‘Value-based healthcare’ has a sting in its tail, especially for general practice.
As a senior medical educator, I was often responsible for training new medical educators in GP training.
They would come to me to discuss the feedback they’d received when presenting compulsory educational sessions on mental health, communication skills and professionalism. Often, the feedback was not based on their knowledge, skill or educational delivery, it was based on what learners thought about the topic. “Want better outcomes?” I used to say: “Teach dermatology.”
In recent years, we have been hearing about “value-based healthcare”. The idea is not that we make sure healthcare is as cheap as possible, although cost is obviously important; the idea is that we invest in things that make a difference to patients, and stop investing in things that don’t.
The idea has merit. The process involves identifying a population with shared needs, like people with type 2 diabetes, finding out what matters to them and working to achieve the best patient-centred outcomes you can with the resources you have. This approach often results in innovative solutions that get better outcomes for lower costs in a defined segment of the patient population.
The problem with value-based healthcare, though, is that it often doesn’t measure the impact on healthcare as a whole. We see this with cancer care centres. These centres provide holistic, patient-centred care, and achieve great outcomes, partly because cancer can mobilise the community to raise money to supplement government budgets. Cancer is a “high-prestige disease”, one which can attract research funding, government grants, and community support. However, every dollar that is invested in cancer means a dollar less for diseases that are low-prestige, even if those diseases have similar morbidity and mortality.
Patients with rare diseases, unpopular diseases like inflammatory bowel disease, or stigmatising diseases like alcoholic liver disease often receive less support than they deserve, because money is funnelled elsewhere. Put simply, if I want my patient to have better outcomes through timely, effective and affordable multidisciplinary services, I hope they have a common, high-prestige disease.
We see a lot of value-based healthcare initiatives, particularly in hospitals, that achieve impressive outcomes. Usually they are around well defined, common diseases (diabetes, heart disease), symptoms (headache) or procedures (hip replacement). However, we do not see, measure or evaluate the impact these relatively narrow initiatives have on the broader system.
This is a serious problem in general practice. We know that focussing on a “segment” at an individual level doesn’t necessarily achieve best outcomes for the whole person. We optimise 84-year-old Mrs Jones’ blood pressure, and she falls and breaks a hip. We manage 16-year-old Anna’s type 1 diabetes effectively, and don’t register that she has developed an eating disorder.
On a health system level if we continue down the value-based healthcare road, general practice may “achieve” lower and lower “outcomes”. Why?
Value-based healthcare only works if you choose a segment that has roughly uniform needs. If you select all the patients with type 2 diabetes, for instance, you can achieve great outcomes for them, by standardising best practice care, treating a lot of patients efficiently and engaging in continuous quality improvement. This works – if you exclude the complex patients from your segment.
This is the problem: if you create multiple segments in your health service, general practice will inherit the patients who are excluded from all of them.
Our practices are already full of complex patients who are inherently more expensive to treat and whose outcomes are difficult to measure. These patients will not achieve great outcomes on any standardised metric, because trade-offs need to be made: I have to sacrifice a “perfect” blood pressure to focus on reducing the risk of falls. Frankly, these patients need bespoke solutions to their complex problems. Putting the most expensive patients in the health sector into primary care (which has the lowest funding) and expecting good outcomes on irrelevant metrics is not only unrealistic, it is also quite depressing. It is impossible to defend our value to the health system when we are absorbing the unmeasurable tasks.
It is possible to achieve value-based healthcare outcomes in general practice, of course, by defining segments as “patients with frailty” or “patients with chronic disease” or “patients with multimorbidity”, and these initiatives have been successful, grounding the idea of creating ‘healthcare homes” that use effective and efficient team care arrangements and better remuneration structures to reward best practice.
However, the more segments we define, the greater the risk that patients will be involved in competing segments, or fall between their remit.
Every value-based healthcare initiative that is funded by the public purse ought to be able to answer the following questions:
- What services can be accessed by patients who are NOT suitable for this initiative, but still have significant needs?
- Are there demographic differences between the patients who are accepted into the team, and those who are not? We may achieve better outcomes, but we may well be sacrificing a commitment to equity if we don’t deliberately examine our own systemic bias.
- What do we do with patients who cross multiple segments? Who is co-ordinating care?
