While the pandemic may lead to more late-stage metastatic cancers, this tool could help.
Over the past 30 years, we have witnessed significant technological innovations in radiation therapy that have improved effectiveness, decreased side effects and expanded indications for treatment.
Modern computer technology used for treatment planning, coupled with advanced technological improvements to linear accelerators, have led to the development of new radiation therapy techniques, including image-guided radiation therapy, stereotactic body radiation therapy, stereotactic radiosurgery and proton beam therapy.
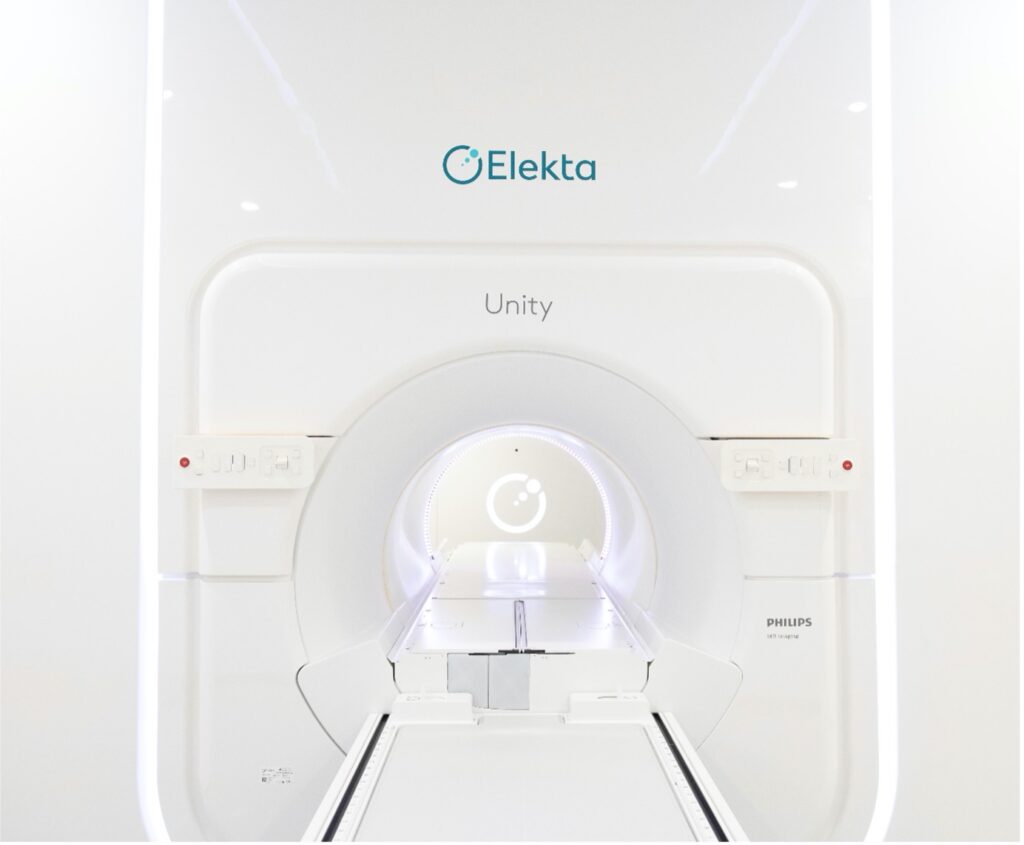
Globally, we are witnessing the implementation of the latest revolution in radiation therapy: the MRI linear accelerator (MR Linac), a technology combining a linear accelerator and an MRI to facilitate online MR-guided adaptive radiotherapy (MRgRT) in real time.
The first MR Linac was installed in Australia in 2019 in Queensland, and three other machines have since been installed, the latest of which is being installed at GenesisCare’s new integrated cancer centre at St John of God Hospital Murdoch in Perth, Western Australia.
