Sexual transmission really does play an important role in recurrence, a study finds, and it warrants a change in practice.
GPs should start treating male partners of women with bacterial vaginosis who are in a heterosexual, monogamous relationship, the RACGP chair of the sexual health special interest groups has told TMR.
The evidence from a new study conducted at the Melbourne Sexual Health Centre and published in the New England Journal of Medicine is enough to change treatment immediately, said Dr Sara Whitburn, who was not involved with the research.
“If you are seeing someone who’s having recurrent, relapsing bacterial vaginosis, and if they are in a monogamous heterosexual relationship, I do think that this article supports a change in treatment,” Dr Whitburn said.
The change will also require some patient and pharmacist support.
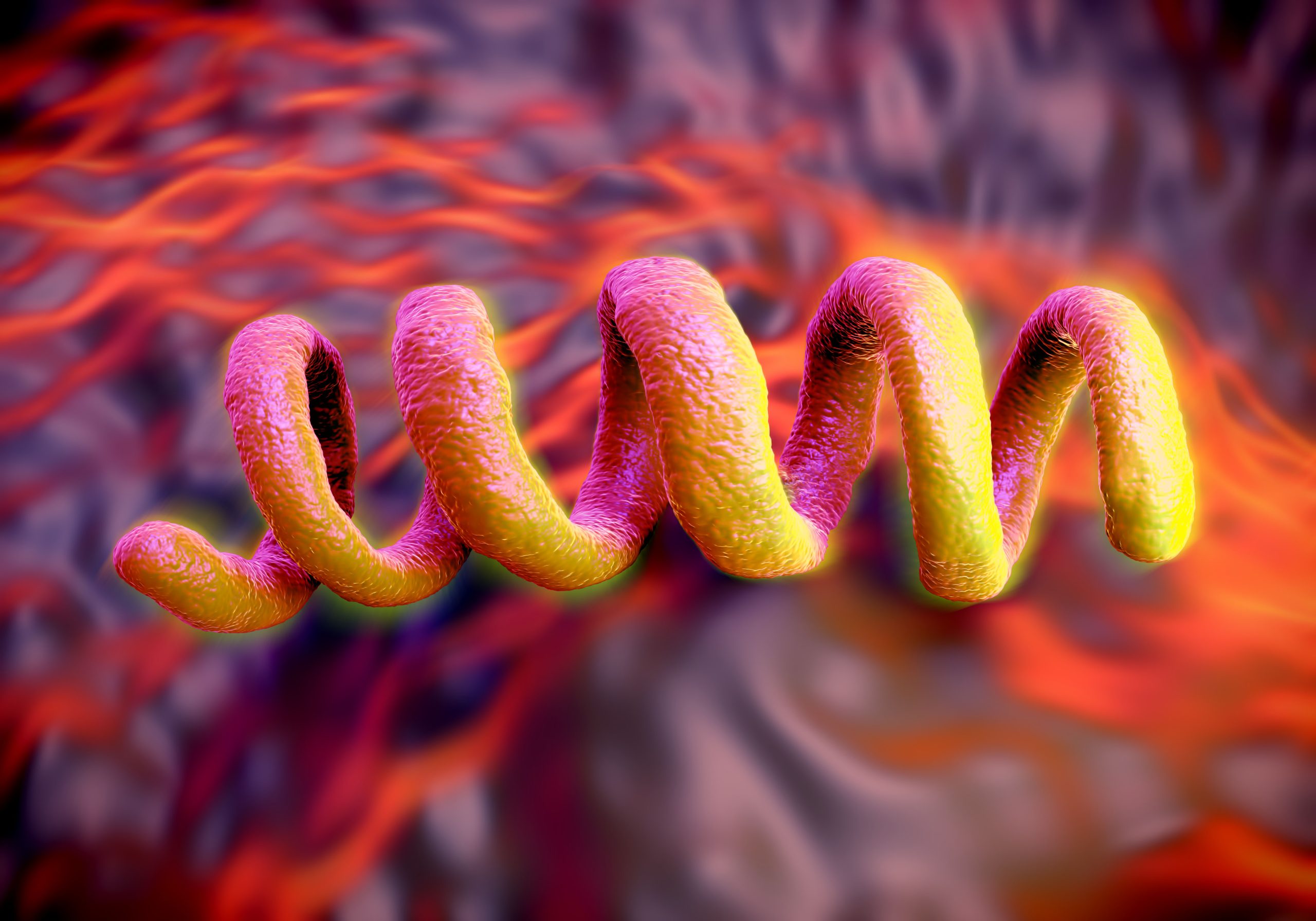
Bacterial vaginosis affects at least 12% of non-Indigenous and 30% of Indigenous women in Australia, and more than half of those treated will have a recurrence within three to six months. The condition increases the risk of acquiring HIV and STIs, and, in pregnancy, early labour, low birth weight and miscarriage. It affects quality of life and is a significant burden on the health system.
