Neurodegenerative diseases are among our greatest health risks. Here's everything you need to know about ALS.
Neurodegenerative diseases are one of our fastest growing health risks.
Most GPs will already know these figures are rapidly increasing, with the total number of people projected to be diagnosed with dementia expected to reach 82 million by 2030, and 152 million by 2050.
However, one of these diseases, amyotrophic lateral sclerosis (ALS), is more prevalent per capita in Australia than anywhere else in the world — something that is less well known. Here’s what you need to know about this disease.
What is ALS?
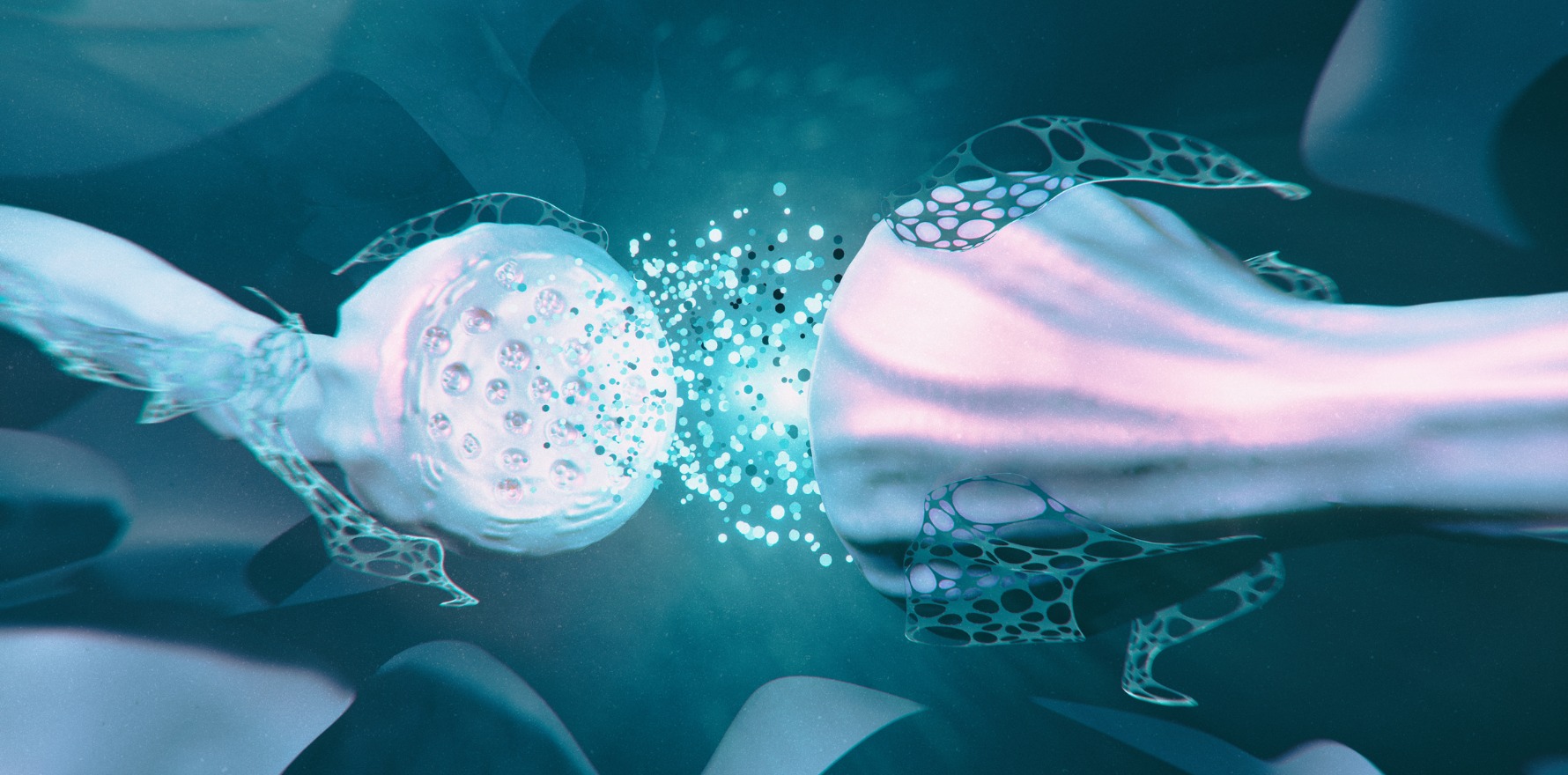
ALS, or classical motor neurone disease (MND) as it is commonly known, is a progressive neurological disease that affects the neurons responsible for controlling voluntary muscle movement. The disease is typically attributed to painless progressive weakness that steadily gets worse over time.
