A new CSIRO study highlights one of the potential public health risks of pharmacist prescribing.
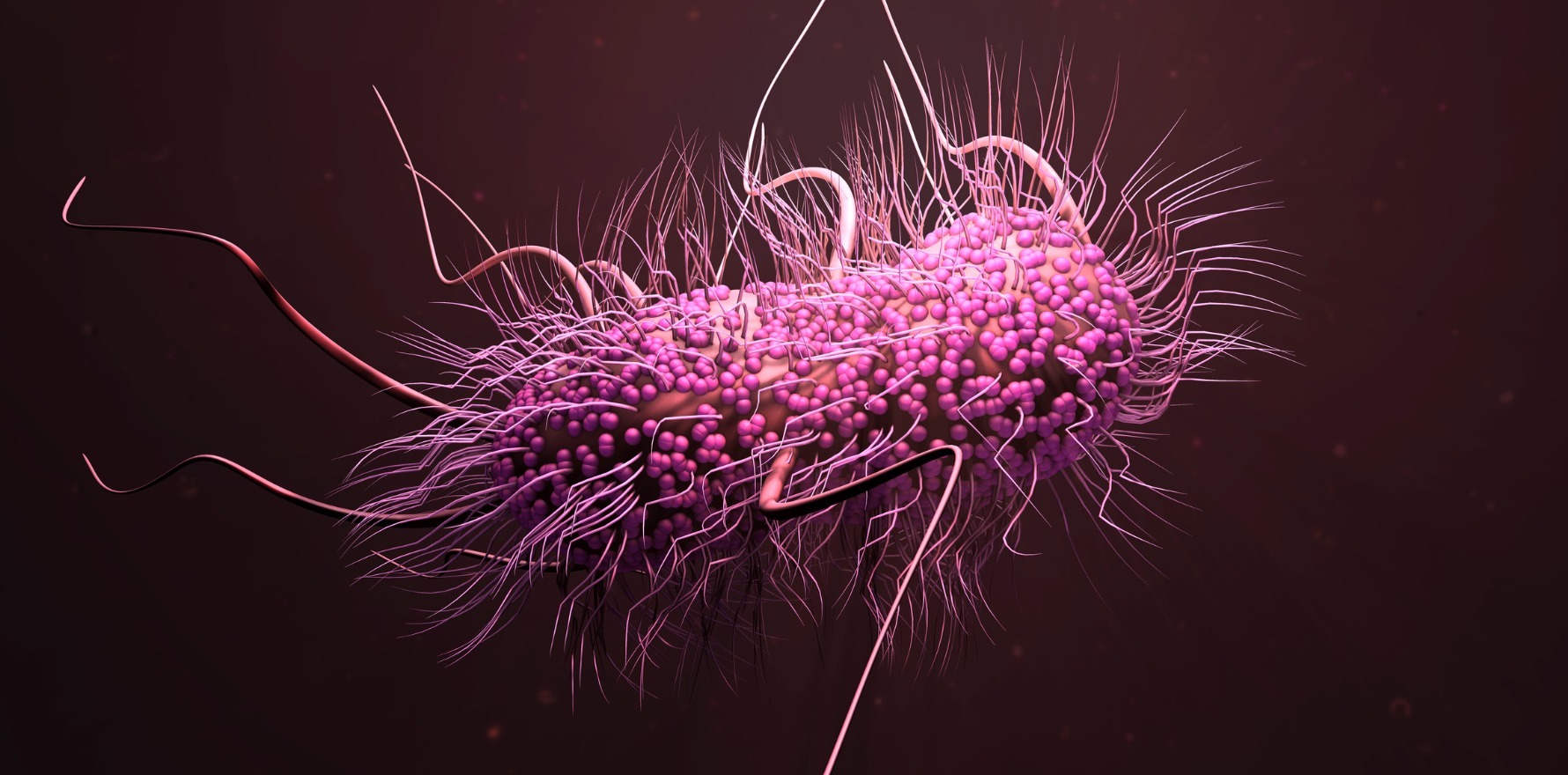
A recent CSIRO study has found the spread of drug-resistant bacteria in the community is increasing the risk of death for common infections such as UTIs.
