Fewer infections over the last two years possibly means less "natural immunity" when these respiratory diseases return.
Public health measures to control covid, including social distancing, masks, border closures and reduced international travel, have worked to reduce the impact of covid.
But they’ve also led to a reduction, or changed the pattern, of other respiratory infections such as influenza, whooping cough and respiratory syncytial virus (RSV).
A Productivity Commission report released last month showed whooping cough rates in 2020–21 were the lowest they’d been in years.
Australia also didn’t experience much of a flu season in 2020 or 2021. This is good news as we didn’t want to have both flu and covid circulating in high numbers.
One concern, though, is these low rates may have lulled us into complacency. It might mean many people haven’t been in any rush to get their flu vaccine.
What’s more, because very few of us have had these infections over the past two years, we have probably experienced less of a boost in any “natural” immunity.
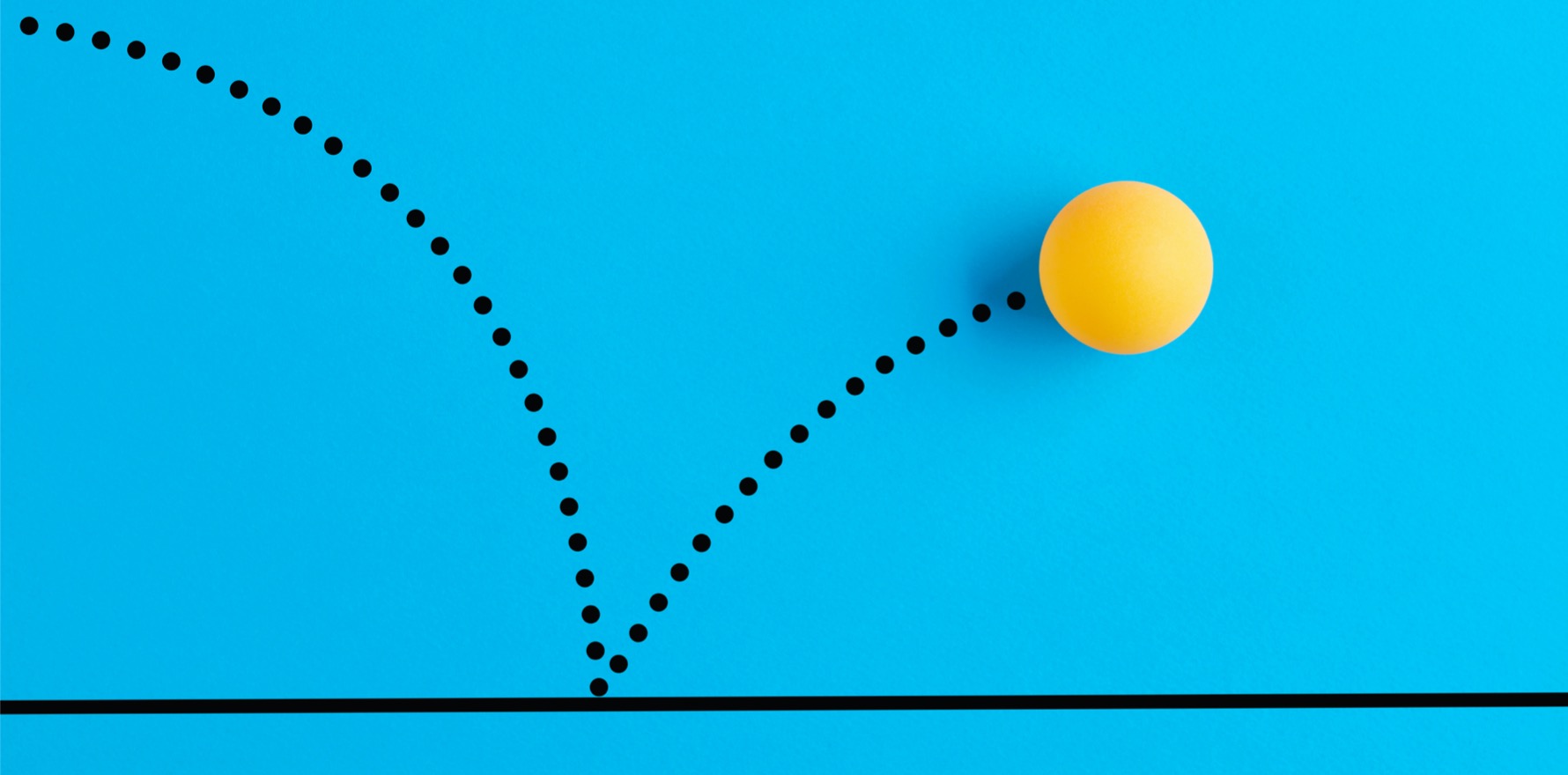
We need to be wary of these infections bouncing back, especially as we head into winter and our borders open to international travellers.