Most of the time, the disease progresses quickly, with survival rates averaging between three and five years from symptom onset. However, some patients experience “plateaus” where they appear to stabilise for years or even decades, and a very small number of patients recover from the disease.
How common is it?
In Australia, while ALS is uncommon, it certainly isn’t rare. Recent statistics show there are more than 2,000 people in the country currently diagnosed with the disease, and a further two are diagnosed each day, or around 730 people each year.
The disease can affect people of all ages, anyone from teenage years up to older patients. In Australia, the average age of onset is 50 whereas globally it is 60.
What are the tell-tale signs?
ALS is highly variable between patients and this can make it incredibly difficult to diagnose and treat. However, there are some tell-tale signs to look out for.
Early symptoms include atrophy (degeneration of muscle or nerve tissue), fasciculations (muscle twitches) and hyperreflexia (overactive or over responsive reflexes). In the early stages of the disease, there is generally no pain for sufferers and it doesn’t tend to affect a patient’s bladder control or senses. But as the disease advances, nerve cells are destroyed and the patient’s muscles get weaker. This eventually affects chewing, swallowing, speaking and breathing.
Often, when the weakness starts, it can typically be found in the patient’s hands, feet or limbs and then spreads to other extremities of the body. And about a third of the time, it can start in the bulbar muscles — the muscles of the mouth and throat, responsible for speech and swallowing. It’s also important to be aware that, very rarely, less than 3% cent of the time, the weakness can start in the respiratory muscles — such as the diaphragm and external intercostals.
What are the diagnosis and treatment options?
Currently, there is no single test that can confirm ALS within a patient – which can make diagnosis challenging. Typically though, the diagnosis is made through a patient’s history, an exam and an electromyography (EMG), which measures muscle reaction or electrical activity in response to a nerve’s stimulation of the muscle. This confirms the lower motor neuron disease while imaging and blood tests help to rule out mimics.
One of the most challenging things about ALS is that in most cases, the cause is never found – a situation called “sporadic ALS”’. For about 10% of cases, the cause can be identified as “genetic ALS” in which it stems from genetic mutations. Because we know so little about the disease, and there is currently neither a cure or prevention, it means treatments are focused on reducing the symptoms and improving the quality of life for those with ALS.
In the majority of instances, an individual with the condition requires support from numerous healthcare professionals including a GP, neurologist, occupational therapist, physiotherapist, speech pathologist, psychologist, home care nurse and social worker.
What does the future hold?
As professionals in the field, it has never been a more exciting time as researchers aim to find out more about this disease – everything from why it occurs to personalised therapy options.
One example is through studies conducted by GenieUs, referenced in Molecular Neurobiology, that found that a single and unique biomarker, hsa-miR-30b-5p, represents a common feature among patients with ALS. The company found that the genetic expression of the microRNA hsa-miR-30b-5p was consistently upregulated in the spinal fluid of ALS patients. Initial research suggests the microRNA strand prevents the action of natural processes used by the body to maintain healthy neurons, a key feature of neurodegenerative disease progression.
The hope is that by targeting hsa-miR-30b-5p, the progression of neurodegenerative diseases such as ALS can be significantly slowed or halted.
Dr Richard Bedlack is MS Professor of Neurology and Director of the Duke ALS Clinic from Duke University in North Carolina.
Matt Keon is CEO and co-founder of GenieUs with 20 years’ experience in the health sector including in telehealth, patient engagement and healthtech platforms.