If Senator Hollie Hughes is any indication of Liberal Party attitudes towards GPs into the future, you might have to vote Labor.
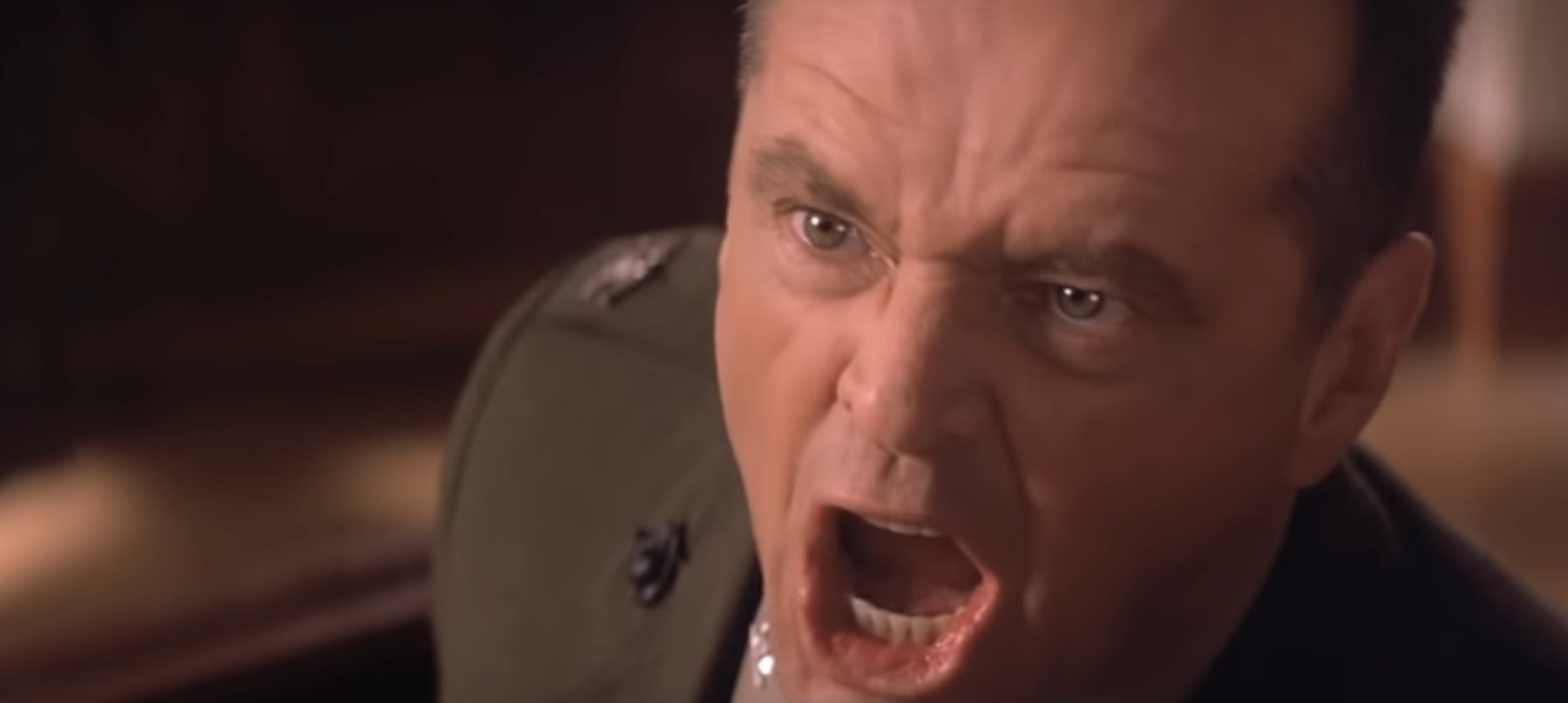
If you didn’t catch any of the backwards and forwards between Liberal Senator Hollie Hughes and various witnesses to this week’s Senate hearings into GP services in non-metro areas, it’s worth having a quick look at some of things she said and in what context.
