The next president of the RACGP will be the most important in the history of the profession, if you choose the right candidate.
Despite the minor complication that I’m not able to vote in the RACGP presidential election, I’m going to try to sway how you think about your vote.
I’m also going to have a go at getting some of those GPs who never vote – only 11% of eligible members voted in 2020 and 15% in 2022, which is a problem – to maybe reconsider their disinterested, or possibly cynical, positions on the college, and think about voting this time around, given the probable critical nature of the next two years for the profession.
In attempting all this I’m going to make a few assumptions:
- That you think it is the role of the president of the RACGP to create the right cultural, political and regulatory settings for the profession to flourish into the future;
- That you think the current trajectory of the profession isn’t where it needs to be;
- That you think if you pick the right person they will be empowered enough in various ways to be able to create conditions for change.
There is a school of thinking that says the RACGP should mainly be concerned with what it was originally created for – training, education and governance – and as such it should keep its head out of advocacy and politics.
I’m going to note here that the new CEO of the college – who you never hear from these days because the college board decided the CEO should not have any public profile at all – is a consummate training, education and governance professional. That would make it much easier for a president to be the spearhead of advocacy for the profession (ie, the core of the college function is in good hands) should a president choose to concentrate their efforts in this manner.
I also note while RACGP presidents are significantly handicapped in being able to achieve any of the above by the poor governance surrounding their role, some have achieved a lot in their short tenure in the past, regardless.
If you accept these assumptions, start by asking yourself – if your new president could only do one thing to change the trajectory of the profession the way you think it should be heading, what do you think that one thing would be?
This isn’t a very easy question to answer.
I wish the college had required each candidate to answer this question as the first part of their statements.
But they didn’t.
So if you start by reading their statements you are going to get lost almost immediately in a lot of detail and motherhood type promises (the statements are all HERE).
Detail is important. It’s just that clarity of purpose should always be at the forefront of such detail if you are going to take constituents on a journey with you, and nearly all the statements aren’t that clear on purpose.
“Make America Great Again Again”, is current example of clarity of purpose.
Unfortunately, it is one with virtually no substantive supporting detail, evidence or plans to achieve the stated purpose, which is potentially a relevant problem already in the RACGP election statements.
If you manage to whittle a candidate’s statement down to what you think their single purpose might be, you’re going to then want to see if any of the accompanying detail constitutes any plans that are actually doable.
If you read all the candidates’ statements and you’ve voted before in the RACGP election, the first thing you are going to notice is quite a few usual-suspect motherhood promises and initiatives that might sound good to say out loud in a campaign, but for which there has been no meaningful plan or path to achieve in the past and probably therefore won’t be one in the future either.
For example:
“Maintain GPs as the central role in patient care – and work with governments to have all practitioners working top of scope.”
Or,
“… create new Medicare item numbers and raise reimbursements for existing ones that are currently undervalued.”
Nice things to state but naively generic without proper consideration as to the machinations of politics and process needed to move the dial on the ideas.
There is a lot of this in all the candidate statements and it makes for a significant amount of noise.
I went through all the statements with a red marker, crossing out everything that was aspirationally naïve, a motherhood statement, a nice thought but entirely impractical to achieve in a two-year presidency or lacking entirely in a plan to achieve it, weirdly detailed and at times irrelevant to the point of no relevance to the bigger question of the future of general practice, and stuff that I just didn’t get.
At the end, there was only about 10-15% left in all the material to think seriously about.
I am a bit of a hard marker though.
At this point I did wonder if this might be the problem for the college and the profession.
What does it say if most of the presidential candidates of the most powerful institution in the profession can’t be reasonably succinct on what is wrong and provide a realistic structured plan to address that wrong?
It’s not all bad.
But in the light of what we have so far (I’m hoping clearer ideas and plans emerge as we go along) I am recommending you start your consideration at a different point to the candidate statements: that one thing you want a president to achieve.
And then work backwards.
