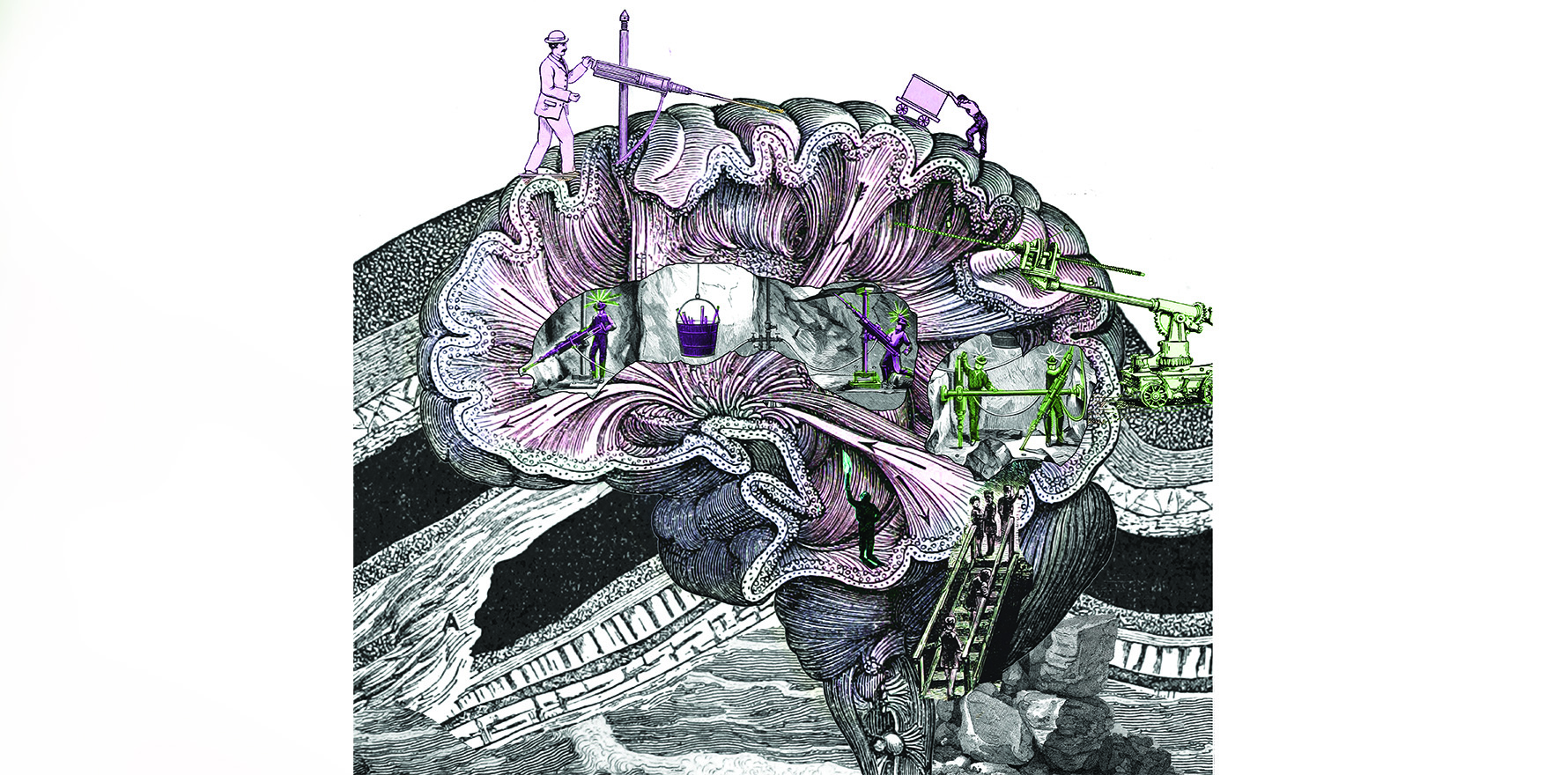
Deep brain stimulation is thought to improve mental health symptoms by affecting the way neurons fire in the brain and communicate with one another, but experts aren't completely sure on how this works
What if some of today’s hardest-to-treat psychiatric problems could be treated with a zap of electricity to the brain?
You may have already heard of this treatment for people with Parkinson’s disease, when an electrode is placed deep into the brain to deliver an electric current. Watching doctors switch on the device is miraculous. You can see the shaking hands immediately steady once the current is switched on.
Thanks to its success in treating Parkinson’s disease, deep brain stimulation (DBS) is now being explored for other conditions.
“The first frontier was movement disorders,” says Professor Matthew Kiernan, co-director of the Brain and Mind Centre at the University of Sydney. “Now we’re getting into trialling this approach across a range of brain and mind disorders, from depression and OCD through to epilepsy and MS.”
Brain and neurodegenerative disorders are some of the most important health concerns on the horizon. We are increasingly recognising the cost that such illnesses exact from individuals, as well as their carers and loved ones, and some of these conditions may become increasingly prevalent as the population ages.
