Bulk-billing rates are a fantasy, but one the government loves to promote, so it can keep rebates low and GPs under pressure.
The government would have us believe that almost 90% of Australians do not pay out-of-pocket costs when they see a GP.
In 2016 the RACGP challenged this statistic on the back of a cross-sectional study which found less than 69% of patients did not pay an out-of-pocket amount at the GP. I was recently quoted as saying that legal bulk-billing was more likely around 30% (I was not referring just to GPs). So where does the truth lie?
For context, academics who believe leakage from heath financing systems is able to be accurately measured, say that no country will have less than 7% leakage caused by fraud and billing errors. Precise quantification has always proven elusive because the problem is often not what you can see, but what you cannot see. In Australia, estimates since Medibank (later Medicare) began have ranged from as low as 2% to over 25% of the scheme’s total cost.
My research concluded that the incidence of non-compliant billing would now be much higher than all previous estimates, but the causes of the problem are principally system issues rather than deliberate abuse.
Ultimately, determining whether billing errors are deliberate or innocent is less important than finding solutions to stop as much incorrect billing as possible, and bulk-billing is a good place to start.
I regularly receive emails like this (a full screenshot is at the end of the story):
Thank you for getting back to me.
My mistake: When I started bulk billing plus receiving gap payment, I still bulk-billed my clients instead of charging them the full amount and getting them to claim the Medicare part. I did this due to the advice I received from PRODA/HPOS online claiming program. They advised just to write the full amount into the cost field and that Medicare will know what the difference is.
After participating in Margaret’s webinar I realised my mistake and promptly changed how I bill.
However, recently I received this from a client:
Hi [redacted],
As discussed, the Medicare advised that there has been errors entering the service in the Medicare provider system.
I here provide a screen shot of the record.
The Medicare will required [sic] all the invoices show ‘a balance $0 and state ‘paid in full’ sent to them in order to correct the record.
Thank you and I appreciate your help.
Regards,
S
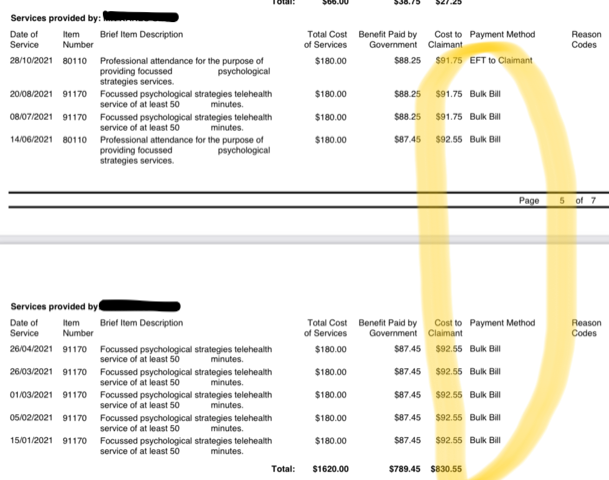
Here the patient includes a screenshot of their Medicare record, with eight payments in the “cost to claimant” column of around $90, and next to each of them in the “payment method” column, “Bulk Bill”.
The provider continues:
So I assume my mistake is showing up the Medicare end.
Hope this helped clarify my situation.
I need advice how to proceed with this.
What you can see is a confused patient offering up their Medicare records to show that each service was bulk-billed, but they also paid for the very same services. How is that possible?
Before you cry fraud, read the emails carefully. There is no evidence of criminal intent to defraud. In fact, the opposite appears true. The provider describes being led into unintentional error by the government, and has made immediate attempts to correct their error and change the way they bill.
I see this type of confusion often, and when I explain the very serious illegality of this conduct, some providers are so devastated they ask me whether they should immediately hand themselves in to the police.
Others say things like “everybody does it so it can’t be illegal”.
I assume those providers continue to bulk-bill and charge separate gaps, undermining the integrity of the entire Medicare scheme and destroying any hope of the government increasing rebates. Why would they when 90% of patients are apparently not paying?
Unfortunately, ignorance around correct use of Medicare is so great that many providers, like the one who sent the email, mistakenly believe that it is legal to bulk-bill and charge a separate gap at the same time. It’s not, unless paying for a non-PBS vaccine, or sometimes if multiple items are claimed. It also doesn’t matter what you call it (admin fee, booking fee etc.) or whether a separate legal entity charges it – it is still illegal.
In 2006 a GP was found guilty of 96 counts of criminal fraud for bulk-billing and charging a separate fee, but now, instead of calling the AFP, the government turns a blind eye. You can see that the government has apparently instructed the patient to ask the provider to reissue the accounts so they can square everything up on the Medicare end.
Most of the time this illegal activity flies under the radar because very few people check their Medicare records, and even if they did, most would not understand what they see. However, sometimes a patient does what the patient in the email did and tries to claim a rebate from Medicare only to find no rebate is payable because the claims were bulk-billed. That’s when things usually go pear shaped.
Recently, a nurse practitioner told me she charges all her patients $20 and then bulk-bills them saying “It is definitely permitted because I have checked”; a geriatrician disclosed that he charges his patients $90 and then bulk-bills an almost $500 MBS item, saying “At least 10 of my colleagues all bill this the same way, so they’ll have to put us all in jail”; the CEO of a practice management software company (one of the big four) told me that bulk-billing and issuing a separate concurrent invoice is everywhere across his massive database; a primary healthcare client asked my team to “Please stop emailing copies of the signed bulk-bill vouchers to patients because we also charge them”; and I am struggling to keep up with requests to run training sessions for professional organisations where the convenors ask me to “Please explain to them that bulk-billing and charging a gap is illegal because they’re all doing it”.
We know that Medicare billing is profoundly complex, and it is not always easy to know what is right or wrong. But if we want to repair and responsibly modernise Medicare, we will need to address the realities of widespread non-compliant bulk-billing, because bulk-billing is the linchpin that keeps Medicare afloat.
Unlike a lot of Medicare law, the bulk-billing law, Section 20A of the Health Insurance Act 1973, is actually quite straightforward. It provides that if you bulk-bill you accept the government rebate “in full payment” for the service provided. So, providers who bulk-bill and charge separate gaps are either ignorant or fraudulent – there is no third option.
In terms of what the true bulk-billing rates are, it’s actually quite easy to measure if we want to. It’s easy for patients to monitor this when they’re given a simple, clear instruction on what to look for – many came out of the woodwork after a recent article in The Guardian, saying they could see that the “cost to claimant” column on their Medicare records showed $0 but they know they paid.
For anyone still in doubt about the illegality of bulk-billing and charging a gap, I ask you to consider Tony Abbott. Whatever you may think of his politics, he would not have put his government through the agony of the failed 2014 $7 co-payment debate if co-payments were already legal.
Dr Margaret Faux is a health system administrator, lawyer and registered nurse with a PhD in Medicare compliance, and is the CEO of AIMAC, which offers courses and explainers on legally correct Medicare billing.