The Senate Committee heard 54 witnesses Monday in Melbourne, and Senator Hughes either asked questions, made statements, or interjected a total of 85 times.
Most of the time Senator Hughes was having a go at the witnesses for one thing or another, sometimes with quite specifically directed vitriol.
We looked at all of her interactions and over 90% were negative in some way or another, mostly in the manner of suggesting that outer metropolitan GPs in Melbourne and some related professionals were whingers, seeking special provisions for better recruitment options for their staff and reimbursement rates (per more remote locations), without reasonable argument.
Senator Hughes is a longtime and staunch defender of remote rural communities and their resourcing, having lived most of her life in the country (she now lives in Sydney, which she needed to do to secure a Senate seat).
During the hearing she often cited how hard much harder it was for more remote locations such as Whyalla, when she was giving it to some of the witnesses. Most of them were trying to explain to the hearing that in outer metro, where practices were once rated for DPA or DWS and then rerated to be only MM2, life had become significantly more difficult as they couldn’t recruit doctors to work for them.
Following are some selections in exchanges of witnesses, chair and Senator Huges to give you a feel of what she was dishing out.
In response to evidence from Australian Medical Students Association (AMSA) President Jasmine Davis, on doctor burnout:
Senator HUGHES: We heard just before lunch from people who are 10 minutes outside the CBD and want to get a certain classification that equates them to a rural and remote area, which I find absolutely offensive. I’m sorry. I do. As someone…
CHAIR: I find it offensive that you are referring to them in that way.
Senator HUGHES: I do find it offensive that someone who is 10 minutes out of a CBD wants to be considered the same as someone who lives 3½ hours from a regional centre. It is absolutely unacceptable to those people that live in rural and regional Australia, because they have very limited access to anything. If they get in an accident, they don’t have a helicopter ride or a short ride down the freeway to major medical facilities. They have zero access to anything …
CHAIR: Do you have a question, Senator Hughes?
Senator HUGHES: I just find this whole thing to be completely self-serving. You’re sitting here telling us that government needs to solve the problem because GPs are burnt out. How do you think restaurateurs feel? How do you think businesses and small businesses feel? They have had exactly the same sorts of issues through covid. Yet we’re travelling around the country listening to complaints from people who earn hundreds of thousands of dollars a year, who are quite often the highest-paid people in country towns, and yet expect the government to further incentivise them. How is that fair to every other Australian taxpayer?
In response to evidence from several witnesses who were trying to explain that after being reclassified as MM2, and losing access to IMGs for recruitment, and other incentives for doctors to work with them, their clinics were unable to meet the demand of the outer suburbs of Melbourne, where most of the patients can’t afford mixed billing, and many have very complex chronic illness issues:
Senator HUGHES: We were in Whyalla last week, which is very remote and not within a commutable distance from Melbourne. You’ve just had a clinic open next door that’s got GPs in it, which is obviously able to then cater for additional patients. I’m just trying to understand your situation versus Whyalla where, if you have a car accident it’s the luck of the draw if there’s a doctor within 400km of you at all. And those doctors are talking about burnout because they’re on call 24/7 for a number of towns. They’re delivering babies and reacting to accidents as well as general GP duties. I don’t feel like we’re comparing apples with apples here [no you aren’t, Senator Hughes, that’s the problem with your rant]; it’s a very different situation. I’m trying to understand: if there are four doctors who have set up a bulk-billing clinic next door to you, is it really a problem recruiting doctors to the area; or are there issues around how clinics are being set up and run?
Ms Whatley: I guess you could say, “Sure, it’s not apples with apples or oranges with oranges.” I think there is a context that needs to be considered in terms of, “Sure, we’re not delivering babies, on call for hospitals and doing after hours locum work for nursing homes” and things like that. However, we are also doing a lot of the frontline work. We are immunising Victorians. We’re having to refer off to testing clinics. We’re doing all those extra things on top of that that I think sometimes …
Senator HUGHES: And more GP activities because these GPs were doing the same sort of work as well as the other work on top of that. We’re looking for solutions, and you’ve got to think that it’s easier to get someone to drive 40km from Melbourne than it is to drive 450km from Adelaide to take up a position. Is it really GP numbers? Is it?