The Australian Technical Advisory Group on Immunisation (ATAGI) last week released advice urging all Australians to get a flu vaccine once available, which is likely to be in March.
Flu rates are way down
Influenza activity is tracked at a global level by the World Health Organisation and used to decide on which flu strains are covered in the vaccine each year.
In Australia it is a “notifiable disease”. This means laboratory-confirmed cases are reported to our National Notifiable Diseases Surveillance System.
In 2020, there were 21,266 notifications of laboratory-confirmed influenza to this system — almost eight times lower than the five-year average, which is 163,015.
In 2021, there were only 598 notifications up to early November.
It’s important to note some of the reduction in flu cases being notified could be due to fewer people presenting to health-care centres and being tested. This means we may undercount flu cases, especially mild ones.
However, we have also seen a reduction in more severe cases leading to hospitalisations and deaths due to flu, suggesting it’s a real decrease.
With all the focus on COVID I actually forgot it’s been more than a year since I had the sniffles ? https://t.co/7m87VzuR3L
— Nick Hose (@NickHose) September 16, 2021
Whooping cough is down too
Whooping cough (also called pertussis) is at historically low levels.
We usually experience an upsurge in whooping cough cases every three to five years. This is probably because we get a natural immune boost after exposure, which then tends to limit the spread and so the epidemic ends, however when our natural immune boost wanes we may then get an increase in cases.
It’s also a “notifiable disease”.
Our last big year was 2015–16, and if we followed the normal pattern we should have seen an increase in 2020–21.
In previous years, notifications of whooping cough have been over 100 per 100,000 children, with the highest rates of 287 per 100,000 in 2015–16 and 357 per 100,000 in 2011–12.
But in 2020–21 there were only 116 cases notified in children under 14 years old. That’s a rate of 2.4 per 100,000 children, substantially lower than 2011–12 and 2015–16.
RSV has changed
Respiratory syncytial virus (RSV) is a common viral infection that usually leads to an increase in hospitalisations every year, often before the arrival of flu. It can be particularly severe in infants under one year old.
The covid pandemic and associated public health measures may be behind a shift in the timing of RSV infections.
In NSW from 2015 to 2019, the peak of infections was in autumn and winter. But in 2020, the peak of infections shifted to early summer.
In 2020, RSV hospitalisations were lower in infants under 12 months and higher in two to four year olds, compared to previous years (2014–19).
Vaccines are important for other diseases, too
The reduction in flu, RSV and whooping cough is likely due to covid public health measures.
However, for whooping cough, the protection of our youngest infants is probably also due to the impact of maternal whooping cough vaccines during pregnancy.
We don’t have much data on this yet, but one paper from Victoria showed an increase in whooping cough vaccine uptake among pregnant women. It climbed from about 38% to over 80% between 2015 and 2017. Another paper from southeast Queensland showed whooping cough vaccine coverage in pregnant women was approximately 70%.
Real world effectiveness studies have shown a whooping cough vaccine during pregnancy is more than 90% effective in preventing young infant hospitalisations from the disease.
For this reason, health authorities in Australia, the US and UK recommend a whooping cough vaccine be given during every pregnancy.
Australian health authorities also recommend pregnant women get flu and covid vaccines.
We can’t be complacent
Concerns about visiting health-care providers during covid may have meant a fall in vaccine coverage for other diseases. This has occurred in some countries and has prompted an alert from the World Health Organization.
Also, it’s clear fewer people have been naturally exposed to flu in the last two years. It’s possible having a flu infection in one year may give you some protection in subsequent years (though you really don’t want to get the flu).
Both of these factors may mean we have lower protection when we finally get a flu season.
With winter approaching and borders opening up, it’s possible we may see the emergence of flu again this year.
In the meantime talk to your GP about any vaccines – including flu when it’s available – that you and your children may need to catch up on.
Nicholas Wood, associate professor, Discipline of Childhood and Adolescent Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.