Despite this, effective treatments are limited.
For instance, as many as one in three people with severe depression may fail to benefit from two or more different treatments. This leaves people distressed, disabled, and at risk of other physical and psychological comorbidities.
Enter deep brain stimulation.
Surgeons cut a hole in the skull that is the size of a five-cent piece then insert a spaghetti-like electrode into a specific region of the brain thought to play a role in the dysfunction. Deep brain stimulation is sometimes called a pacemaker for the brain, because the electrodes stay in the brain long-term, delivering continuous or repeated electric currents from a battery that sits under the skin near the collarbone.
But each condition relies on a different part of the brain being stimulated.
For Parkinson’s disease, the electrodes may be inserted in the parts of the basal ganglia, such as the subthalamic nucleus or globus pallidus, which play an important role in motor control.
In the three or four years after the insertion, patients experience a 40% reduction in symptoms on average overall, and may see up to a 90% reduction in hand tremor.
Funnily enough, experts still aren’t completely sure how deep brain stimulation helps improve people’s symptoms. This electrical stimulation is thought to affect the way that neurons fire in the brain and communicate with one another.
Given that Parkinson’s disease is characterised by neurons misfiring, delivering a jolt of electricity may interfere with these misbehaving brain cells and thus prevent the tremors.
More than 160,000 people around the globe have been treated with DBS. However, in Australia the treatment is only approved and funded for the treatment of Parkinson’s disease, essential tremor and dystonia. DBS is approved, but not yet funded, for use in epilepsy and obsessive compulsive disorder (OCD).
EPILESY
Around one in three patients can’t stop their seizures with medication alone. For these individuals, DBS may help.
“In epilepsy it’s often used to break up circuits,” Professor Kiernan says. “It’s like a lesion – like cutting out part of the scar that might be causing the epilepsy. If you put electrodes into that area and turn the stimulation rates up it sort of paralyses that part of the brain so the seizures don’t occur anymore.”
Just like for other conditions, the patient may need to stay awake during the surgery so that the surgeon can ensure the electrode is placed in the right spot. This is a delicate act, as the target region may be only 1mm or 2mm across.
Using this technique, around one in two patients have fewer seizures, research suggests.
Unfortunately, it may take more than a year for the benefits to emerge, and patients often still need to continue their anti-epileptic medication.
OBSESSIVE COMPULSIVE DISORDER
OCD is one of the most paralysing ongoing mental health conditions, and 10-20% of patients don’t respond well to any treatment.
A number of targets in the brain are being investigated for OCD. In 2008, a small French study showed that positioning an electrode into the subthalamic nucleus led to a significant reduction in OCD symptoms among people who were severely ill and treatment resistant.
More recently, research has shown that stimulation of the superolateral branch of medial forebrain bundle, which plays a role in the reward system, resulted in a 35% reduction in OCD symptoms in one patient and the other was close to remission 12 months after the implant.
In addition, a study of 70 patients with treatment-resistant OCD, found that deep brain stimulation halved symptoms of depression, anxiety and obsessive compulsive scores 12 months after insertion. The paper, which was published earlier this year, classified half of the participants as responders and one in six as partial responders.
OCD is one of the conditions that DBS has the most support in, but even here its use is still somewhat experimental.
One of the key issues troubling researchers is that while some significant benefits have been found in small studies, these often seem to wash out and become less effective when trialled in bigger randomised controlled trials.
For no condition is this effect more apparent than in treatment-resistant depression.
DEPRESSION
Professor Paul Fitzgerald, deputy director of the Monash Alfred Psychiatry research centre (MAPrc) has trialled DBS for patients with extremely treatment resistant depression, who have had little success with other treatments.
His team’s pilot experiment found that patients responded really well, and the benefit was sustained over a long period of time. In one patient, the antidepressant effects lasted around eight years, and in another it has lasted for over 10 years so far.
However, the device didn’t work for everyone, and when Professor Fitzgerald and his team studied the results in a more comprehensive trial, the results were less promising .
There are several possible explanations for this. The first is that there are a number of different biotypes of depression, and each needs slightly different treatment.
“It might be the case that the target in each individual patient might need to be individualised by an understanding of how the networks of their individual brain are dysfunctional, rather than a one size fits all situation,” the professor of psychiatry at Epworth Healthcare says.
Neuroimaging studies suggest that choosing a site should focus on the types of symptoms we want to alleviate, rather than trying to “fix” a condition as heterogeneous and multifaceted as depression .
Another explanation for the lack of experimental support is that the studies may be too short. In an open-label study, around half of the patients responded to treatment at the 18 to 24 month mark.
“In movement disorders you see a very rapid effect. For example, a tremor will stop when the electrode is implanted and switched on,” says neuroscientist Dr Susannah Tye. “Whereas for psychiatric disorders you might see some small changes, but others take a lot longer to develop.”
We now realise that DBS is doing more than just reducing the neural activity, it is modulating the circuitry too, says Dr Tye, who is group leader of the Functional Neuromodulation & Novel Therapeutics Laboratory at the Queensland Brain Institute.
