Following this budget GPs need a better plan.
There wasn’t just nothing in this week’s budget for general practice, there was a shopping list of healthcare initiatives and investments which will add significantly over time to fragmentation of the care GPs try to provide.
That list includes more urgent care clinics; significant new funding for mental health services outside of and not connected to general practice; $3 billion more for pharmacists amid a spate of unreviewed pharmacy prescribing trials converting to established practice; and more money for hospitals to expand a trend in which they tightly manage their patients back out into the community, often cutting GPs out of the loop because it’s too hard to keep them in.
When everyone was in that room whiteboarding all this stuff with the Health Minister at various times in the last couple of months, a room presumably spotted with a few smart Department of Health and Aged Care apparatchiks to ensure no one was missing any important nuances, did no one put up their hand and say something like:
“Errh, do you think maybe, given all the hoo-haa we carried on with last year about Strengthening Medicare and that to do that we had to take general practice far more seriously as it was clearly the pinch point for making the whole system work in a few years’ time when chronic care really kicks in – that, maybe, we should think about throwing something to GPs that indicates we’re still with them and we were actually serious last year?
“I mean, I know health and Medicare aren’t the big show this year, but if we do absolutely nothing for GPs this time around, and we throw $3 billion at pharmacy, $500 million or so at extracurricular non-GP mental health, and nearly a billion at hospitals and aged care, won’t that look like we may not have actually been serious about all those things we said about rebuilding general practice because it is the core of our future health system strategy?
“Seriously guys, even what we threw at them last year involved quite a lot of smoke and mirror stuff if you think about how we added it all up for them.
“Can’t we just ring the boss and ask for say a billion even, so we can throw something half meaningful their way that aligns to the promises we’ve been making?
“Anyone….?”
I’m going to assume that if anyone did make that plea it was followed by the sound of crickets.
Even if the government was never actually serious about backing properly into a GP sector repair it’s hard to see any upside in the government doing nothing at all to send some sort of signal – a false one, even, for now to keep up morale – that they are still firmly on the journey that they seemed to start last year with such fanfare.
If I’m a GP who thought Strengthening Medicare and the new money last year was maybe the dawn of a new understanding of what is wrong, today I’m thinking, no, it definitely wasn’t.
In any way.
To do absolutely nothing is one thing. To then fund a series of initiatives that will in effect do the opposite of what all your rhetoric about shoring up general practice last year was about, is another.
It’s a statement of some sort and GPs probably need to think carefully about what sort.
The government seems to think it did enough last year to somehow keep GPs on side without any follow through at all this year.
That’s a pretty interesting gamble to make and I’m going to assume they’ve considered the pros and cons of what they’ve done.
We headed one of last year’s budget commentaries with “Just enough to stop a riot”. I don’t think anyone knows what a GP riot might actually look like (I’d sort of love to see one). But I’m pretty sure I know what the start of one looks like.
It looks like what Adjunct Professor Karen Price said in November 2021 about bulk billing.
When Professor Price, fed up with years of inaction and hollow rhetoric, crossed what many feared might be a sort of unwritten GP-duty-of-care Rubicon, and told all RACGP members to forget about 100% bulk billing and start charging anyone who could afford to pay an additional fee, things started heating up politically pretty quickly.
At first GPs were reluctant to start mixed billing, but soon they started to realise that a swathe of their patients could afford it and didn’t complain, and yet another swathe did complain, but could also afford it.
It wasn’t a perfect tactic. Without the ability to clearly communicate with their patients in order to properly sort out those that could and couldn’t afford to pay on top of the Medicare rebate, a lot were going to get confused, some understandably upset, and some were going to start falling through the cracks.
But as bad and unfortunate as that problem was it started to create political havoc pretty quickly.
Whether it was actually causing hospital EDs to back up or not, politically it was easy to point to declining bulk-billing rates and blame it.
The good part about that was that patients, advocacy groups and state governments weren’t blaming the GPs. They started pointing the finger squarely at the federal government.
You could argue that the call to abandon bulk billing by Professor Price was the catalyst that set in motion all things that ended up in a very public display of support for general practice by government in last year’s budget.
What this year’s budget says it that the government feels like it’s patched up its political wounds as far as general practice is concerned and it can coast for a bit now.
That Mr Butler seems to be drinking his own Kool-Aid on bulk-billing trends has probably contributed to this stance. All the PR for the last few months has been that the government has stemmed the bleeding on bulk billing.