The standard treatment has been to give the person presenting with bacterial vaginosis metronidazole or clindamycin 2% vaginal cream. But the new research confirms the condition is sexually transmitted, and giving male partners oral and topical treatment (both are required) can interrupt the cycle of reinfection.
The researchers compared recurrence of bacterial vaginosis in two groups of female partners in monogamous heterosexual couples within a period of 12 weeks.
Related
In 81 couples, females were given standard treatment and males were given concurrent oral and topical treatment – metronidazole 400mg tablets and a 2cm diameter volume of 2% clindamycin cream, applied to glans penis and upper shaft, under the foreskin if uncircumcised, both twice a day for seven days.
In the control group of 83 couples only women were treated.
The trial was ended after 150 couples (69 in the treatment group, 68 in standard care) had completed the 12-week follow-up because the control group results were clearly inferior. The infection recurred in only 35% of the women in the treatment group, and in 63% of women in the group where the men were not treated.
Recurrent infection took a mean of 74 days to show up in the treatment group and just 56 days in the control group.
All the women and 86% of the men took at least 70% of their prescribed doses, with the lowest rate of recurrence in the partners of men who took all their treatment.
No serious adverse events were reported.
“Efforts to increase the likelihood of cure have been hindered by an incomplete understanding of the pathogenesis of bacterial vaginosis, although epidemiologic and microbiologic data show that it has the profile of a sexually transmitted infection,” the authors write.
Previous interventions in male partners which didn’t show a reduction in recurrence for the female partner used small samples, didn’t assess adherence to treatment and, importantly, used only oral antimicrobial agents to treat the men, “which may not be sufficient to clear cutaneous penile carriage of bacterial vaginosis-associated organisms,” the authors said.
“In order to promote clearance of BVAB (anaerobic BV-associated bacteria) from the male partner both oral and topical antibiotic therapy will be required. BVAB are detected in the distal urethra of males, a location well accessed by oral but not topical antibiotics. In contrast, the sub-preputial space and coronal sulcus (under the foreskin and in the groove under the head of the penis) are poorly reached by oral but well accessed by topical antibiotics.”
The topical treatment for men, clindamycin, is the same as the cream used for women, said Dr Whitburn.
“But you’re actually prescribing it for the person with the penis to put on their penis. So there will be some patient education required because of the way the prescription looks.
“Also, we’ll be wanting to support our pharmacy colleagues with information around what it says on the prescription.
“What I’m planning to do with my change of practice is probably print out the information from the Melbourne Sexual Health Centre and give it to the patient, or send a note or ask them to say to the pharmacist to give me a call, because I do think there will have to be some communication around this change.”
The evidence currently supports a change of practice only for that specific group of patients – those with bacterial vaginosis, who are in heterosexual, monogamous relationships – but Dr Whitburn said that studies were coming in the LGBTQI+ population. “And it is probably worth discussing this study with people that don’t have monogamous relationships,” she said.