The variation in performance from one primary health network to the next is a bit of a lottery as far as GPs are concerned.
Unbeknown to most primary health networks, the Department of Health recently awarded a contract to consulting firm PwC to do a review of the sector.
Precisely what the DoH wants reviewed isn’t entirely clear, however.
PwC has asked PHNs to submit complaints that they have received from providers as a part of the review, but they aren’t taking direct input from providers (one smart provider tried) – which seems like a strange way to go about reviewing the sector. If you ask only the PHNs, surely you will end up skewing any findings towards what PHNs want you to see?
Earlier this year, PwC surveyed PHNs themselves to understand their challenges better. The insights aren’t particularly enlightening. Most of the issues facing PHNs mirror the problems facing practices: funding pressure, workforce issues, covid-19 and managing a new telehealth regime.
The PwC report summarises by saying PHNs increasingly see a role for themselves in capability- and capacity-building activities such as supporting the uptake of telehealth.
There is no mention of the rapidly growing role of PHNs in aggregating the data of their practices, analysing it and feeding it back to the practices in order to help their practices understand better the population health needs of their region.
Nor is there any mention of PHNs extending their strategic plans to include getting directly into the software business by building their own products to compete with quite a few long-term health-tech vendors, an issue we reported on a few weeks ago.
We had questioned in that article whether PHNs moving to build their own software wasn’t some indication that the sector was playing fairly loose with their funding protocols and core mission. The article looked at a submission by the WA Primary Health Alliance, which runs WA’s three PHNs, to the ACCC to effectively clear the way for the group and several other PHNs based in Queensland to monopolise the market for GP-generated population health data.
Given that 33% of PHNs in the PwC survey indicated that they weren’t funded to perform all the things they’ve been tasked with achieving, it might be that these PHNs feel they can save themselves a significant amount of time and money by bypassing the commercial software market.
We also said in this article that “anecdotally, most GPs don’t think much of their PHNs”, something I’m going to admit was a pretty lame attempt at adding to the argument that PHNs seemed to be a bit all over the place these days, and shouldn’t someone be keeping a better eye on exactly what they were doing so they weren’t going off the reservation too much and doing stuff like trying to build fairly complex medical software.
We partly made this deduction from some past surveys. In 2018, an AMA survey revealed that 58% of GPs felt that their PHN had failed to improve local access to care for patients. This was compared with 73% in 2013. Sixty-two per cent said their PHN had done nothing to build their capacity to deliver better-quality healthcare.
Hence our interest in the PwC PHN review, which is due out by Christmas apparently, and then our disappointment when we learnt PwC’s methodology of review was mainly asking PHNs to send in complaints about themselves.
Taking all this into account, we decided to ask GPs some questions directly about what they thought of PHNs, in an attempt to get a better handle on our “anecdotes”.
The survey was run as a part of HealthEd’s regular fortnightly PULSE survey series. The total sample of GPs answering this survey was nearly 1200 but only 456 GPs answered the PHN questions, of which 219 self-identified as being either practice owners or managers. That’s just a bit more than the AMA survey in 2018, which had a sample of 399.
Our first question asked respondents to rank their PHN on a scale of 1 to 10 for usefulness, with 1 being useless to 10 being highly useful.
The mean result for this question was 5.3, so on average you might say that GPs think PHNs are halfway between useless and highly useful – which would be “useful” maybe, but not by a lot.
But the results weren’t clustered around the middle, so the mean result doesn’t really tell the story of the data: when we dug into the individual results, what we found, especially among the respondents identifying themselves as practice owners or managers, was that in general PHNs were either getting very high scores, or very low scores.
In other words, GPs think their PHNs are either pretty good to great, or pretty bad to hopeless – we got quite a few scoring 1s across the board for their PHN, and some giving 8s to 10s.
The result seems to be pointing to quite a stark variation in performance of PHNs as far as GPs are concerned. Some GPs think their PHNs are on the ball and helping, and others clearly don’t.
The data starts to get a little thin when you break it down by rural and remote to urban areas and a skew towards rural and remote doing a worse job, according to their GPs, is not statistically significant.
But it would be really interesting to get enough data to see if there was a real difference.
PHNs serving rural and remote have a lot more problems to oversee on behalf of their GPs than urban PHNs, so perhaps the pattern is real and not surprising.
