We may have just seen a week that provides some definition of where being a general practitioner is heading.
“Can you comfortably answer the following payroll tax questions? They are real questions sent recently to a practice by one of the state SROs.”
This was just one of many curly moments put to the audience of a TMR webinar this week on wealth creation – “wealth creation” being a cute but important stand-in term for “if you want your practice to be worth anything in a few years, you probably need to sort out your payroll tax problem now, as it’s the biggest current existential threat to your future wealth and wellbeing”.
Here’s a couple of excerpts from that SRO questionnaire to give you a taste of what you may find yourself up against:
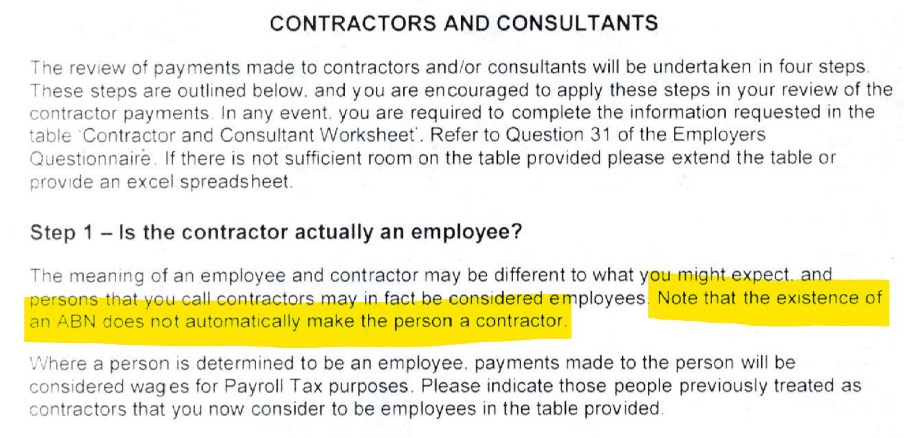
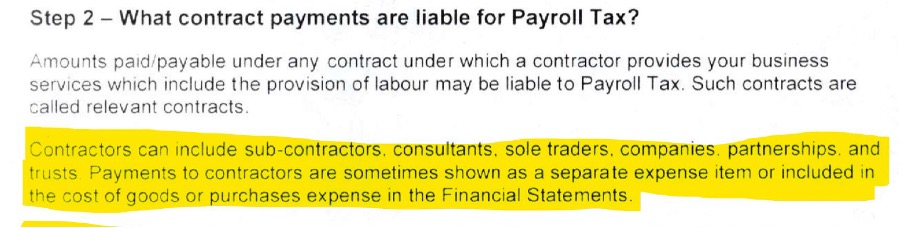
There are nearly 40 questions in the questionnaire.
Gulp.
You can watch the whole webinar here in your own time for free.
It’s a comprehensive up-to-date summary of all the issues for both owners (landlords) and contract (tenant) doctors, including insights from live cases and cases that never went to court because they settled, so most people were never able to learn from them.
Most importantly perhaps, it is a light at the end of the tunnel presentation: it provides pragmatic and workable ideas for remediation: this massive beast of an issue can be tamed, but it’s not always going to be easy or cheap to do it, depending on your set up.
The presentation features specialist medical practice advisory principal David Dahm and legal counsel familiar with lots of SRO cases Lukasz Wyszynski. It also features a great summary of all the ways you can do payment flows from the CIO of Tyro, Peter Williams.
It’s 100 slides long, but nearly all of the slides have something interesting or compelling in them.
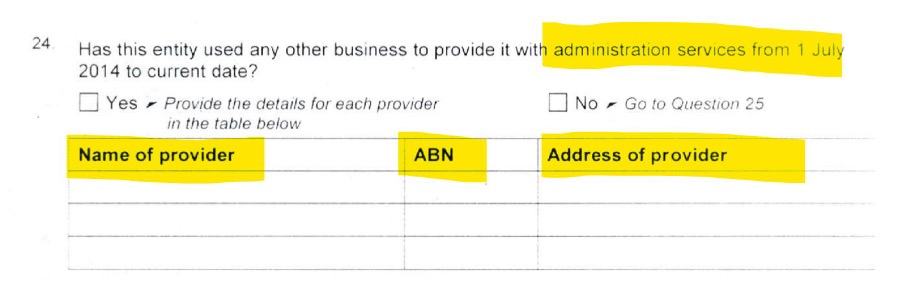
Here’s an interesting one:
TMR understands this recent assessment notice worked out to $60,000 per doctor per annum in the practice, going back at least eight years, plus interest and penalties, and all those Xs at the end adding to over $3m.
Dahm might have made a good cameo on Monsters Inc.
Remember Sully’s motto? “We scare because we care.”
There’s lots of scary stuff in his presentation, and, perhaps as a result, Dahm is constantly accused of hyping the issue of payroll tax up (for what reason his accusers never really get to, possibly because if they did they might expose themselves to a defamation action).
