Experts are encouraging ongoing awareness and vaccination with the possibility of things getting worse before they get better.
Vaccination numbers are down, case numbers are up, and other respiratory diseases are circulating.
Earlier this year experts felt low vaccination rates and steadily climbing flu cases could create a “perfect storm for a severe flu year”. And in news that should be surprising to absolutely no one, they were right.
Data from the National Notifiable Disease Surveillance System reveals there were 14,000 more laboratory-confirmed influenza cases between January and June this year compared to the same period last year (148,731 versus 134,960). There were 36,039 cases in the first 11 days of July this year, already more than half of the 56,681 reported in July 2023.
Queensland-based infectious diseases physician Professor Paul Griffin told The Medical Republic that even though current case numbers were high, we were yet to hit the peak – meaning numbers could continue to climb over the remaining winter months.
Professor Adrian Esterman, an epidemiologist from the University of South Australia, had a slightly different opinion.
“We did see an earlier start to the [flu] season this year, so we had several times as many cases in the beginning of the year. [Now] if you look at the cumulative number of cases it’s not too dissimilar to [what we saw] last year. But we will have to wait and see whether or not the peak goes much higher than last year,” Professor Esterman told TMR.
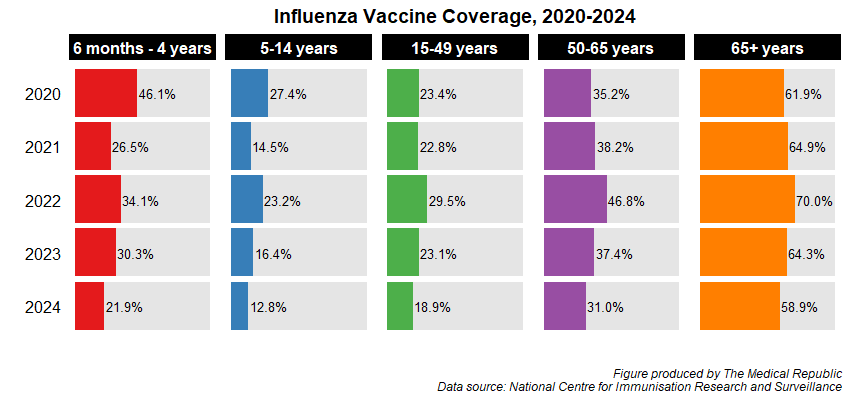
Both Professor Griffin and Professor Esterman felt declining vaccination rates had contributed to the increased number of cases, despite ATAGI recommending all people aged six months and above should be vaccinated against influenza earlier this year.
Vaccination coverage data from the National Centre for Immunisation Research and Surveillance shows vaccination rates have fallen for all age groups since 2022.
Professor Griffin was concerned by the low vaccination rates but felt there was definite merit in still getting vaccinated, telling TMR the two main circulating influenza strains are covered by the vaccine. He also clarified the misconception that you don’t need to get vaccinated if you have already had the flu, as “even if you’ve had one [strain], you can still get the other one”.
There is also greater scope for using antivirals like oseltamivir, which Professor Griffin believes is being underutilised.
Professor Griffin said the recommended measures people could take to protect themselves against influenza – getting vaccinated, hand hygiene, mask wearing and staying home if you feel unwell – were also effective at minimising the spread of other respiratory diseases such as covid, RSV, pertussis and mycoplasma pneumonia.
Related
“We need to remind people [about] the value of [these measures] because I think we did quite well [with them] for a few years during covid, and perhaps the fact that we’re doing all of those things at the lowest levels in some time is why we’re seeing quite bad seasons for a host of different infections,” Professor Griffin said.
Professor Esterman echoed Professor Griffin’s call for healthcare professionals and patients to bring back wearing masks.
“There’s now ample evidence [that face masks are] protective against respiratory infections. So if that’s the case, mandating them in healthcare settings [would be helpful],” he told TMR.
South Australian-based immunisation education consultant Angela Newbound told attendees at an Immunisation Coalition webinar earlier this year that the flu normally affected 5-10% of the community each year, with rates as high as 30% in children.
Common symptoms of influenza include fever, chills, headache, feeling tired and weak, a stuffy or runny nose and a sore throat. Children with influenza can also present with abdominal pain, nausea and vomiting. Infection can lead to serious complications such as breathing problems, pneumonia and death.
It is estimated that 1.5 million workdays are lost to the flu each year, in addition to over 300,000 GP visits and more than 15,000 hospitalisations.