Senator O’NEILL: [sarcastically] Or they’re just lazy.
Senator HUGHES: I’m not saying they’re lazy.
Senator O’NEILL: They’re just lazy doctors; that’s the problem?
Senator HUGHES: No, I’m just trying to understand because when we spoke to people in Whyalla last week one of the questions was: is there a shortage of doctors coming through medical schools? And we were emphatically told: “No, that’s not the issue.” So, what is the issue? If there are plenty of GPs going round but they won’t go 50km out of Melbourne, how are we going to get them to go 450km out of Adelaide?
Ms Whatley: I guess that’s why we’re here.
Senator HUGHES: That’s what I’m trying to understand. If you are having this kind of issue and you’ve got a clinic that’s set up next door, is it servicing the population or is it just the GPs – what is it? Is it the expectation that GPs get going through medical school that they don’t want to go into general practice? I’m trying to understand: are they better off staying in Melbourne and becoming cardiologists, immunologists or whatever, rather than going into general practice whether it’s in Toorak, Langwarrin or Whyalla? What is the issue here?
Trying to compare Whyalla with outer metropolitan Melbourne, to make a point around outer metro GPs being out of touch and whingeing, and, introducing the idea that GPs should allow pharmacists to do more of their work (edited):
Senator HUGHES: This is a question I asked GPs out in Whyalla last week. One of the things that the RACGP has opposed and vehemently opposed was the allowance of the Pharmacy Guild and pharmacists to deliver immunisation. They’ve vehemently opposed things like pharmacies and pharmacists being able to reissue prescriptions for things like the contraceptive pill, which obviously then increases the burden on GPs if you’re talking about having to deliver immunisations when, clearly, pharmacies were prepared and able to do that. Also they are prepared and able to do things like renew contraceptive pill prescriptions without a doctor’s appointment. But it is the RACGP that continually opposes pharmacies being able to provide these services. Do you think that in rural, remote and MM2 areas, if pharmacies were allowed to provide these services and weren’t opposed by the RACGP at every opportunity, that actually might relieve the pressure on GPs in some of these areas, that they wouldn’t be having to see patients to renew a contraceptive pill prescription and wouldn’t be seeing patients to give them an immunisation, because they could get it at the chemist?
Ms Whatley: You’d probably have to ask pharmacies and things like that …
Senator HUGHES: Pharmacies are very happy to do it. I know pharmacies are very happy to do it. It’s the RACGP that opposes it.
Ms Whatley: I can’t talk for the RACGP. I can only talk for Langwarrin clinic.
Senator HUGHES: Would it ease the pressure on your doctors if they didn’t have to see those patients? Would it ease up the pressure on your books?
Ms Whatley: It is hard to say because at the moment they are providing some of the vaccines. They do take up doing some of the flu vaccines and whatnot. However, the pharmacy and the shopping centre next door are providing every single type of covid vaccine. That has not relieved the pressure on us and has not alleviated any of our waiting lists whatsoever. We still have a waiting list running, and we’ve been doing it since last year.
Senator HUGHES: Do you have nurses who deliver the vaccines?
Ms Whatley: Yes.
Senator HUGHES: So there are nurses?
Senator O’NEILL: We’ve been talking about the challenges faced by people here. We’ve heard about doctors collapsing, in terms of their mental health and inability to be able to do the job, because they’re under incredible pressure. We have locals telling us they can’t get in to doctors. We’ve got people here basically comparing salaried doctors, who get a solid income in the hospital, with the compassionate doctors, who are willing to cross-subsidise their own patients’ care. This is a broken model …
In response to a practice manager from an MM2 area who was struggling to get GPs into their clinic:
Senator HUGHES: The GP services per capita of 7.6 is higher than the MM2 average of 6.5. So you’re actually in an area that is serviced more highly than the average MM2 area. I’m just trying to understand – and I appreciate you might not have perfect systems. Why do you become a priority when you have more GPs than any other MM2 area while I have an area in another rural and regional area with one GP doing 24/7 care?