But Dahm is just trying to get your attention. He wants to help. And he’s a details guy.
In this webinar he presents a lot of practical advice in the form of checklists, and then remediation strategies.
Part of the presentation is an exhaustive list of all the things Dahm has seen SROs try on in cases.
There’s a lot of really interesting and at times weird things, like the example below where the SRO has gone to Google Street View to make the point that the practice does not advertise the doctors who work at the practice on their signage, as Westfield would do of all the major tenants in its shopping centres.
One of the strong messages you get from the presentation is that the SROs are working hard at looking at the smallest thing that might help make their case so you have to start looking to cover off a lot of smaller issues as well as the big ones, like payment flows.
As Dahm points out, the ATO has stated clearly that establishing an employer/employee relationship versus a tenant/landlord one is not just a few key things: it’s the “entirety” of a setup. And the SROs are looking at all points of the compass.
Dahm’s last slides are probably the most important and compelling as they deal with developing a good plan to tackle the issue. He is laying out reasons not to panic.
He notes that depending on a series of factors, remediation might be small or large, to the point where “detonation” might be sensible strategy.
“Detonation” is where you wind up all your structures and start again. It’s the nuclear option and not common, but Dahm says that in some situations, setups are not worth trying to remediate as it becomes too cumbersome and expensive. In order to set up continuity and value creation, something entirely new is required.
The most important message I took from the webinar was that all the “unknowns” that are freaking everyone out about payroll tax are slowly but surely starting to become “knowns”, and with that, professionals are now able to start giving everyone the correct advice they need to navigate what seemed like an existential threat to the entire profession.
In other words, there is light now at the end of this dark tunnel.
The bad news remains that the law is the law. Dahm tells the story of Dr Max Kamien from WA who set up a not for profit practice within the University of WA in the 70s. The story is in Australian Doctor. After getting pinged and getting advice from the university’s expensive law team and the best payroll tax lawyers in the state that they could fight it, Dr Kamien tells of an off-the-cuff discussion he had with a patient who happened to be a Supreme Court judge. He told Dr Kamien, way back then in respect to payroll tax, “It is everyone’s responsibility to know, or to find about, the laws pertaining to them.”
SROs and the ATO are coming for practices now in high numbers because technology is enabling things like data matching so they can. And they aren’t going to back off. The law is the law.
The good news is, with the right advice, some time and thought, the issue should be manageable for most practices over time.
Here’s that webinar link again. It includes a Q&A where all the live questions from the audience are answered by the panel.
Dr Irwin’s dangerous mind
Segue.
If you read Dr Chris Irwin’s opinion piece this week on voluntary patient enrolment (VPE), one thing he addresses is payroll tax.
The ASGP president says it’s a major problem already and one that’s not being addressed by the big member groups. If VPE does kick in – it is in the main supported by the AMA, RACGP and ACRRM – then the significant funding shifting directly to practices and not the individual doctors will potentially crash the whole services entity business model, reduce the profitability of most practices by over 5% as a result, and send many broke.
There’s a lot of things that have to come together for that to happen, and speaking to some accounting experts about the issue – it’s an issue already for PIP payments obviously – there will likely be terms within a service agreement that practices can agree with a tenant doctor that could manage the situation, depending of course on how the government structures VPE in the end.
Notwithstanding, Dr Irwin, unlike some (not all) of his fellow candidates for the upcoming RACGP presidential election, is firmly thinking ahead (there are seven candidates in all).
And thinking deeply.
His ideas on VPE are worth a read, not so much for some of the conclusions he is drawing about where it will end up, some elements of which – like payroll tax – possibly can be avoided with some clever thinking a long the way, but for his broader views on how general practice has historically engaged with Canberra.
He says GPs have in the past largely surrendered to the system and have been slaves to it, but GPs need to shift their thinking on positional power significantly if they are to navigate their way out of what is probably their lowest ebb in history as a profession.
He’s a bit of a revolutionary in that his ideas are surely seductive to the masses – in more of a Che Guevara than a Donald Trump way, mercifully – but to those currently in power in the major member bodies and Canberra, they must feel “dangerous”.
He wants to turn traditional power dynamics in general practice medicine upside down.
He wants to release what he sees as the enormous latent political power that GPs have if they organise properly.
“I completely disagree with the defeatist attitude that seems prevalent in many GP circles: ‘We may as well collude in a system we see as harmful, so at least we can minimise harm.’ General practice is a sleeping giant that just needs to be awakened. We are acting solely in our patients’ best interests – imagine the force for good that we could be if we stopped fighting with both hands tied behind our backs. We are larger and stronger than the Pharmacy Guild. The government needs us far more than we need government. It is completely attainable for general practice to be the premier medical speciality.”
Dr Irwin makes some killer points. Like, if the federal government can commit to $5.4 billion in new ongoing annual childcare funding (he agrees with the policy), which is 60% of the entire Medicare funding base for general practice each year, why can’t it pay its GPs properly as well?