A new era in adaptive radiation therapy
The MR Linac technology combines a high-field MRI scanner with a linear accelerator, a concept first presented by Raaymakers et al. in 2009.1 The MR Linac bolsters adaptive planning capabilities with simultaneous radiation delivery and real-time visualisation of high-resolution anatomical and biological MR images.2-5
Many tumours are located in organs that move during or between radiation treatment sessions. Often, tumours are located near sensitive organs or tissues, such as the bladder or bowel, which we want to protect during treatment. Precise, real-time imaging is therefore useful in determining the exact boundaries and location for effective treatment.2,5,6
The combined technology allows clinicians to visualise cancerous tissue during treatment in real time, adapting the plans and margins to minimise radiation exposure to surrounding healthy tissue.7
This highly personalised and adaptive care may result in reduced treatment-related side effects and fewer treatment sessions and fewer visits to the hospital, thereby reducing the overall burden on patients.2-4
Early real-world evidence from Australia
The first real-world experience of MRgRT using an MR Linac with a fully adaptive workflow in Australia was recently published in the Journal of Medical Imaging and Radiation Oncology by colleagues from St Vincent’s Hospital in Sydney.8
The team’s early experience demonstrated that training, the creation of a detailed workflow from patient selection, data collection and review of online treatment accuracy are paramount to establishing a new treatment programme such as the MR Linac. It is also noteworthy that implementation of such a complex program involves input from a multi-disciplinary group, as outlined by colleagues from the Odette Cancer Centre, Canada, from their initial experience.9
The ADAPT MRL Registry
As part of a strategic partnership between GenesisCare and Elekta, teams at GenesisCare St Vincent’s and GenesisCare St John of God Murdoch are participating in ADAPT-MRL, a long-term prospective and retrospective registry that will collect patient-reported outcomes and follow-up data from patients who have received treatment on the MR Linac, to promote the ongoing clinical development of adaptive therapy based on real-world data and evidence. 10
Leveraging our global network of treatment centres, GenesisCare will collect real-world data that will inform future advancements in adaptive therapy technology.
The MR Linac – front & centre on the global stage
At the recent American Society for Radiation Oncology (ASTRO) Annual Meeting, a total of 22 abstracts were presented, highlighting the technical capabilities and clinical benefits of MR-guided radiation therapy.
One to highlight would be the abstract Real-Time Motion Tracking based on Orthogonal Cine MRI During MR-guided Radiation Therapy for Prostate Cancer, which demonstrated the feasibility of tracking intrafraction prostate motion in real-time using 2D cine and 3D MRI images during MRgRT, without the need for fiducial markers.11
The study essentially concluded that with further investigation and careful workflow, real-time motion-tracking strategies might be implemented in MRgRT to manage motion during treatment delivery. This abstract was awarded the ASTRO Recognition award.
Colleagues at the Miami Cancer Institute recently presented their experience using an MR Linac to treat patients with inoperable pancreatic cancer at the 2021 European Society for Radiotherapy and Oncology (ESTRO) in Madrid. The typical median survival time for patients with inoperable pancreatic cancer is 12-15 months. For patients treated with MR-guided adaptive therapy on an MR Linac, the median survival was significantly improved to 21 months. These are exciting real-world data results that need to be confirmed in randomised studies.12
The future of adaptive radiation therapy
Adaptive radiation therapy is a promising emerging treatment paradigm, and the integration of MR imaging capabilities into linear accelerators is setting a new benchmark for innovative cancer treatment on a global scale.
As we start to contemplate what a “post-pandemic” world would look like in the world of oncology, sadly, we know we will see more patients presenting with late-stage metastatic disease, as a result of delays to early diagnosis and treatment.
Technologies such as the MR Linac, as well as innovative new service models such as the integrated cancer care model, will have an increasingly important role to play in ensuring the best possible clinical outcomes and quality of life for patients with complex, hard-to-treat cancers.
Dr Hendrick Tan is a radiation oncologist for GenesisCare in Western Australia and works across GenesisCare’s Perth centres and regional centre in Bunbury. He will be joining the team at GenesisCare’s new integrated cancer centre at St John of God Murdoch Hospital when it opens its doors to patients in December 2021. Dr Tan completed his Bachelor of Medicine and Surgery at the University of Western Australia and began his medical career at Royal Perth Hospital. He then went on to undergo specialist training in radiation oncology at Sir Charles Gairdner and Fiona Stanley hospitals.
Following this, Dr Tan undertook a clinical research fellowship at the Sunnybrook Odette Cancer Centre in Canada in the field of neuro-oncology, thoracic oncology, stereotactic ablative radiation therapy (SABR) and MRI Linac technology. Here, he published work and presented at international meetings. A keen researcher, Dr Tan has a strong desire to pursue research activities in new treatment and imaging technologies to improve patient outcomes.
