When it comes to combatting cancers, are we overlooking a powerful form of protection that's already available?
Countless dollars are being spent in finding a cure for cancer, but we may be overlooking a powerful form of protection already available.
“During an era when physicians are called on for action to find a cure for cancer, we tend to forget that we have available at our disposal a human papillomavirus (HPV) vaccine that prevents multiple types of cancers,” wrote the authors of a JAMA editorial.
The time has now come for a new generation of vaccines that also cover cancer-causing, but non-sexually transmitted HPV subtypes, according Dr Jad Chahoud, a haematology-oncology fellow at the Anderson Cancer Center in Texas, and colleagues.
In particular, a growing body of evidence now links beta-HPV types to cutaneous squamous cell carcinoma and oropharyngeal cancers in the immuno-competent population.
Alpha-HPVs, which play a role in types of cervical, vulvar, vaginal, anal, head, neck and penile cancers, infect mucosal epithelial cells.
But beta-HPVs infect cutaneous epithelial cells, so can be transmitted through casual contact, including between children.
“Such an HPV vaccine protecting against beta-HPV subtypes would offer children precise prevention without being type-restricted, to prevent SCC and oropharyngeal cancers as well.”
The causal link between beta-HPVs and these cancers had been well established in immunocompromised patients, meaning a vaccine would provide protection for those undergoing organ or bone marrow transplant, on chemotherapy, or have HIV, who were around 65 times more likely to develop beta-HPV-related SCC, the authors said.
The protection of transplant recipients and HIV-infected individuals alone “should constitute a major goal for precision in cancer prevention and our global fight against cancer”.
“The next generation vaccine would probably provide herd immunity against a larger spectrum of HPV types. The aforementioned differences between the current and next-generation vaccines break a couple of the barriers that policy makers face in rendering HPV vaccination mandatory.”
While the evidence linking beta-HPVs to SCC and OPC was strongly suggestive but not conclusive, researchers had started working on alpha-HPV vaccines long before conclusive evidence of causality, they wrote.
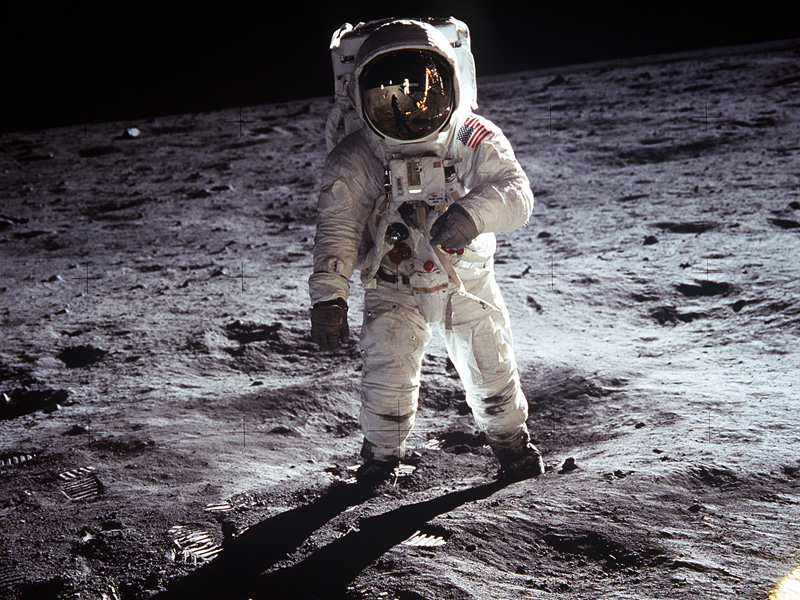
“This vaccine constitutes a true moonshot; it is our collective duty to render cancer prevention a priority and focus our efforts on providing a non–type-restricted HPV vaccine to every child.”
Divorcing the vaccines from sexually-transmitted diseases would also help to weaken parental and religious opposition, such as in the US, improving vaccine coverage.
“We believe the next-generation vaccine protecting against non–sex-specific cancers, would strengthen the healthcare providers’ position and decrease parental resistance which would in turn increase male vaccination rates.”