GP advocates were finally getting somewhere, now they're drinking the government’s triple-bulk-billing-incentive Kool-Aid.
Possible irony in today’s piece about the ramifications of the continuing collapse of bulk billing: it’s being written from the emergency department of a nearly brand new public hospital in a high-SES suburb of Sydney.
My partner has a particularly nasty case of RSV, and after a week of suffering is going downhill fast.
We felt that we had better check for pneumonia and other possible side effects, which was medical advice we’d been given early on in the illness.
We just needed a medical second opinion now on what to do next.
Of course we tried to get into a few local GP practices including our own, but there were no appointments for a few days, not even a telehealth call.
None of them answered their phones, either – they kept going to voicemail.
Busy Thursday, I guess.
All good though: we’re No 45 on the ED waiting list in the local hospital now.
We’re actually isolating outside, where the weather is pretty crispy, as I’m pretty sure that inside could end up ground zero for a new pandemic.
There’s just a hint of “what are you even doing here you horribly infectious middle-class gremlins? Go and see your highly remunerated local mixed billing GP why don’t you?” from one staff member.
Which would be fair except we tried really hard to do that. We don’t want to be here either.
No one is brave enough to estimate a waiting time. If that information got to any of us punters past 25 on the list, I’m guessing there could be a riot – even among us sophisticated well-off folk – so staying stumm on that sort of intel feels smart.
My guess, based on the progress of the first three patients in the 45, is about four to five hours, by which time my partner’s head might actually explode based on her current state.
Still not complaining (my partner would but she isn’t capable of speech at this point, which helps).
It is what it is. Besides, having been here before, I brought lots of water and camping gear.
As I finally connect to the wi-fi (bet you can’t get that in a country hospital) I am starting to wonder a lot more about what’s going on at the other end of the system spectrum if we are the lucky ones enjoying the smooth end of the pineapple.
It feels just a little like we might be moving beyond leaks and cracks towards imminent and significant structural failure. Some might say we are already there, with the GP crisis and ambulance ramping in certain city postcodes.
We would have gladly paid way over the odds just to see a GP quickly who could have pointed us in the right direction, rather than suffer the trials of a public hospital ED (I’m thinking there might be an online auction-type business model in that but it’s a pretty ugly thought).
The thing is, bulk billing collapse or not, we couldn’t get close to seeing a GP in a well serviced wealthy Sydney suburb at the one time in the last few years we probably really needed to see one, and in the one circumstance the government is desperately trying to avoid: a couple of punters who can afford mix billing and more, defaulting to a strained hospital system for lack of GP access.
Of course some people will (rightly) point to this situation and say “Boo hoo, you poor middle-class Sydneysiders, couldn’t get to a GP locally in a day? Try to get to one in three weeks in my town.”
But that’s sort of the point. You can’t get either.
This week’s Department of Health and Aged Care numbers on bulk billing for the March quarter reveal that in just one year bulk billing has dropped a whopping 11.3%. It’s possibly more because the government figures have masked the raw numbers of patients who have lost access to bulk billing, and certain items allowed during covid (especially telehealth items) seemed to have masked the start of the decline.
The data show that bulk billing’s decline is gaining significant momentum, after something like 15 years of relative stability, not withstanding rebate freezes for GPs for most of the last 10 years of that period.
If you look at the trend on the basis of total services billed (see below) and not rate of billing, the decline is even more alarming (it’s approaching 20%).
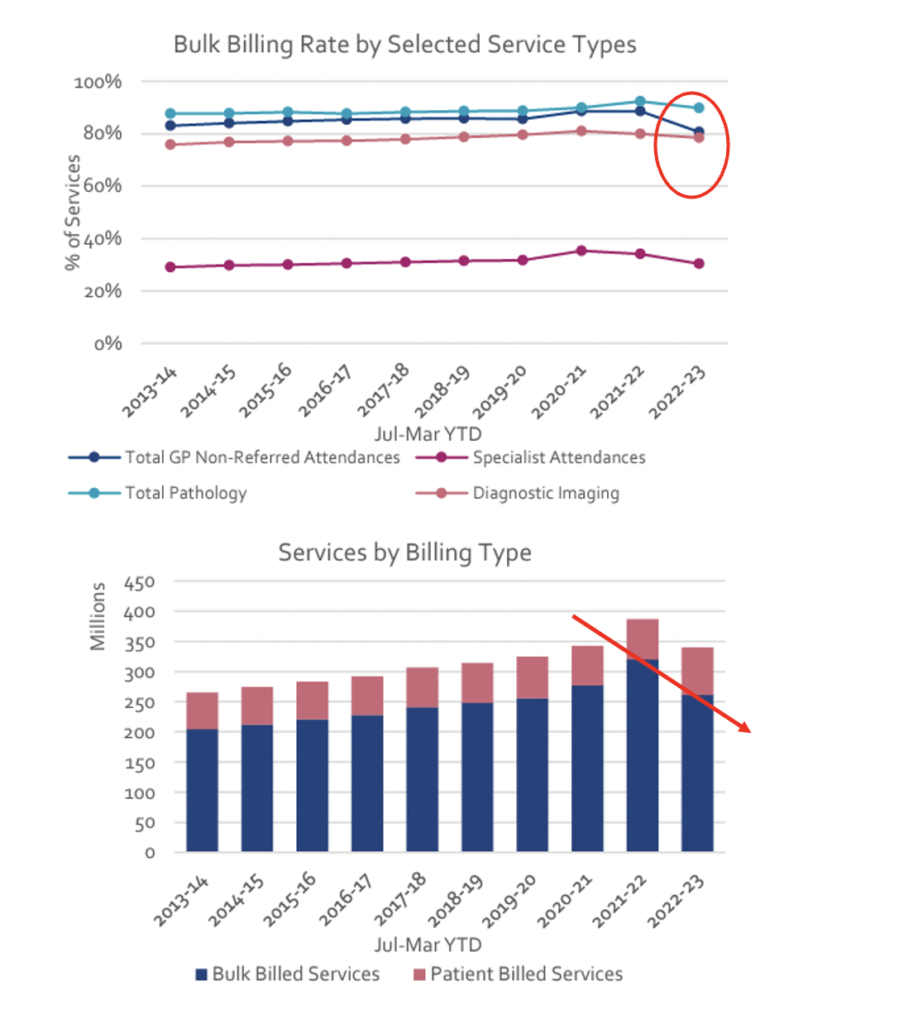
In three months’ time when the next Medicare stats are due, we might all be in for a much bigger shock, and then again another three months later, because nothing announced in the budget will have had any time to kick in by either date.
