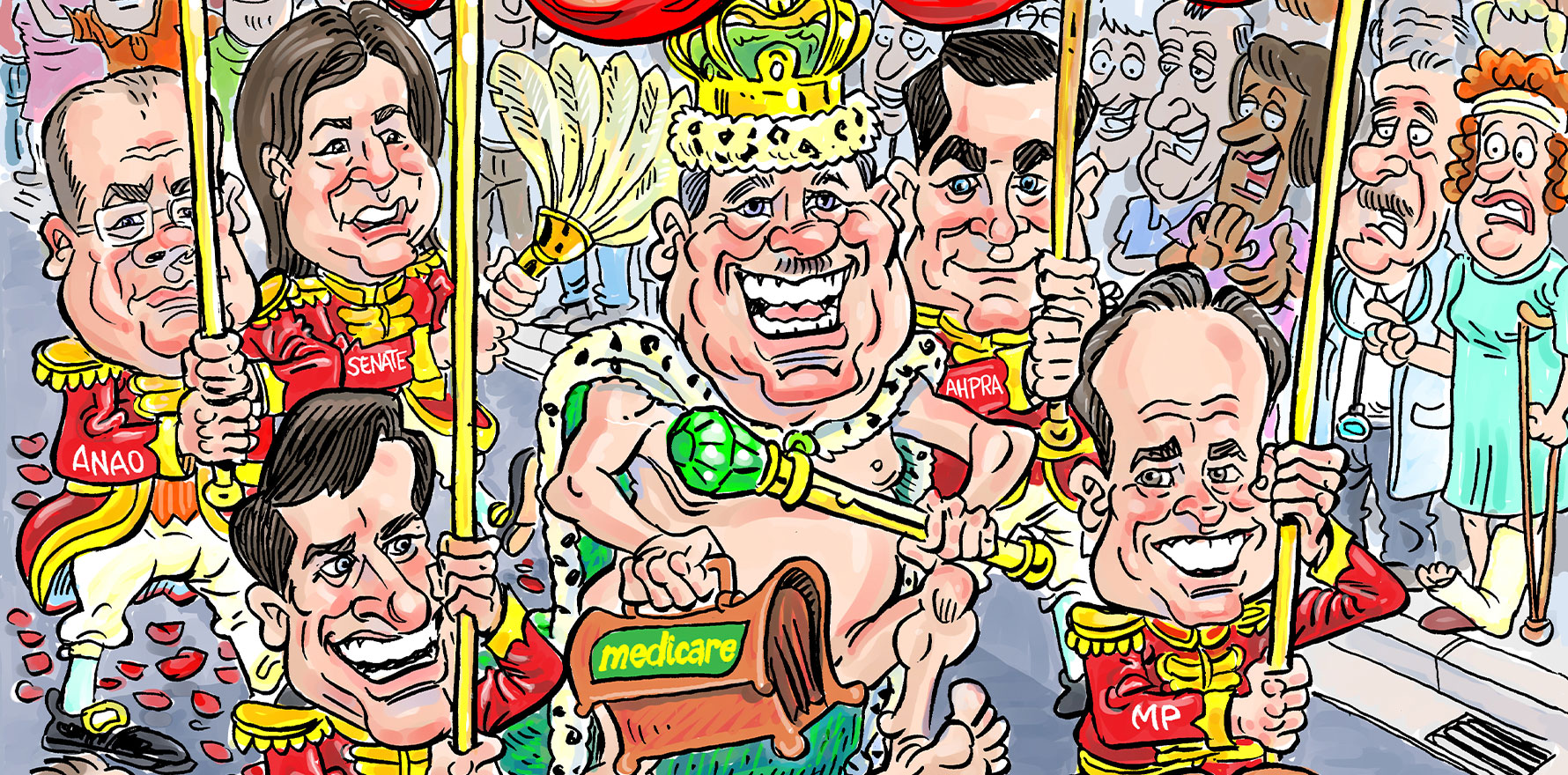
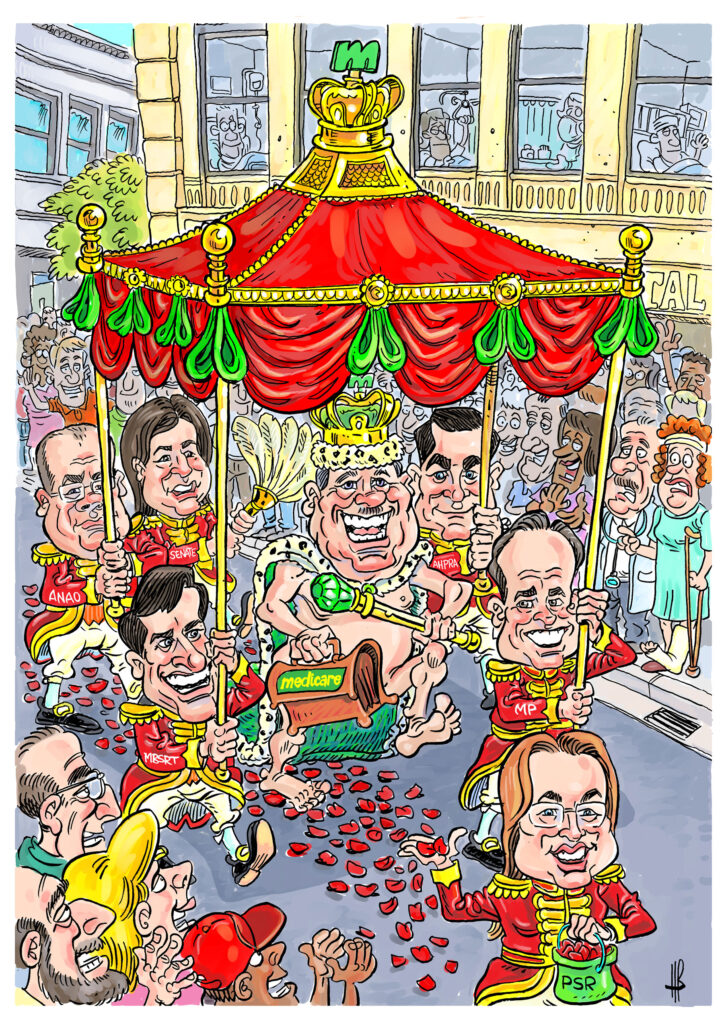
I felt we had become incapable of having the conversations we needed to have about problems within Medicare, because we were stuck in a binary time warp. Doctors were saying the system was easy to navigate, which led health economists and others to the view that all non-compliance must therefore be deliberate. Meanwhile, the government’s line around Medicare compliance was “We’ve got this!” The narrative had become like a rusted-on Medicare version of The Emperor’s New Clothes, with collective denial about the facts in front of us, because the truth was that they were all wrong, and the Medicare billing system was broken.
Eight years later, my journey has drawn to a close. There are just a few administrative matters between me and a doctorate, and it will be an honour to share my research findings with you in forthcoming articles.
The nuts and bolts of it are:
- Medical billing is profoundly complex.
- There are major problems with doctors’ understanding of billing.
- There is no education or reliable support for doctors around billing.
- The root causes of billing non-compliance are rule-of-law problems.
- Government oversight of compliance and current policing strategies are ineffective.
- Recent reform of Medicare may have exacerbated compliance problems.
- Education will be a critical component of future solutions, though no one currently has clear responsibility for education.
- Education alone will not improve billing compliance and a national curriculum cannot be introduced until rule-of-law problems are first addressed.
The research concluded that a principal cause of non-compliant medical billing in Australia is system issues rather than deliberate abuse by doctors. Without reform, the government can expect no improvement in non-compliance and increased litigation against the PSR by doctors, who have no choice but to try and comply with an incomprehensible system that they do not understand and feel powerless to change. Consumer out-of-pocket medical expenses will likely continue to rise as doctors shift the cost burden to their patients, which may in turn accelerate contraction of the private health insurance market. An urgent correction to Medicare’s billing system infrastructure is required, encompassing regulatory, educational, and digital reform.
In this series of regular articles for TMR‘s Money & Medicine, I am looking forward to sharing not only my research findings, but also a blueprint, with 27 evidence-based recommendations for reform, which are designed to rescue and modernise Medicare – which I believe is a masterpiece worth preserving.
Margaret Faux is the CEO of AIMAC, which offers training courses and explainers on legally correct Medicare billing.