The study, on mortality associated with community-acquired infections, comes as concerns grow about pharmacists’ prescribing antibiotics as part of Queensland’s UTIPP-Q pilot.
The high prevalence of UTIs makes them a major contributor to antibiotic use in Australia, said CSIRO research scientist and study author Dr Teresa Wozniak.
“Our study found patients who contracted drug-resistant UTIs in the community were more than twice as likely to die from the infection in hospital than those without resistant bacteria,” she said. “Without effective antibiotics, many standard medical procedures and life-saving surgeries will becoming increasingly life-threatening.”
The Urinary Tract Infection Pharmacy Pilot – Queensland (UTIPP-Q) – which commenced in June 2020 and has been extended to 30 June 2022 – allows trained community pharmacists to provide “appropriate treatment for uncomplicated urinary tract infections”, according to the Pharmacy Guild’s Queensland branch. This includes being able to supply trimethoprim, nitrofurantoin and cefalexin.
But Dr Krystyna de Lange, a Queensland GP, immediate past-chair of the RACGP National Faculty for GPs in Training and a former pharmacist, is concerned about the expansion of pharmacists’ scope of practice.
“We have pretty good data to show that in cases where medications move from prescription-only to over-the-counter, their use increases,” she said, “and it makes sense that if there’s increased access, there’s a corresponding increase in the provision of that medication.
“Unfortunately, that doesn’t always correlate with the patient’s need and appropriate provision.
“The evidence [shows] that with increased numbers of prescribers, with increased access, we do end up with increased use – and at a time when antimicrobial resistance is a global health emergency, that’s actually the opposite of what we want to be happening.
“We want really stringent antibiotic guidelines, we want really stringent use of antibiotics in appropriate settings and for appropriate reasons. So, the more we open up non-doctor prescribing for antibiotics, the more, unfortunately, we’re potentially going to see an increase in use and a corresponding increase in inappropriate use, which would be bad news for antimicrobial resistance.”
Queensland Health said antimicrobial resistance was covered throughout foundation pharmacy training programs. Since antimicrobials form key treatment choices for many acute and chronic conditions, pharmacists were trained to understand the impact of antimicrobial resistance on antibiotic choices, patient outcomes, and antibiotic monitoring and responses as part of their role as medicines experts within the health care team, the department said.
In addition to this underpinning knowledge, the training for the UTI pilot includes the epidemiology and pathogenesis of UTIs, clinical features and differential diagnosis of UTIs, the use of pathology testing, and antibiotic guidelines for treatment including antimicrobial resistance.
However, Dr de Lange said she believed the training for the UTIPP-Q pilot was not fit for purpose.
“The training that’s currently mandated for pharmacists to be involved in the Queensland UTI pilot is a short online module, which really promotes a kind of tick-box, flowchart style medicine,” she said, “rather than teaching the kind of clinical reasoning skills to enable non-doctor health professionals to correctly identify and diagnose, but also to consider other diagnosis ‘red flags’.”
Dr de Lange suggested that if pharmacist prescribing were to be an increase in scope of practice, working in a team-based, collaborative manner might be a preferred option. This could be as part of a multidisciplinary team, either in a hospital setting or with a general practitioner rather than the with the “fragmented and completely separate care” that occurs in the UTI pilot.
However, she had further concerns about the proposed extensive North Queensland Pharmacy Scope of Practice pilot, which would allow pharmacists to diagnose and treat more than 20 medical conditions.
“Some of these include other infective conditions – for example, ear infections, and these are in some regions with a high proportion of Aboriginal and Torres Strait Islander patients, where there may be increased concerns around antibiotic stewardship and microbial resistance,” she said.
“So, the more you open up to different types of infections and different types of antibiotics, I would have increasing concerns over the long-term impact when it comes to complications like microbial resistance.”