Inhaler use can make or break how well the disease is controlled, but too many patients are using them incorrectly.
Much has been researched and written about inhaler devices and their specific role in managing chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD).
Using an inhaler correctly requires a patient being able to complete a series of steps associated with the correct use of that inhaler.1 More specifically, the way in which patients use their inhalers is now accepted as being critical to good disease outcomes, with the latest clinical guidelines reiterating the importance of checking a patient’s inhaler technique and adherence before amending a patient’s medication regimen.
Despite this, inhaler use, in particular inhaler technique, remains a significant and persistent problem.
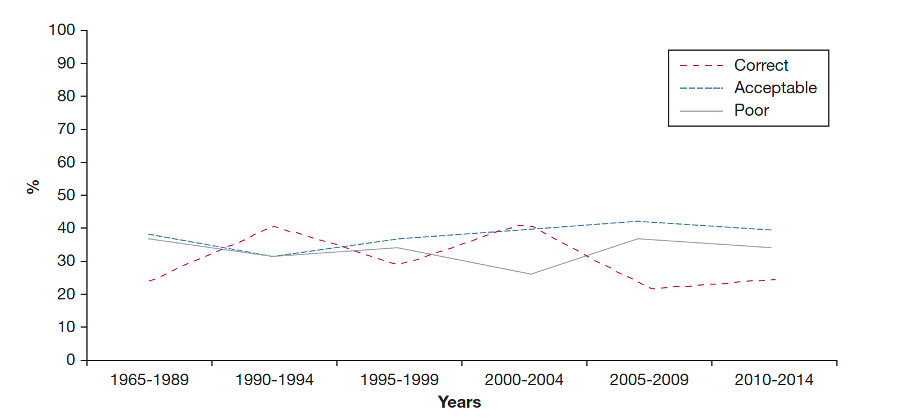
In 2016, a review of the scientific literature2 found that since the introduction of the first inhaler in the 1950s, the use of inhalers has been problematic and this has essentially continued ever since (Figure 1). One of the most recent Australian studies evaluating inhaler technique found that, among a cohort of 200 people with asthma visiting their GP, not a single individual was able to demonstrate correct inhaler technique, making at least one error. This was despite 86% of patients reporting that their inhaler was easy to use and 73% stating that they believed they had a “good” or “excellent” inhaler technique.3 Clearly achieving and maintaining correct inhaler technique continues to require our attention.
The significance of poor inhaler technique cannot be underestimated. It is established that incorrect use of inhalers leads to poor disease outcomes.4,5 The “gold standard” for inhaler training,6-9 now used globally, is well defined. Patients need to be shown how to use their inhaler with a placebo device, they need to be “tested” on their use and then re-educated as appropriate.5,10 They can then be supported with online videos of inhaler technique that they can access at any time.11
Much research has focused on identifying and improving inhaler technique once a patient has been prescribed and has received their inhaler. But little research has focused on the importance of selecting an inhaler device that best matches an individual patient at the time of prescribing.
Today, there are multiple inhalers on the market, falling into three broad categories. These are the pressurised metered dose inhaler (pMDIs), the dry powder inhalers (DPIs) and the soft mist inhalers (SMIs). And if we consider the choice of drug, strength and inhaler type, prescribers now have more than 200 inhaler device-drug options to choose from.12
It is not surprising that the choice of inhaler can become confusing and, while there is much literature on patient preference and patient choice, the reality is that the former is not necessarily linked to better inhaler technique and the latter cannot be relied upon, as most patients report using their inhaler correctly, despite failing to do so.13