The boosted bulk billing incentives don’t even start until November, while the indexation of rebates happens July and then again in November.
Even then it’s far from certain those moves will do much to slow the fall in bulk billing, let alone bring it back up to where it was.
Let alone touch the sides of the GP supply-side problem.
The budget feels like very little very late – yet the colleges and AMA are backing it enthusiastically.
Before the budget they had their feet firmly on the throat of the government for the first time in decades.
It wasn’t just good politicking on their part. The system was genuinely starting to break down in front of all sorts of people, and big media was running stories most days (although Nine and the ABC did walk a lot of the government’s problem backwards in October with their $8 billion Medicare rorting fairytale).
There was also some very hard and, turns out, good politicking in there: Adjunct Clinical Professor Karen Price’s public call to all of GPdom to start abandoning bulk billing was a landmark stance for an RACGP president. In days gone by it would have been regarded as an outrageous act met with some form of government retribution for the college, and possibly even internal organisational repercussions.
Given the obvious momentum of system collapse, the still delayed time frame before we start to actually address that collapse, and the obvious existing shortfalls in both money and policy in the budget, it’s not that easy to understand why nearly all the colleges and associations have so forthrightly come out in support of the government and the budget.
Yes, if you’re the polite type, who needs to win some friends, and you look at all the things the government is trying to fund in this budget along with Medicare, tripling bulk billing incentives and increasing rebates by 4% is certainly “a start”.
But a “great start”, a “game changer”, “immediate resuscitation” (all one liners used by either the AMA or the RACGP)?
Anyone in Canberra eyeing off the government in the days following the budget could be forgiven for tilting their head a little or even changing their facial expression to maybe a wry smile, as some sort of acknowledgement that, directionally, the budget had at least sent some signal of change and intent.
But anyone doing the maths on the rate of system decline, as described by this week’s bulk billing stats, and the ability of this budget to catch this problem, would almost certainly not have lifted their foot even one millimetre off the throats of those in Canberra.
So what do statements like these ones from the RACGP and the AMA mean?
“… the federal Budget [is] a game changer for GPs, practice teams and the patients they care for across Australia”
“I commend the Albanese Government for committing to this massive investment …”
“This $5.7 billion funding … will help to stem the bleeding, relieve pressure on our entire healthcare system including our hospitals, and ease pressures on people struggling to afford the care they need”.
“… we’re delighted to see initiatives and funding that put general practices at the heart of long-term reform and build the teams around them that can provide care for Australians with complex and chronic conditions”.
“We absolutely welcome the enormous injection that we’ve seen tonight in funding to immediately make healthcare and general practice visits affordable and accessible …”
Does anyone doing the maths here think that this budget:
- Will stem bleeding, start reversing the sort of public hospital problem I ran into this week, and meaningfully ease pressure on those, unlike me, at the wrong end of the system (say someone in a remote country town with no access to a GP on an income that couldn’t afford a gap if there was a GP in town)?
- Put general practices at the heart of long-term reform?
- Build teams around GPs that will be able to provide effective care for complex chronically ill patients?
- Immediately make healthcare and general practice visits affordable and accessible?
These are some pretty big hairy-ass goals (BHAGS) the AMA and the RACGP are claiming a win on in a budget that clearly put Medicare behind a whole lot of other priorities established for voters at the last election (NDIS, aged care, child care, defence and so on for quite a bit).
Most of the above BHAGS, which the AMA and the RACGP are suggesting we’ve won on, will almost certainly not be achieved in this budget and if we do make any inroads, those inroads are going to be spread out over the time to the next election, not immediate.
The interesting aspect of the position being taken by the member organisations here is that if you poll GPs and social media, they aren’t taking the view of their organisations at all.
In a GP poll TMR conducted last week, over 83% of respondents said that the budget was either not a game changer at all, or they were still undecided as to whether it was or not (split evenly).
Only 16% said they thought it was in fact a game changer.
In support of the idea that the bulk billing decline numbers released this week might be signalling a terminal decline, over 75% of GPs said they would not change how they bulk billed after the budget or weren’t sure they would change (63% said a flat out no).
That’s a lot of disconnect between the members and their respective representative organisations who are supposedly doing business on their behalf down in Canberra.
I’m completely unsure as to what such a disconnect means for the chances of my very ill and highly infectious partner one day not having to go to number 45 in a line at a hospital ED, when despite being reasonably well to do and living in a highly serviced GP region, we still couldn’t access a GP for love nor money.