Dr Tan is also closely involved in teaching and education. He was a clinical oncology lecturer at UWA and a clinical examiner for radiation oncology residents at the University of Toronto. He was also awarded the “Excellence in Clinical Teaching Award by a Clinical Fellow” from the University of Toronto through his involvement in teaching the radiation oncology residents.
References
- Raaymakers BW, Lagendijk JJ, Overweg J, Kok JG, Raaijmakers AJ, Kerkhof EM, et al. Integrating a 1.5 T MRI scanner with a 6 MV accelerator: proof of concept. Phys Med Biol. 2009;54(12):N229-37.
- Hall, W.A., et al., The transformation of radiation oncology using real-time magnetic resonance guidance: A review. Eur J Cancer, 2019. 122: p. 42-52.
- Bertelsen, A.S., et al., First clinical experiences with a high field 1.5 T MR linac. Acta Oncol, 2019. 58(10): p. 1352-1357.
- De Leon, J., Stricker, P. & Jameson, M. Towards MRI-guided personalised radiation therapy. 2020; Available from: https://insightplus.mja.com.au/2020/20/towards-mri-guided-therapy
- Kerkmejjer, L.G., et al., The MRI-Linear Accelerator Consortium: Evidence Based Clinical Introduction of an Innovation in Radiation Oncology Connecting Researchers, Methodology, Data Collection, Quality Assurance, and Technical Development. Front Oncol, 2016. 6:p. 215
- Milano, M.T., et al., Oligometastases: history of a hypothesis. Ann Palliat Med, 2020.
- Winkel D, Bol GH, Kroon PS, van Asselen B, Hackett SS, Werensteijn-Honingh AM, et al. Adaptive radiotherapy: The Elekta Unity MR-linac concept. Clin Transl Radiat Oncol. 2019;18:54-9.
- De Leon, J., Crawford, D., Moutrie, Z., Alvares, S., Hogan, L., Pagulayan, C., Jelen, U., Loo, C., Aylward, J.D., Condon, K., Dunkerley, N., Heinke, M.Y., Sampaio, S., Simon, K., Twentyman, T. and Jameson, M.G. (2021), Early experience with MR-guided adaptive radiotherapy using a 1.5 T MR-Linac: First 6 months of operation using adapt to shape workflow. J Med Imaging Radiat Oncol. https://doi.org/10.1111/1754-9485.13336
- B.M. Keller MC, M.E. Ruschin, A. Kim, C. McCann,, A. Lau HS, D. Vesprini, J. Detsky, C.L. Tseng. MR-Linac Radiotherapy in Year One: Experience’s in Imaging,Patient Treatment and Data Collection. International Journal of Radiation Oncology Biology Physics. 2020;108:e249-e50.
- Jeremiah de Leon, Amanda Woods, Tania Twentyman, Michael Meade, Vicki Sproule, Smitha Chandran, Joseph Christiansen, Neil Kennedy, Maria Marney, Kris Barooshian, Michael Plit, Jayd Lynch, Raj Jagavkar, Helen Ormandy, John Christodouleas, Florian Pietzsch, Michael Chan, Michael G Jameson, Analysis of data to Advance Personalised Therapy with MR-Linac (ADAPT-MRL), Clinical and Translational Radiation Oncology, Volume 31, 2021,Pages 64-70,ISSN 2405-6308, https://doi.org/10.1016/j.ctro.2021.09.004.
- Jassar. H, Tai. A, Chen. X, Keiper.T et. Al, Real Time Motion Tracking Based on Orthogonal Cine MRI for Abdominal Tumors on 1.5T MR-Linac, 2021, https://w4.aapm.org/meetings/2021AM/programInfo/programAbs.php?sid=9269&aid=57278
- Chuong. M, Mittauer. K, Herrera, R. Romaguera, T. ESTRO Abstract 2021. Long-long term outcomes of MR-guided SABR & on-table adaptive replanning for unresectable pancreas cancer, https://www.estro.org/Congresses/ESTRO-2021/502/profferedpapers25-uppergi/3760/long-termoutcomesofmr-guidedsabr-on-tableadaptiver