As you are doing this, try to keep in mind the following if you can:
- Which candidate seems to have a purpose which aligns with that one thing you think is the key?
- Which one has a CV, experience and tone (I nearly said “vibe”) that you think would give them the best chance to engage effectively and immediately with the critical relevant third parties (government and politicians mostly) that will need to be brought into the tent to achieve that one thing?
Which is to say, whatever that one thing is, it’s going to involve engaging in a more considered and effective manner with government and politicians, both state and federal, than we have in the past.
This is what I think that big thing is and with that how I would then filter candidates.
To be clear, I’m not saying I’m right about the one thing (although I think I am), I’m just offering it as an example to help outline a good process for choosing a candidate.
I want a president who has the experience, pre-existing cache and emotional intelligence to meaningfully start to shift thinking on a series of now out-of-date and misguided beliefs around how general practice and GPs operate.
Such beliefs are held by various key stakeholders in the health system, including but not limited to, policy people in government (some very senior and influential) and state and federal politicians.
This dynamic is holding nearly everything back.
I think that a lot of the problems you will read in each of the candidate statements that they are promising to fix are not problems, but symptoms of the actual big problem: that government departments and politicians have struggled to keep up with the culture of general practice and the way that culture effects their role in the healthcare system.
Why GP culture is now being misread is in part because the long established and safe Medicare paradigm helped build a lot of those beliefs. But that paradigm is breaking down now. It is rapidly becoming not fit-for-purpose to deal with the actual evolved culture of general practice and people have not caught up.
On top of this, healthcare is changing existentially and rapidly through an urgent need to shift emphasis in care from acute to chronic and through massive technology changes. These changes are also hard to keep up with, so people’s beliefs around general practice are rapidly going out of date and becoming irrelevant when making plans around general practice.
Some examples of what once may have been true culturally and some that were never actually true but came to be seen as true under Medicare include:
- GPs are insular, whinge a lot, don’t see the bigger picture and are actually very well paid (overpaid even). Note: a lot of people in government departments (not all for sure) think this still;
- GPs are paid for and looked after by the Department of Health and Aged Care (ie, GPs are on the payroll of the federal government on behalf of the people). Obviously not correct at all and rapidly changing even more now through connected care models, technology platform operators and a big push from the private sector, but still a widely held belief, nonetheless.
- GPs and hospitals are for free. They never were, especially GPs, but in the past it didn’t matter about this belief. Now the breakdown of Medicare and the economics of our system are making it clear they aren’t for free and that is creating tension with key stakeholders, especially patients.
- GPs shouldn’t be making a profit. Although a lot of key system stakeholders will acknowledge that GPs are small businesses, many of these stakeholders still can’t get out of that belief that GPs are really government employees and therefore they shouldn’t be making a profit. It’s strange.
- GPs are mainly there for families, the poor, and the downtrodden. They are, but they are there for so much more in a fast-evolving system and this is not being contemplated enough at the moment because this cultural meme restricts how innovatively policy people and politicians think of applying our precious GP resource. By the way, if GPs do look after the poor and downtrodden, how come we continue to refuse to pay them properly to look after our most complex and in-crisis mental health patients?
- GPs will always be there for us. Once this may have been true, but not anymore and everyone should be worried at the prospect that general practice can actually break down and GPs may not be there for us in the future.
- GPs need to sort out technology transformation for themselves, just like every other business. Interesting that we want to think of GPs as businesses only when it suits us. Technology transformation in general practice has suffered massive market failure and it’s clearly the job of government to correct such failure when they identify it. Better technology for GPs done the right way will substantively help transform the whole system. GPs, as mostly small businesses, are not able to do it themselves when such market problems exist.