Ms Wilk: Senator Hughes, I’m really glad you raised this because I have a clinic with 6000 patients and – once again I’m going to reiterate – one doctor. There are other clinics around me that have more doctors, bless them. They’re lucky, they’re fortunate. Let them retain them. But I can only talk of my clinic and my patient load. You’re saying that there is a number of doctors in those areas. I don’t know, to be quite honest, how accurate your figures are. I know of two clinics around me that have had to close because they didn’t have doctors. They shut their doors.
Senator HUGHES: That is something doctors need to take on board – that if they want these problems solved, take some responsibility for themselves. If we are going to get the right information, perhaps we need to talk about, not just what the government does but some personal responsibility from the profession. You can’t come to the government and say ‘We don’t have as many doctors as we think there are,’ if you guys don’t take any responsibility.
Senator O’Neill interjecting –
CHAIR: I would like to hear from the witnesses, please. Senator O’Neill and Senator Hughes, could we have some quiet, please?
We will leave it there as far as excerpts and Senator Hughes go, but there’s quite a bit more, most of it along these lines.
It’s a little bit surprising that the Liberal Party, in the run-up to an election, is OK with what Senator Hughes is saying at these hearings.
After all, even if she thought these things were true, as a politician, where’s the political upside in laying into a series of GPs, practices managers and allied health professionals, all of whom are clearly working in what has developed into a series of “ghost zones” as far as federal health policy is concerned.
Around 2017 and onwards, the Department of Health, seeking system savings, reclassified a lot of outer metro areas in the country to MM2, and denied them a capability to staff themselves properly to meet what are very real increases in population and complexity of patient cases.
This is not to say MM3 and outwards isn’t in big trouble as well. It is.
But what Senator Hughes bypasses entirely in her stance is that in these “ghost zones” we have a big and rapidly growing segment of our patient population that are largely low income, have very complex chronic care challenges and are being denied proper care because of budget decisions a few years back on the part of the DoH.
Senator Hughes’ argument, that more remote regions are in much more dire need, might be right sometimes, but on a patient population basis, many MM2 areas, especially those ones which were reclassified in the last few years, are in crisis, and it is likely that on a per-patient basis, funding some of these MM2 areas through reclassification back to DPA might provide a much better overall return to the system.
All the witnesses in this hearing had horror stories of trying to make ends meet in outer metro. It was hard to hear.
But Senator Hughes wasn’t buying any of it.
Her performance has established her as a poster child of Canberra politicians who think most doctors are rich professionals who do a lot of whingeing, given that most of their income is from the public purse.
It’s a bit weird though, as her performance from any political viewpoint doesn’t make any sense in the runup to an election.
GPs don’t have huge political clout unfortunately (they find it very hard to sway their patients on much politically), but they do all vote.
It’s hard to imagine that Greg Hunt, even though he is leaving the building after this election, would be cheering Senator Hughes on.
As a prominent Liberal senator, she’s not really helping the cause, especially when the Labor senator on the same Senate committee was constantly expressing empathy and compassion for the outer metro GPs and allied professionals.
What is the upside in being so aggressive and insulting to the profession?
What Senator Hughes displayed this week isn’t usual in a public forum.
Most politicians are smart enough not to say exactly what they think.
Unfortunately, however, a lot of politicians and a lot of public servants, do think along the lines of what Senator Hughes was saying this week.
Which is whose problem precisely?
Although you could make an argument that Senator Hughes is wilfully being ignorant, and she should look at herself in the mirror a little more, the buck for brand GP stops with GPs.
It’s not an easy brand to position for a few reasons, so it’s not simply that the RACGP, the AMA and ACRRM have never got it right in representing the profession in Canberra.
For starters, GPs (and specialists to a degree, although at least they are generally much better paid) tend to suffer from the fact that they make income from people’s health or rather ill health.
For generations, surveys that compare tobacco companies with pharmaceutical companies, have tobacco companies coming out on top.
