The government’s after-hours review dances neatly around addressing two elephants: a highly fragmented approach underpinned by conflicting funding signals between tertiary and primary care.
As far as ticking boxes to give the impression you are tackling the really big issues of our creaking hospital and primary care system, the Government’s Review of After-Hours Primary Care Programs and Policy has probably done the trick.
It’s actually a great review of what is going on in after-hours care and what the problems are, particularly in respect of the challenge we have getting after hours primary care to somehow put a meaningful a dent into our burgeoning ED access issues. It’s worth a read and will be a good reference document.
But like a lot of other major healthcare system reviews we’ve seen in the last couple of years that initially threaten to address long term systemic system issues, this review timidly plays at the edges of existing initiatives and programs when it comes to any plans to alter the trajectory of what is in effect a pretty wasteful and fragmented approach to after-hours care in Australia.
To be fair to the expert committee who conducted the review (and did a good job summarising the problems) the government would not have given them any permission to wander outside the guard rails of our existing funding and policy frameworks. And if they had, you’d have to suspect that such ideas would never have seen the light of day.
Related
An example of such guard rails may have been the following:
“Commonwealth primary care after-hours policy settings, delivery strategies, infrastructure and administrative arrangements that provide the setting for MBS expenditure were within the Review’s scope. Specific MBS items were out of scope of this Review”.
One big part of the problem (elephant number one) is neatly summarised by the chart the review produced below.
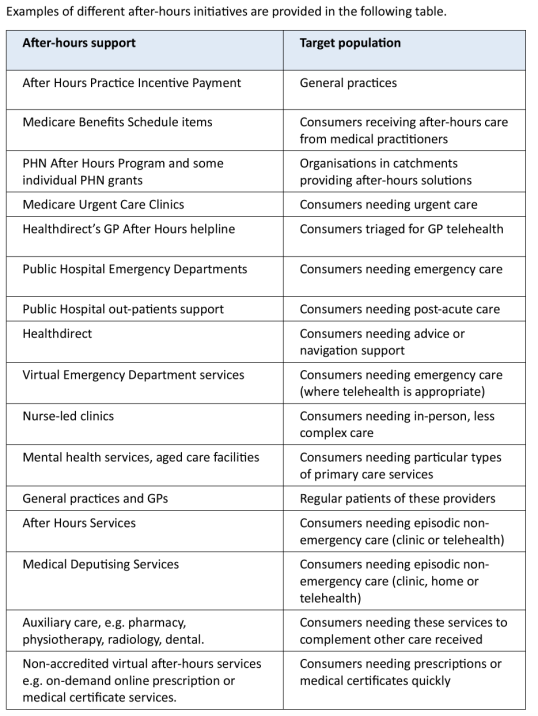
Another way of looking at this elephant is to look at how eclectic government funding to the after-hours sector is, again from the report, below:
• Approximately $521 million for around eight million services funded through the MBS1
• $92 million for over 6000 general practices claiming the After Hours PIP2
• $41 million for the PHN After-Hours program
• $35 million on Healthdirect’s Nurse Triage and After Hours GP Helpline, and
• $240 million on Urgent Care Centres (we added this last point, as it is in the list above but for some reason not mentioned in the funding summary).
If we add all that up, we are spending nearly $1 billion on after-hours care per annum which is quite a bit. It makes you suspect we may not be spending it all that effectively.
One thing that immediately stands out from both lists above, and which the review does at least identify in its own way, is the almost total lack of co-ordination between all of the above approaches to tackling the problem.
“The current system for after-hours care is complex, fragmented, and difficult to navigate, with issues affecting both consumers and primary care providers,” it says.
The key word being “fragmented”.
Two related key finding were that “incentives are insufficient, misaligned and act as a limiting factor for take up or entry by primary care services” and that “consumer pathways are fragmented, impacting continuity of care and with consequent safety and quality issues”.
If you read far enough into the review you will eventually come to a possible seed of a plan of attack to address fragmentation – “integrate after-hours primary care within an Urgent Care Framework”.
I say seed of a plan because those words are it as far as any actual plan is concerned in the review. It’s not so much a seed of a plan as a poorly articulated catch all phrase which may or may not be a good idea depending.
The review probably should have spent some time expanding on why building out an integrated urgent care framework is such a good idea, how you could do it and who would be involved (more on this below).
All the other key proposed reforms of the review are summarised as per below chart below.
The detail on why each other reform is important and how you might tackle them is similarly sparse in the review, which gives you a sense of how light the document is on actually doing something practical quickly.