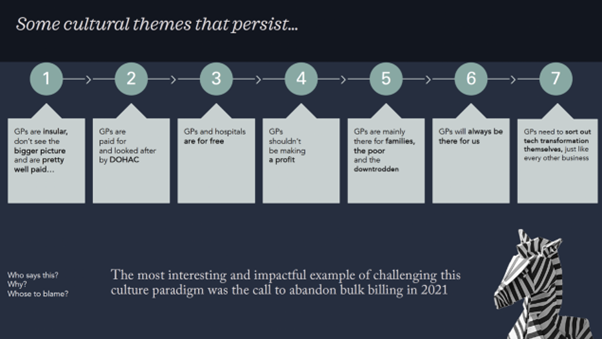
This is not an exhaustive list. You can probably think of a lot more cultural themes or beliefs that we apply in a blasé manner to general practice which either were never quite right but it didn’t matter because of how Medicare worked, or are simply not right any more.
By the way, I want to stress here that those policymakers and politicians who aren’t reading general practice right aren’t the main ones to blame for being stuck in a GP cultural paradigm that is fundamentally wrong.
I’ll let you figure who is more to blame but it’s close to home as far as the RACGP is concerned and ironically – given this article – it goes to leadership.
Related
Medicare was a fantastic and foundational system for a long time, and it’s not changing much because it’s wickedly hard to change the funding formats that underpin it in a federated system.
In such world, it’s very hard to discern how system fundamentals such as the machinations of general practice, are starting to break down and why, and even harder to work out how to fix it.
There is still much momentum in Medicare – like that of a trusted, giant and old aircraft carrier that has seen better days – and in our long-term political obsession with hospitals as the epicentre of our system to overcome.
If you’re wondering what a few more realistic and modern cultural norms around general practice are, here are few examples to get you started:
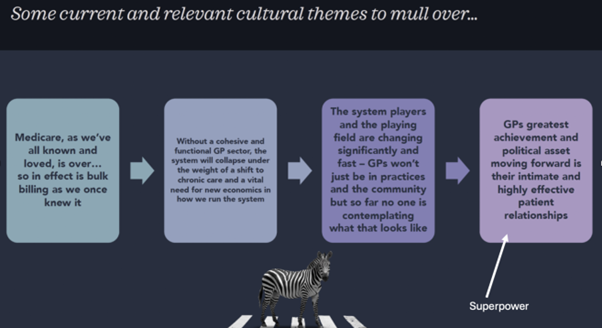
- Medicare as we’ve all known and loved it, is over … so is bulk billing as we once knew it. Which means the playing field for how GPs roll is changing radically and fast. GPs are spreading their wings because they have to.
- Without a cohesive and functional GP sector, the system will collapse under the weight of a shift to chronic care and a vital need for new economics in how we run the system. Importantly, this is one cultural theme that is acknowledged now by policymakers and politicians. Unfortunately, acknowledging something is wrong and doing something meaningful about it are two different things.
- The system players and playing field are changing significantly and fast. GPs won’t just be in practices and the community but so far no one is contemplating what that looks like, for GPs and the system. Policymakers and GP leadership need to embrace just how far and wide GPs can go into a rapidly evolving system. The RACGP still significantly hubs its advocacy around GPs in the old family practice model. That still exists but there is so much more these days, including their role in corporates, tech plays, private funders and rural and remote hospital systems, which the college needs to better contemplate.
So, if I want a candidate who can attack that one thing I think is wrong, I am looking for what?
In three words I want a conniving, consummate communicator.
Conniving? Is that a good quality for a president of the RACGP?
I think maybe conniving isn’t exactly the right word. It’s just that I don’ t think the person who can do the above is someone a key policymaker or politician will see coming.
You need someone who isn’t always going to say what they think because they know that influencing the high-level people you need to influence is going to take a lot of backroom work combined with some very well targeted strategic initiatives, some of which are not always going to make the powers-that-be happy.
If you think about all those misbeliefs that persist in parts of our system about how GPs roll, then I’d proffer that the most powerful move by a past RACGP president to challenge most of the outdated beliefs and culture did not come from elegant and influential communication, but in the horrifically blunt tactic of announcing to politicians that GPs are now going to stop bulk billing, thank you very much, because they are going broke doing it.
