Australian research is investigating whether two natural supplements can help prevent diabetes in at-risk individuals
Australian research is investigating whether two natural supplements can add to the efficacy of traditional treatments to prevent diabetes in at-risk individuals
Currently one in six Australian adults aged over 25 suffer from pre-diabetes – an asymptomatic condition linked to metabolic syndrome, which puts individuals at high risk of developing Type 2 diabetes and cardiovascular disease.1 Pre-diabetes is diagnosed by a single plasma glucose measurement of one of the following:
• Fasting plasma glucose (5.6-6.9 mmol/L)
• Glycated hemoglobin (HbA1c) (5.7-6.4%)
• 2-hour oral glucose tolerance test (OGTT)
(7.8-11.1 mmol/L)
Metabolic syndrome is a cluster of conditions putting an individual at high risk of cardiovascular disease, and includes the following:
• Increased waist circumference (greater than 80cm for women, and 94cm for men)
• Raised triglycerides (150 mg/dL or higher )
• Raised blood pressure (140/90 mmHg or higher)
• Glucose intolerance, with OGTT 7.8-11.1mmol/L
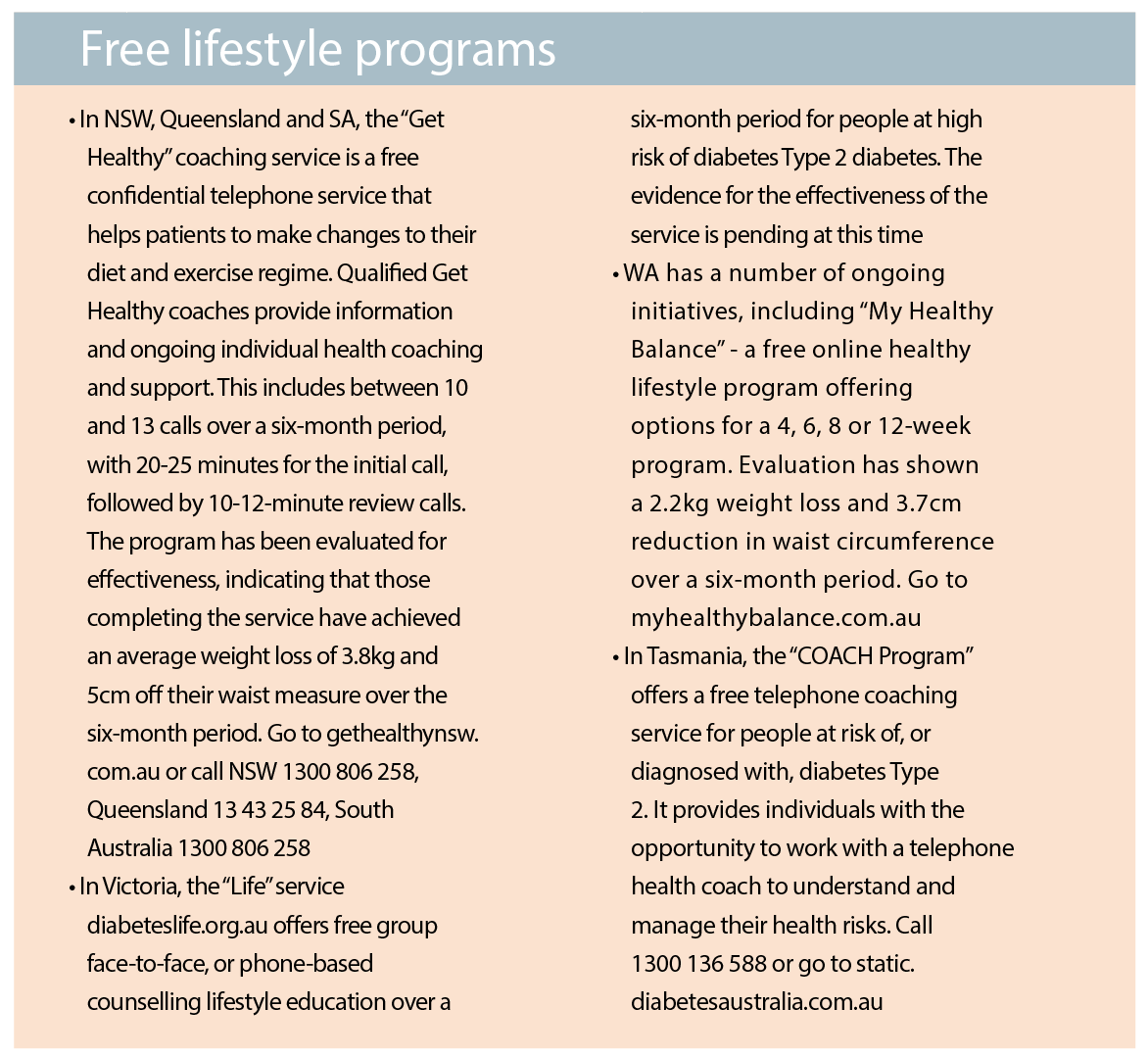
Primary care is critical to managing pre-diabetes to avoid a progression to Type 2 diabetes, using a personalised approach to monitoring and management of co-existing obesity. Risk of the progression to Type 2 diabetes can be established by using AUSDRISK, the Australian Type 2 diabetes risk assessment tool, which is accessible on the Diabetes Australia website. An AUSDRISK score of 6 -11 suggests an increased risk, and the score of 12 or more suggests undiagnosed diabetes Type 2.
The MBS item number 66841 for HbA1c testing describes the test as the “quantitation of HbA1c performed for the diagnosis of diabetes in asymptomatic patients at high risk”. This applies to patients with AUSDRISK score of 12 or above, and those with a medical condition or ethnic background associated with a high risk of diabetes Type 2.
Lifestyle interventions
Evidence has shown that lifestyle interventions are effective for the prevention of Type 2 diabetes, and are therefore recommended as first-line therapy.2 An estimated 60% cases of diabetes Type 2 can be prevented with a reduced-calorie diet and physical activity of moderate intensity for at least 150 minutes per week. Overweight or obese adults should be advised that even modest weight loss of 5% of body weight could prevent or delay progression to diabetes Type 2.