“It shows … that there is money to be spent – just not the political will to spend it on fixing general practice,” he says.
Although he’s written this piece for TMR ostensibly to unveil the flaws of VPE, what he’s really done is written a mini-manifesto for a potential new future for general practice.
One where it organises properly and exerts its enormous latent political power to systemically influence at the community level with the single intent of improving the lot of patients (and yes, of course, through improving the lot of GPs).
I wonder what is going to happen here?
If Dr Irwin were running for president in a small South American country in the 1970s he’d surely disappear mysteriously one weekend – taken out by the CIA on behalf of the incumbent government of the country.
While that can’t quite happen in Australia, you wonder what those currently in power are thinking they can do, if Dr Irwin gets any traction for his ideas.
They’re dangerous ideas, depending on where you sit in the power spectrum of medical politics. They have a whiff of the sort of insurgency that characterised the latter days of Dr Harry Nespolon as president of the RACGP. It feels as though Dr Irwin is picking up where Dr Nespolon left off.
Notably, they are all ideas that feel like they are right for the times.
General practice is undergoing major structural changes which threaten its existence in all sorts of ways.
It is under threat from:
- technology start ups such as Mosh, Pilot and Medinet, all of whom are hoovering up low-hanging non-Medicare-rebated consult fruit via modern technology and marketing plays
- the hospital sector, which is reaching out rapidly with virtual technology and state funding to manage their patient cohorts in the community, separately from the GP network
- private health insurance, which is rapidly soaking up all the opportunity above bulk billing to meet community healthcare needs where they can
- PHNs, which in many regions (not all) are disintermediating their local GP network for key funding for services like mental health, and which are trying to suck away GP-owned data to form a separate population health centred power base (outside of general practice)
- state government revenue offices which are hunting for revenue gold in lazy and antiquated medical practice structures, and in doing so are not only threatening the viability of practices, but of the contractor doctors who work in them
- federal government, which while making a lot of noise about fixing general practice and committing some short-term money, is broke and searching desperately for ways to save in the mid term.
Maybe an idealist and a revolutionary is just what’s needed for GPs in these times, dangerous or otherwise.
Could it hurt?
The profession gets Hickied
Segue.
Speaking of “the times”, and trying to herd GP cats, it’s interesting to see that when general practice really needs to align on an important issue of patient safety and down the weapons of political infighting, it can do it pretty quickly.
This week the profession collectively rallied to put paid to initial claims by Professor Hickie that GPs weren’t treating mental health properly in the community. Professor Hickie had initially made those claims in an MJA Insight article and had based his conclusion on an analysis of Medicare claim items.
Very quickly various parties pointed out that Professor Hickie’s entire premise was flawed because GPs often don’t book specific mental health items but general items when treating mental health issues, because of inefficient pricing signals in the items. These parties also pointed out that mental health help often makes up parts of broader consults and is thus never recorded.
Professor Hickie didn’t buy it and came out punching every which way, particularly on Twitter.
And he got hammered from all points of the GP political compass, from the current RACGP president, to candidate future presidents, to well, lots of streetwise GPs. It was a rare case of unity across the profession on a very important issue of what the profession feels is gross misrepresentation of their role.
Interestingly Professor Hickie didn’t address the flaw in his article at all – that the data is wrong, at least as evidence of what he was trying to claim. He played the men and women (GPs as a profession) not the ball (actual numbers of mental health consults done by GPs).
In an extraordinary interview with TMR yesterday he essentially said that the time of GPs had past. That with the internet we can bypass the GP “gatekeeper” and go direct to specialists.
In respect to the internet and bypassing GPs one Twitter post pointed out that Professor Hickie has an interest in a commercial venture called Innowell. The explanation Innowell gives on its website for the product is as follows:
“Innowell provides research-validated digital tools and personalised insights to connect your people to the support they need when they need it.”
Presumably Innowell isn’t pointing too often to your local GP if Professor Hickie is is true to his word on generalists.
But whether he is right in his assertions about GPs and mental health or not (he’s almost certainly not, although the internet is changing how GPs practice – derr, what profession isn’t it changing, Ian?) is not really the point here.
The point is, that when they need to, and as Dr Irwin suggests they can do with far greater effect into the future, GPs can organise effectively, and quickly.
A lot of factors are converging now for GPs which indicate it might be time to fundamentally shift the traditional government-dictated paradigm for GP working conditions and pay.
For the first time I can remember the community, normally apathetic about the plight of GPs (in part because although not paid anything like specialists, they are still well paid), seems to be starting to listen to the problems our GP network is facing, and expressing some support for change too.
Hardly a day goes by now where the current plight of GPs, especially rural and remote ones, isn’t the subject of some major media story.
It’s not normal.
For some reason perceptions in the community are shifting.
For how long I wonder?
Harnessing this current shift while it lasts is vital.
But as Dr Irwin points out, we aren’t likely to do that if the usual suspects stay at the helm of our major GP representative bodies.
Revolution, anyone?