- What burden are we placing on patients and carers to navigate these increasingly complex systems, and does the benefit of the multiple multidisciplinary teams outweigh the cost to the system, patient and carer?
- When does generalist care achieve better and more cost-effective outcomes than multiple intersecting teams?
The following flowchart illustrates why I believe the value-based healthcare movement is an increasing problem for GPs by concentrating the complexity into general practice.
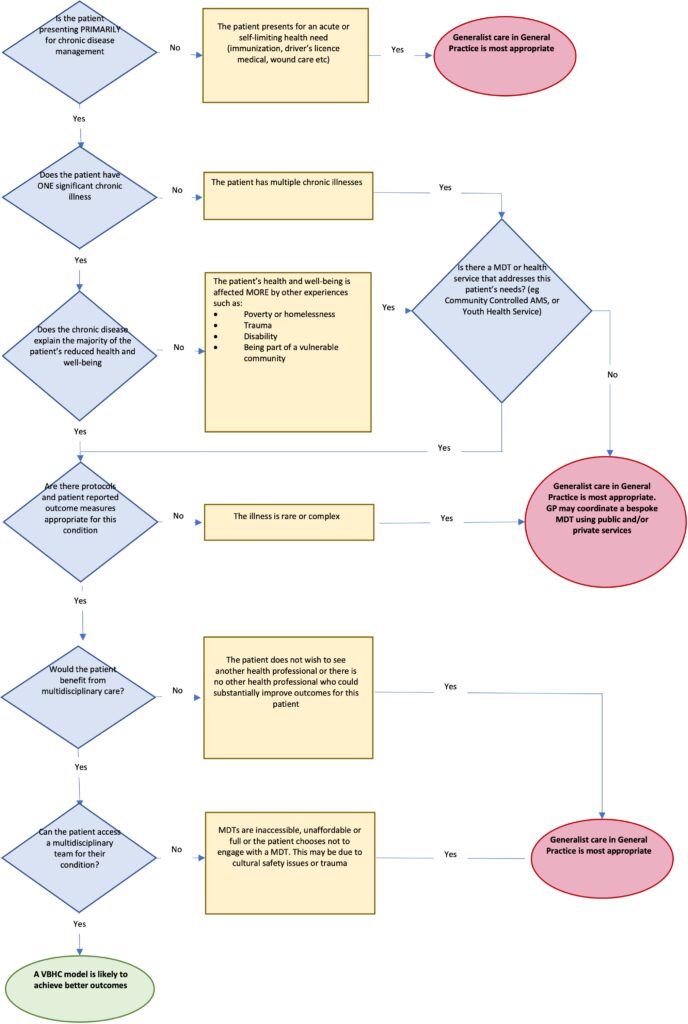
Value-based healthcare and primary care
If we continue to absorb the patients value-based healthcare initiatives reject, and continue to provide bespoke solutions to their complex healthcare needs within an off-the-rack budget, our businesses will no longer be viable.
Perhaps this is part of the reason why we will have a national shortage of around 11,000 FTE GPs by 2030.
The other reason is that the structure of the MBS means every complex patient reduces our financial viability. Longer consultations mean lower rebates.
The only way I can see value-based healthcare delivering better patient-centred outcomes for a lower cost in an entire population is to channel the savings from simple segments with streamlined multidisciplinary solutions into complex care. Otherwise, some patients get excellent outcomes, which is great for the morale of the health service, but the patients who are rejected from care are not seen, not counted and not valued.
What’s more worrying is that in an environment where it is increasingly difficult to access GP care, and we have initiatives like the “nudge” letters from the Department of Health targeting GPs who work with challenging patient populations, it makes perfect economic, professional and self-care sense to focus your energy on patients with straightforward problems. Which explains why many GPs are joining the burgeoning dermatology industry and setting up specialised clinics that pay well, have measurable outcomes and let you sleep at night.
When the safety net of general practice for complex patients is gone, the whole system is likely to become less accessible, more expensive and less equitable. This is not value and not what universal healthcare is meant to be.
Dr Louise Stone is a GP practising in Canberra and an Associate Professor at the Social Foundations of Medicine Unit at ANU Medical School; she tweets @GPswampwarrior.