That move, by past RACGP president Adjunct Professor Karen Price, in late 2021, was not elegant and it did not win her any friends in Canberra or state government.
It took everyone by surprise and when it first happened there was quite a bit of head shaking and horror. But it turned out to be a highly targeted and effective tactic to wake up the policy people and politicians.
It went directly to how people might vote.
Vitally for general practice, the significant cohort of their patients that started rapidly learning they had to pay for something they had always thought or was told was free, did not turn on them.
They turned on the politicians.
And in that, general practice learnt a superpower it always said it had, but had never really tested – tight longitudinal trust relationships with their patients. Much better and tighter than pharmacists in fact.
Calling for a stop to bulk billing immediately challenged the cultural norms (some listed above) and a lot of GPs, who first thought of their patients, were immediately worried for their patients.
But it exposed boldly what had been going on for 10 years – that GPs were slowly going broke with no pay increases and being gaslit by governments to keep putting up with it – and importantly, it put a place marker down for the future and how the system should be thought about.
From a cultural perspective, the politicians significantly misread culture here. They thought that GPs, as empathetic and intimately tied to the betterment of their patients as they are (again, much more than pharmacists), would never abandon bulk billing because that would hurt their patients.
Bulk billing, if it wasn’t dead prior because the government could never afford to catch up 10 years’ worth of non-indexing ever, was doomed after this initiative, at least in the manner that Medicare and the system had originally designed it to work.
That even today the federal government clings onto bulk billing by saying that urgent care clinics are starting to solve all our problems – without any evidence to prove even a trend and no intention to measure what these centres are actually doing for three years – and that the tripled bulk-billing incentive has “stemmed the tide” of bulk-billing decline, is a sure sign that we still have a serious cultural misbelief that a conniving, consummate communicator will need to work very hard at breaking down.
So who fits the bill for this job, after you finish cutting out all the noise on those candidate statements with your big red marker?
Look for someone who you think:
- Can walk into Canberra and command some immediate respect for what they have already done, for how much understanding of the system they have already demonstrated, for where they have worked, and who you think will already be walking in having earned the respect of some of the key government and political players. Presidents only have two years. They have no time to waste.
- Notwithstanding all the elegance and smarts of the above, they need to have some mongrel in them. I don’ t think Karen Price is going to appreciate the compliment, but calling on all GPs to stop bulk billing at the time she did, took a lot of mongrel. It was a very calculated move and it didn’t make it very easy for her outgoing tenure, or the next president arriving in Canberra. Initially the politicians were openly hostile. But it was nothing but impactful and effective. Dr Harry Nespolon (president prior to Adjunct Professor Price) was at once a consummate charmer and influencer who had a lot of mongrel. He didn’t go mongrel a lot but when he did he picked his time and target and landed some important blows for general practice.
- Can defy the college when needed for the greater good of the profession. According to Adjunct Professor Price she didn’t ask the college board for permission to call on GPs to stop bulk billing. If she did you strongly suspect the idea would have never seen the light of day. Dr Nespolon at times dispensed entirely with seeking board approval to do things.
You might also look for anything in those long lists of ideas in the statements that might have the whiff of a strategic initiative that would go to a candidate being able to pull off this one thing.
Hint: the call-to-abandon-bulk-billing episode has starkly shown us that despite patients liking to whinge about GPs – even join in the “they’re all overpaid” rhetoric we get a lot from politicians – patients love their own GPs.
Are any of the candidates suggesting any good ways of leveraging that love in a manner that is going to help?
In a couple of the statements you will see some interesting ideas around organising GPs in a much more comprehensive manner to regularly engage with their local member. This is a highly effective tactic that the Pharmacy Guild has used for years.
Why GPs haven’t gone there is still a bit of a mystery, but hopefully they are going to now because patients like and respect their GP more than their pharmacist. That’s a huge latent power that a good president organising well might unleash.
So who did I pick?
I’ll let you try to work that out, but there are at least two in there who it could be.