The decline of bulk billing was the government’s biggest political exposure following Professor Price’s call to arms.
It’s easily weaponised by health system stakeholders, and not just patients and GPs. State governments are regularly blaming bulk-billing decline now for increasing pressure on their hospital systems and private health providers are all over it, building out various, often virtual-based, paid service offerings to capture a market for non-Medicare care that always existed.
Has the government, for some unfathomable reason, not contemplated properly that the Medicare of old, the one where everyone somehow thought GPs were for free, paid for by our good government, is mostly over, never to come back?
It does not seem feasible because of all the people who must have realised Medicare as we knew it for GPs was finished, it would be the government. Because, by freezing GP pay for 10 years they created a gap in income they knew they could never catch up.
So what might be going on here?
It looks a lot like, understanding that they could never catch up GP pay to sustain the old Medicare bulk-billing paradigm, the call to abandon bulk billing, while disturbing at first, presented the government with a unique opportunity: co-payment for GP services where with a bit of luck the government wouldn’t get blamed too much.
It’s not like past governments haven’t floated the idea of patient co-payments for GP services. In this case it wasn’t their idea so presumably they weren’t going to cop the flak they did last time they tried. The government could even stand back and say they were somewhat horrified by what GPs were doing.
But things spun out of control politically anyway so the government had to do something. That something was last year’s budget and a much-boosted triple bulk-billing incentive.
Clearly everyone couldn’t afford a co-payment and if they didn’t step in and help at the lower end they might end up with a riot – on the patient side because so many lower income families were falling through the cracks, on the GP side because they were actually getting mad that the government was making them subsidise these groups when times were tougher than ever, and on the state government side because a lot of these patients were working out that ED was free and they could wait the seven hours or so to get their chronic care problems seen to in some way.
The tripled bulk-billing incentive was understandably much appreciated by GPs, especially those in the country where the gap was smallest, because it meant they didn’t have to face off to their most disadvantaged patients and ask for money or lose them altogether and face the ongoing guilt of that.
What the RACGP, the AMA and ACRRM may now need to contemplate is that this is the new federal government strategy for renumerating general practice: a two-tiered system where GPs now manage most of their pay increases through mixed billing the patients they think can afford it, and a top up at the lower end via the tripled bulk-billing incentive, even though there is still a gap in that payment between reasonable remuneration or not.
In this model, Medicare rebates outside of tripled bulk-billing will likely never exceed CPI going forward, if they even meet it.
No catch up.
In other words, GPs take most of the load for building income with cost of living and other extraneous expenses (payroll tax for instance), and a significant amount of the risk of being blamed by patients in the longer term.
If it turns out that we are indeed in this new paradigm, then the government’s budget treatment of GPs is entirely explainable: the government thinks they have a new model where GPs make up the shortfall in their income going forward via mixed billing the patients they can, and it will do what it needs to – pick up the low-income patients and stave off any potential riot.
Figures on the growth in the average gap payment being charged by GPs in the last year released by the DoHAC earlier this week seem to support this theory.
The gap fee GPs are charging for the March quarter has risen about 10% for a B consult and a bit more for a C consult year on year.
That’s a trend that everyone needs to keep an eye on. It’s not being caused by anything extraneous like payroll tax because that has not kicked in anywhere yet. That it’s outpacing cost of living by quite a bit suggests GPs are adjusting their income as they can.
And there may be some way to go yet.
The bulk-billing trend of course is possibly the most important swing factor here in terms of the politics.
Early in the year the government was very quick to jump on the stats for December, the month after the tripled bulk-billing incentive started. The figures indicated that the long slide in bulk billing had stopped and, in the month of December, even experienced an uptick of 2%.
The government press releases were predictable. This one for instance arrived just over two weeks ago:
“Five months of official Medicare billing data shows after a decade of cuts and neglect from the Liberals, the slide in the GP bulk-billing rate has stopped and bulk billing has now stabilised, since the Albanese Government tripled the bulk-billing incentive.”
The release was accompanied by this chart which on the one hand neatly articulates the stop in the slide since the tripled bulk-billing incentive came in but on the other wholly misleads anyone by suggesting it’s all over red rover, battle won.