That feels counterintuitive given that tobacco companies knowingly kill millions of people each year, and pharmaceutical companies, albeit they often do not behave very well, do manage to save millions through their products.
The problem the public has with pharmaceutical companies is that they profit from people being sick.
Doctors cop this effect to some extent.
Behind closed doors you hear a lot of politicians laying into doctors for being rich and complaining about their work conditions. But you hardly ever hear one laying into a lawyer or accountant for the same thing. Even bankers, noting that they were all dragged kicking and screaming to the Banking Royal Commission.
Doctors also are largely on the public payroll, which lawyers, bankers and accountants aren’t. So that’s another level of constant scrutiny.
If you’re shocked by Senator Hughes’ attacks on doctors she probably isn’t an outlier as far as politicians and attitudes towards doctors go.
Which is why GPs shouldn’t have been surprised by the Medicare freezes, and shouldn’t be surprised that they’re not likely due for a pay rise in the minds of the politicians for a long time to come.
If you read all 81 pages of Mondays hearings, it’s very hard not to feel for the outer metro GP and allied health witnesses. Most are committed and delivering care despite the system, at quite a bit of personal cost.
Giving evidence this week Ms Tegan Whatley, a practice Practice Manager at Langwarrin Medical Clinic told the hearing, “I’ve only been at Langwarrin for a short period, after working in health care for several years. When I interviewed for the position, there were nine GPs, mostly part time. By the time I got here, three weeks later, to actually take the job, they were down to three and barely floating, for lack of a better description. It got to a point where they were paying rent, consumables—all those extra things—out of their own pockets, not just out of their percentages, which they usually pay to the clinic. The problem is that, if those three GPs hadn’t been willing to pay out of their own pockets and subsidise in the meantime, we would have shut.We’ve had days where we have shut the doors and just said, ‘We don’t have anybody today.’ What that then means, obviously, for the ongoing care for the patients is: (1) we can’t offer any appointments; and (2) we can’t offer consistent care to those with chronic conditions or complex health issues. I was explaining before that we have a three-day wait for a male GP for our existing patients—not new families or anyone who had moved down this way during the pandemic—and a seven-day for a female GP. So the need is there, but we can’t provide the service. That’s basically it.”
The pollies will argue that telehealth is one giant pay rise that demonstrates Canberra’s commitment to general practice.
But it isn’t.
Without telehealth, the healthcare system would have disintegrated during covid.
And once we had telehealth, it was clear that the overall return to the system made it worth keeping, and without it, the general practice network might fold in the face of any further covid stress.
Telehealth is not about rewarding GPs for their hard work and commitment to their patient communities during covid.
The RACGP president, Dr Karen Price, recently publicly stated that GPs will need to start upping the ante on mixed billing if they are going to make ends meet, saying that she didn’t think that Canberra was ever really going to return to reasonable indexing of the MBS for GPs.
This week we saw iconic GP and past AMA president Dr Mukesh Haikerwal break ranks and write publicly (in Australian Doctor) about why he is walking away from bulk-billing.
We’ve published a few similar articles from GPs walking away from what the government is pushing as the beating heart of the system.
Brand doctor and brand GP are never going to be easy gigs, given the dynamics of health and politics, but one thing for sure is that as long as GPs are beholden to bulk-billing, they aren’t going to make ends meet far into the future. This is especially so if you’re following the payroll tax stories on medical practices and the likely significant compliance costs most practices are going to need to fork out to survive.
Outside of breaking the government Medicare chains by (sensibly) abandoning bulk-billing, one thing that might help a little is if the AMA, the RACGP and ACRRM could get together and develop ethical and clinical standards that applied across the whole profession.
At the moment, it’s easy to pick off the profession with nonsensical comparisons, like the one Senator Hughes made this week when she attempted to compare how Whyalla should work for GPs and patients compared with how outer metropolitan Melbourne should work.
With clinical and ethical standards, developed and maintained by doctors, we’d have some units of measurement by which doctors could defend themselves and their performance better in Canberra (financial, and clinical).
Such standards would also likely work to level the income playing field to some degree between specialists and GPs. That’s another story though.