Very low energy diets
Very low energy diets are effective in supporting weight loss in adults with BMI > 30, or with a BMI > 27 and obesity-related comorbidities. They provide 800 total calories per day in the form of partial meal replacements and include the daily allowance of all essential nutritional requirements. Before starting VLED, baseline blood tests are performed, and reviewed regularly every four to six weeks. VLED are not recommended for longer than 12 weeks, but can be used for up to 12 months under medical supervision.
Pharmacological options
There are currently three TGA-approved pharmacological options for weight loss, which can be used long-term:
• Phentermine (Duromine) is a centrally-acting adrenergic agonist which suppresses appetite
• Orlistat (Xenical) inhibits pancreatic and gastric lipase, reducing fat absorption by 30%
• Liraglutide (Saxenda) is a glucagon-like peptide receptor agonist which slows gastric emptying and suppresses appetite
The Australian Obesity Management Algorithm notes the high cost for these weight loss medications at $125-$387 per month, and a lack of data for long-term effectiveness and safety. 3
Bariatric surgery
This is currently the most efficacious weight loss intervention for adults with BMI > 40, or with BMI > 35 and comorbidities. Bariatric surgery may be considered as part of a multidisciplinary approach, which includes GPs, surgeons, dietitians, nurses and psychologists.
Natural supplements
A world-first face-to-face diabetes prevention study is currently running at Sydney’s Royal Prince Alfred Hospital’s Charles Perkins Centre. It is modelled on similar initiatives in Finland, China and the United States, which achieved a 60% success rate in the prevention or delay in the development of Type 2 diabetes. The researchers aim to answer whether two commonly used over-the-counter natural supplements (Alpha-Cyclodextrin fibre and Compound K ginseng) can add efficacy to standard diet and exercise interventions, due to their synergistic effects on metabolism.