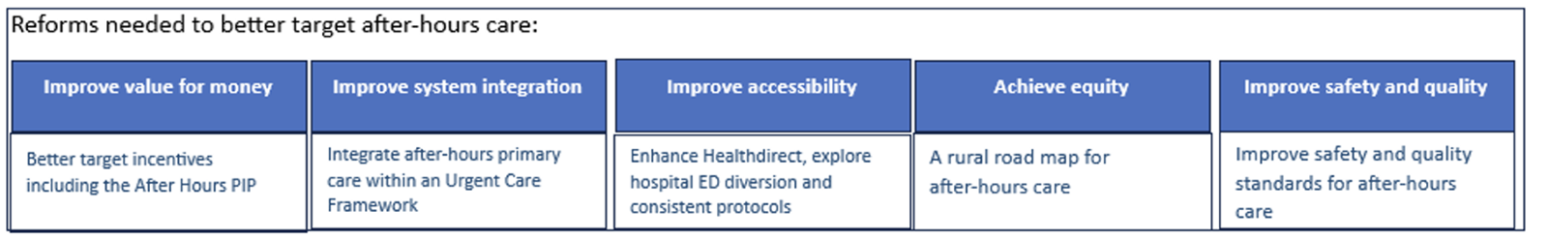
Like a lot of government reviews, we have identified five areas for action (you always need at least five) but not really provided any prioritisation of the areas in terms of what bang for your buck you’re going to get if you concentrate on one more than any of the others (or maybe two).
The standout area for return on effort from the five areas of reform addressed in the review is addressing the fragmentation, and the standout concept is developing a “National Urgent Care Framework”.
We don’t quite know what a National Urgent Care Framework is, but you can already imagine from the words, it could be something worthwhile given where we are today.
Which in a manner brings us to what might be this review’s second elephant in the room: it only really contemplated initiatives outside of the hospital sector using funding from outside the hospital sector.
A major reason for having a properly functioning after-hours care sector is to address the burden that a non-functioning after-hours sector is putting on our hospital system.
But the hospital system side of the equation and key hospital stakeholders are not really contemplated in the review.
Surely the states and hospital leadership should be front and centre in any ideas we are starting to have around a National Urgent Care Framework.
Part of the problem you suspect is our current funding paradigm.
The federal government is charged with funding the primary care sector (and other elements of non-hospital care such as aged care) to keep patients that don’t need to go to an ED or, to be staying in a hospital, out of hospital.
But perversely there are no funding signals for the hospital sector – where we spend a lot more money than primary care – to join in the party and help with the problem.
The hospital sector does get political and economic signals to try and help, notwithstanding.
But would it be too much to ask if the idea of a National Urgent Care Framework somehow addresses this elephant?
That of course feels like it is outside those guardrails we talked about above.
One aspect of the review that does go to addressing fragmentation practically and quickly, and which ironically bridges the divide between hospital and primary care funding, is its push to use Healthdirect more effectively across the whole system.
Healthdirect is a not-for-profit entity funded by all the states (bar Queensland for some reason) and the federal government with an objective of being a universal source of truth for directing a patient to the healthcare service they actually need first time they look, outside of them needing an ambulance (they will do that too if someone hasn’t called one but needs one).
In a manner this should make Healthdirect a bit of Switzerland in terms of how hospitals want to deal with ED presentations versus how all non-hospital services can deal with them.
Unfortunately, we aren’t there yet in terms of the hospital sector trusting Healthdirect to send them the right patients and we also have the odd problem with GP groups such as the RACGP thinking that it might be stealing patients from their traditional GP members via their virtual GP service.
But as far as an existing entity that is in a position to provide the system with some real and immediate leverage on much better triage between the community and hospital care after hours across the country, Healthdirect is it.
The expert review committee at least recognised this and recommends a lot more focus on leveraging this service in our plans moving forward.
Which makes you wonder just a little when you look at that eclectic funding mix, we mention above.
If you really think Healthdirect is in pole position to help the whole process move forward now, is $35m out of a the nearly $1 billion we spend each year on trying to make after hours work better, enough funding for this group?
Note: At 7pm tonight Health Services Daily is holding a one-hour webinar on our rapidly evolving ecosystem of healthcare provider virtual front doors, including a look at the idea, mooted by the After-Hours Review committee, that Healthdirect might be a candidate for a master entry point for all our virtual front doors. You can register for the webinar HERE. If you can’t make it, if you register we will send you a link to the webinar so you can watch it after the fact.