This suggests that DBS needs to be coupled with psychological support and rehabilitation to be effective for some conditions, and this may explain why the benefits have been muted in larger trials.
“One of the things we think it is doing is enabling the brain to become more plastic and adaptive,” says Dr Tye.
When we learn anything, whether it is a person’s name or a new skill, connections are being formed in the neural circuits.
When this is repeated, the connections between synapses get stronger, and this is known as synaptic plasticity. Or put more simply: neurons that fire together, wire together.
“We suspect that in the treatment resistant brains, that the brain is quite resistant to changing those connections,” says Dr Tye.
Now there is evidence that DBS may be helping to prune some of those connections and promote the growth of new ones. In a similar way, antidepressant medication promotes new connections in the brain, which is why they can be used for people with anxiety and PTSD.
“It’s almost like it’s unlocking the circuit,” says Dr Tye. “Just trying to do that without trying to bring in that rehabilitation means that you are only doing half of the process.”
CHRONIC PAIN
Chronic pain was one of the first indications for DBS, although research has similarly found mixed results for the treatment. In a study of 17 people with cancer pain, DBS was able to make people almost pain free, with only four still needing opioids afterwards. The pain did return for many in their final weeks of life.
The thalamus and the cingulum are two common targets for patients with severe refractory neuropathic pain. DBS is also used in phantom limb pain.
One of the challenges is that pain is subjective, and harder to measure than movement disorders.
DISORDERED EATING
DBS has also been used to treat eating disorders.
The hypothalamus, and in particular the nucleus accumbens, are part of the reward system and have been implicated in motivation for food.
Studies in animals show that binge eating can be reduced with stimulation of these regions.
A Danish study of seven obese patients found that coagulation of the hypothalamus lead to weight loss, although they regained weight a year after the intervention, prompting interest in continuous DBS for ongoing weight loss.
Several studies have looked into DBS as a treatment for anorexia nervosa.
One study of 16 patients found that stimulation of subcallosal cingulate significantly reduced depression and anxiety in these patients and changed the brain activity of key areas thought to be responsible for the illness. Participants began to gain weight over the next few months and researchers believed it was due to better mood regulation and engagement with anorexia treatment.
COGNITION AND MEMORY
Beyond this, researchers are currently investigating whether zapping the brain might help out people with memory problems linked with dementia.
Clinical trials on Alzheimer’s disease have targeted the fornix, which is the structure connecting both sides of the hippocampus. Recent research has found that stimulation to this area may enhance neurogenesis, improve synaptic function and cell survival. In some patients, this has been shown to improve metabolism in areas of the brain that were starting to go quiet, and stalled cognitive decline.
The results have been mixed however, with some studies finding benefit and other more rigorous ones not displaying any difference. Researchers are still trying to determine which patients will respond and which part of the brain is the best to target.
ADDICTION
Another area where DBS is being used is in treating drug and alcohol addiction.
In addiction, the brain’s reward system starts to change, and one of the key regions responsible for reward is the nucleus accumbens.
Animal research suggests that stimulating this part of the brain decreases the animal’s drug seeking, and research in humans suggests that heroin and alcohol dependent patients are more likely to remain abstinent when this part of the brain is targeted.
OTHERS
DBS has also been trialled in schizophrenia, bipolar, narcolepsy and tinnitus. One recent small open-label found that six months of continuous stimulation to the caudate nucleus led to a clinically significant improvement in symptoms for 60% to 80% of the patients with treatment-resistant tinnitus.
There have been early promising results for Tourettes, indicating that DBS can reduce tics and obsessive-compulsive behaviours.
However, side-effects include a sudden worsening of symptoms when the DBS is stopped, and mania or hypomania.
LIMITATIONS
Of course, the procedure is not without side-effects for other conditions either.
Patients are at risk of haemorrhage, irritation from where the wire runs under the skin, infection and other surgical complications.
The electrode and battery can break, and even if it doesn’t, the power source will need replacing after several years.
In addition, up to half of Parkinson’s disease patients get side-effects from the stimulation, which include depression, speech and balance problems.
These are mostly mild though and depend on where the electrodes are inserted. Many side-effects are also reversible and will clear when stimulation is turned off or the electrode is removed.
Developments in technology are expected to improve some of these effects, and researchers have recently developed electrodes that pulse in only one direction rather than radiating in all directions, reducing the risk that unnecessary parts of the brain get affected.
There are also regulatory limitations, with DBS being banned for psychiatric disorders in parts of Australia, such as New South Wales and the Northern Territory. This cautiousness has come from psychiatry’s chequered history using neurosurgery to treat psychiatric conditions, but may lift when the evidence base is stronger.
What’s more, the cost of the procedure may be upwards of $60,000.
THE FUTURE
DBS is a valuable tool to both treat and investigate the way our brain malfunctions. Researchers are now racing to understand the biological underpinnings of brain diseases better, so that they can target increasingly specific areas of the brain.
It’s exciting to think of how zapping the brain may heal us from some of the hardest problems we face in brain and mind problems today.