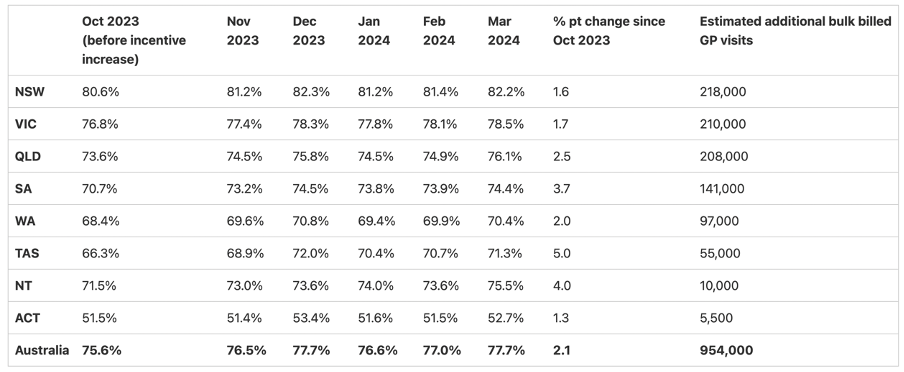
It might have been a little more transparent to put the chart below, also produced by DoHAC from the Medicare stats to the end of March, next to this chart above, as some sort of sanity check on what is really going on here.
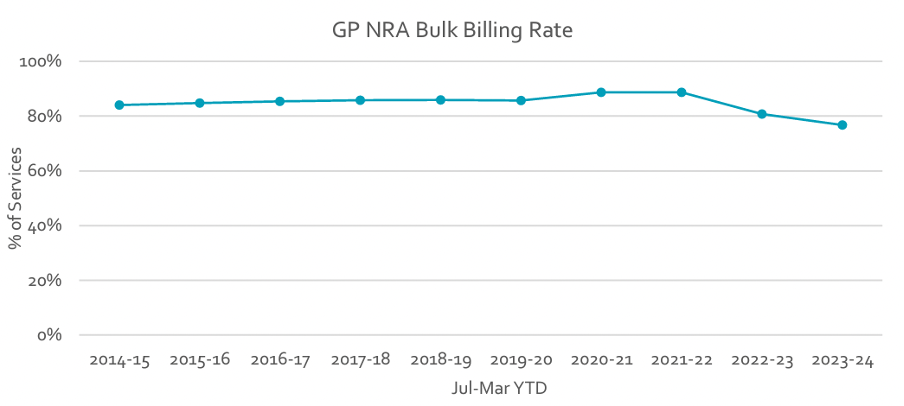
So far all you could say really about the government’s tripled bulk-billing initiative is that it’s a sugar hit that has slowed down a steep rate in decline of bulk billing, but regardless it’s at its lowest rate in decades.
It’s a pretty big call for the government to suggest it’s all over given this context. Add to this the significant financial pressures that GPs are going to face over the next couple of years, not least among them addressing payroll tax in some way across the board (many are threatening a flat $12 fee increase to their gap), and we almost certainly are going to see robust growth in gap fees.
More likely than not, we will also see a resumption in the decline in bulk-billing rates when the one-off tripled bulk-billing sugar hit has been absorbed in the system and GPs keep testing the boundaries of patients’ preparedness to pay for service directly.
In no way can anyone be calling the end in the decline of bulk billing on these numbers. We don’t have enough data.
If we are in this new paradigm, and last year’s budget was a false dawn, GPs need a better plan.
One that continues to participate in the normal pageantry of engaging with Canberra and pretending to play nice with each other for the greater good, but in which behind the scenes there is some serious off-the-book riot-like planning.
Maybe not actual riot planning, but at least for some bold tactical political plays that engage patients and other key stakeholders in the fight in the sort of hugely effective manner that Professor Price’s call to abandon bulk billing did from 2022 onwards.
GPs still underestimate and underplay their position in this game.
Although times are tough, and despite all the drama surrounding payroll tax, no GP is going broke any time soon.
There’s a pretty big supply-and-demand problem out there that isn’t going away for years to come.
With GPs in short supply and increasingly working out how to play the problem of extracting enough money to make a living outside of a now broken Medicare bulk-billing paradigm, while keeping the goodwill of their patients, GPs have leverage.
When push comes to shove, patients tend to like their GP a lot, and aren’t blaming them for having to pay them a gap fee mostly.
The AMA, the RACGP and ACRRM need to work on this dynamic in much smarter ways moving forward.