Alpha-Cyclodextrin (?-CD)
Dietary fibre is known to bind to dietary fat in a 1:1 to 1:1.4 ratio. These small ratios make commonly used types of dietary fibre impractical for weight loss, as very large amounts of fibre would have to be consumed to remove a significant amount of dietary fat.
The current search for a more efficient fat binder has focused on the fibre supplement FBCx®, a formula based on ?-CD, a polysaccharide derived from corn. It has been demonstrated that ? -CD has the ability to bind with dietary fat in a ratio of 1:9, therefore preventing the absorption of nine times its own weight in dietary fat.4 It appears that ?-CD forms a very stable complex or emulsion with the dietary fat in the stomach and remains bound to the fat during its passage along the gastrointestinal tract.
Previous research examining the effect of ?-CD on weight loss has shown effectiveness in reducing and maintaining body weight in obese patients with diabetes Type 2. For study subjects with raised triglyceride levels at baseline, there was a consequent reduction in cholesterol and triglyceride levels, with no adverse side effects.5
Compound K
The root of ginseng has been used in traditional Chinese medicine for centuries, most recently for improving glycaemic control.6 The pharmacological properties of ginseng are attributed to the ginsenosides, the active components found in the extracts of various species of ginseng. Numerous studies of ginsenosides conducted in animals have focused on their anti-diabetic properties.7,8
GINST15™ (a ginseng extract formula based on Compound K, a final product of hydrolysis of protopanaxadiol ginsenosides by intestinal microbiota) has been shown to be the active ingredient responsible for this anti-diabetic action. It is thought to enhance insulin secretion by acting directly on the pancreas, with a consequent lowering of blood glucose. A combination of Compound K and metformin has demonstrated significant efficacy in the control of plasma glucose and insulin levels in diabetic mice, compared with metformin therapy alone.9 Similar efficacy and safety have also been demonstrated in humans.10
The research study
Four hundred participants are provided with individually tailored lifestyle advice, including a reduced calorie diet and prescription of 150 minutes of moderate physical activity per week. They are also provided with trial supplements containing ?-CD, Compound K or placebo.
The study aims to assess the effect of these remedies on cholesterol levels and glycaemic control.
The study is currently recruiting participants with BMI ? 25 and test results indicating pre-diabetes. If you have patients meeting this criteria, further information is available at www.metabolictrial.com or by calling (02) 8627 0101.
Dr Nicholas Fuller, PhD, is research program leader at the Charles Perkins Centre at the University of Sydney
References
1. https://www.mja.com.au/journal/2007/186/9/prediabetes-position-statement-australian-diabetes-society-and-australian
2. http://www.nejm.org/doi/full/10.1056/NEJMoa012512
3. The Australian Obesity Management Algorithm https://diabetessociety.com.au/documents/ObesityManagementAlgorithm18.10.2016FINAL.pdf
4. Artiss J., et al. The effects of a new soluble dietary fiber on weight gain and selected blood parameters in rats. Metabolism Clinical and Experimental, 55, 195-202 (2006).
5. Grunberger G., et al. The benefits of early intervention in obese diabetic patients with FBCx – a new dietary fibre. Diabetes/Metabolism Research and Reviews, 22, 56-62 (2007).
6. Vuksan V., et al. Nutr. Metab. Cardiovasc. Dis., Herbal remedies in the management of diabetes: lessons learned from the study of ginseng. Nutr. Metab. Cardiovasc. Dis. 15, 149-160 (2005)
7. Akao T., et al. Appearance of compound K, a major metabolite of ginsenoside Rb-1 by intestinal bacteria, in rat plasma after oral administration – Measurement of compound K by enzyme immunoassay. Biol. Pharm. Bull., 21, 245-249 (1998)
8. Tawab M. A., et al. Degradation of ginsenosides in humans after oral administration. Drug Metab. Dispos., 31, 1065-1071 (2003)
9. Yoon S. H., et al. Anti-diabetic effects of compound K versus metformin versus compound K-metformin combination therapy in diabetic db/db mice. Biol. Pharm. Bull. 30, 2196-2200 (2007)
10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4213818/ – This is the human study that is the main reference for the ginseng product