Certainly the pattern of bipolar response to the usefulness of their PHN is real.
If you do draw from this data that there is quite wide variance in the management capability from PHN to PHN, then it is apparent that some PHNs are nailing engagement with their GPs and doing a good job, while others are missing by quite a bit.
Bad luck, I guess, if your PHN is one of the bad ones.
Supporting this conclusion would be the history of how PHNs have been built over the years and managed. Each is a separate company with a separate constitution and governance. This allows for quite a bit of potential variance in how a PHN might be run.
But is anyone monitoring this on behalf of GPs and making an attempt to provide some sort of performance guidance to the low-performing groups?
To some extent, we seem to have at least started this process.
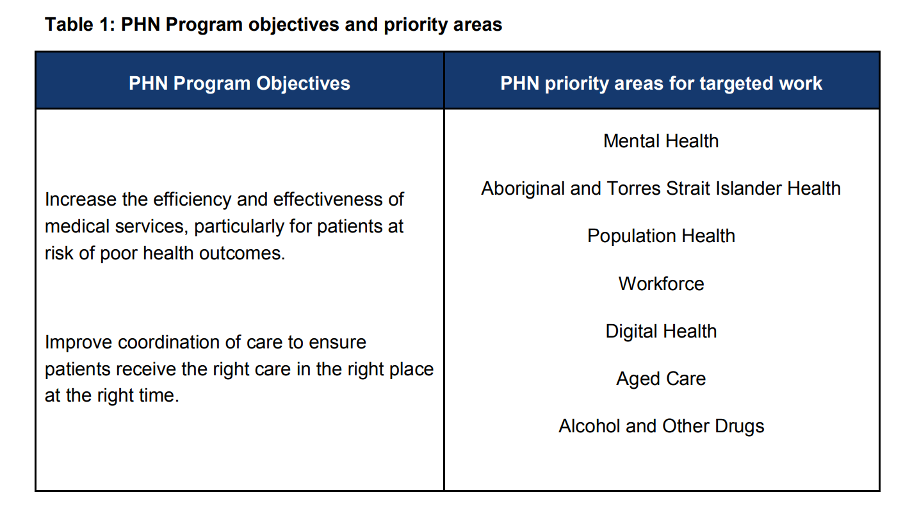
In 2018, the DoH established a “Performance and Quality Framework” program for PHNs in some attempt to bring cohesion across the sector in terms of purpose and performance. At the highest level, the DoH set broad program objectives for PHNs and some priority areas, and then said that there would be obvious variance in emphasis depending on what region a PHN was serving.
The program sets out quite specific guidelines for performance reporting and management of the PHNs, including that the DoH will publish an annual report of the performance based on the guidelines set out in the paper. Essentially, each PHN has to build its own work program and then set objectives and KPIs and work to them. They also are meant to self-report, which might not work too well.
So far, we haven’t seen any performance reports for any PHNs. But it’s almost certainly going to give rise to “covid ate my homework” excuses, given the timing involved in the introduction of this program.
The program was outlined only in late 2018, and we’re guessing that with a year to do a bit of backwarding and forwarding between the DoH and the PHNs on fine-tuning the framework, and then covid starting in early 2020, we haven’t got far with the whole program just yet.
If it’s of any interest to the DoH or PwC, it looks like about half of GPs score their PHNs as a fail, and half a pass.
Given GPs are the main clients of PHNs still (when they became PHNs their remit broadened quite a bit beyond just meeting the needs of GPs), it’s quite possibly a strong indicator that at least half of the PHN system may not be performing.
A half is a lot when you think that PHNs attract grant funding from the federal government in excess of $5 billion each year.
If we have $2.5 billion worth of underperforming PHNs, which is what GPs seem to be suggesting in this survey, and the DoH PHN performance program has been suspended temporarily because of covid, it probably needs to be unsuspended pretty quickly.
So far, you might say the DoH is in a paradigm – something akin to what most marketers would recognise about their advertising spend: “I know half my PHNs are working, I just don’t which half.”
The HealthEd/TMR Pulse survey did ask for more detail on the key priority areas identified by the DoH, the results of which are here if you’re interested. We can’t make much of it, other than it all seems to be half-half again.