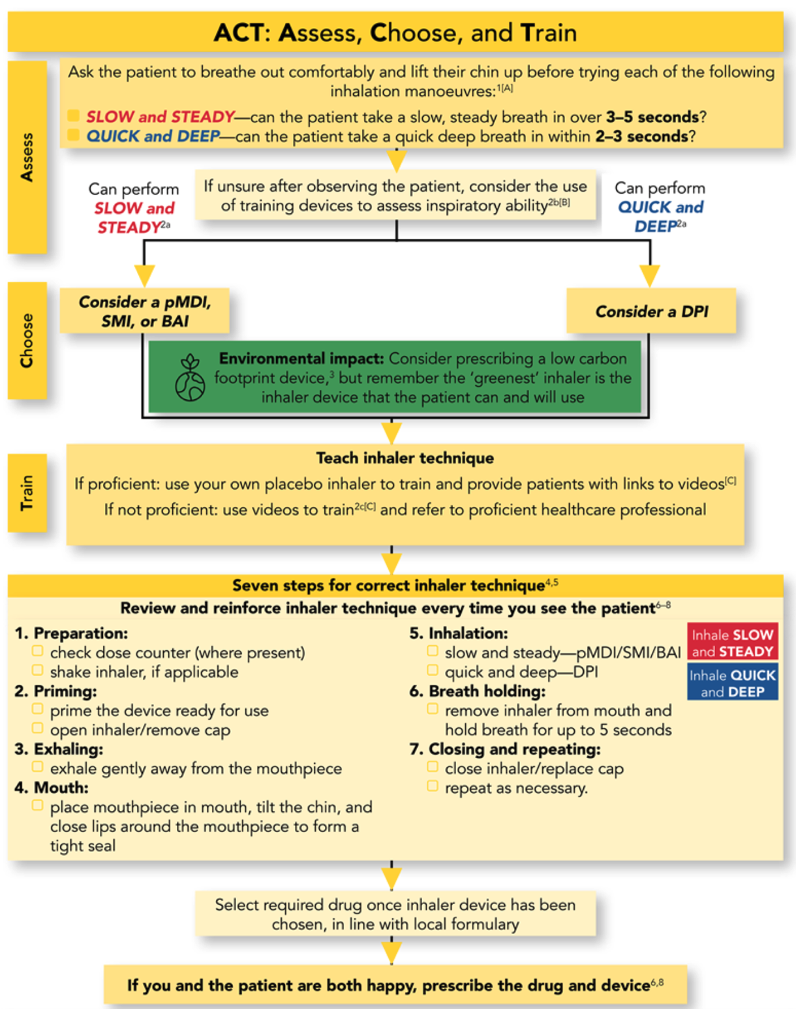
Clearly a more systematic and objective approach to selecting the right inhaler is warranted. Colleagues in the UK have considered this and proposed an “algorithm” for choosing an appropriate inhaler device (Figure 2).14
The importance of the breathing manoeuvre
When looking at the UK-developed algorithm for selecting an inhaler, it is not surprising that it starts with an assessment of the patient’s ability to “inhale”: can the patient breathe in “slow and steady” or “quick and deep” (Figure 2)? This is both logical and empirically based.
Patients with chronic obstructive conditions of the airways might be expected to have their inhalation manoeuvre compromised as their disease status changes. Research has shown that failure to breathe in correctly is one of the most common errors a patient makes when using their inhaler.5,15 Inspiratory errors have been independently associated with poorer disease outcomes (poor symptom control and hospitalisation), both in asthma and COPD.5,16 This is particularly important for DPIs, as the ability of the patient to inspire correctly through the inhaler – that is, have sufficient peak inspiratory flow (PIF) – is critical to drug delivery.
PIF in practice
Peak inspiratory flow is a unique physiological parameter that becomes relevant only when a patient is using an inhaler, in particular a DPI. DPIs are breath-actuated devices that require less patient coordination, making them easier to handle, especially for older people.5 However, for DPIs to be effective the patient must be able to generate sufficient PIF to disaggregate the powder within the inhaler into particles with a diameter of less than 5 µm that can adequately be inhaled into the lower respiratory tract6.
Each DPI has a different internal resistance and formulation, and thus a different optimal PIF.7 In general, a higher PIF is associated with better performance of the DPIs as it increases the dose inhaled by the patient.6
When PIF is measured against the internal resistance of a particular DPI, the minimum PIF required is generally considered greater than 30 L/min, while a PIF of more than 60 L/min is considered optimal,8 although there is still debate as to whether a PIF between 30-60 L/min is truly sufficient.9
Measuring PIF can therefore be done only against resistance, meaning that that standard spirometry does not provide us with any assistance here. Commonly, the simplest way to measure PIF is through the use of an In-Check Dial inspiratory flow meter, which is a hand-held device in which internal resistance can be adjusted to match the inhaler to be used and hence PIF for a particular device can be tested.
Currently, this device is not commonly used in practice, which is why the recommendation is to make a clinical assessment as to whether a patient can breathe in “slow and steady” or “quick and deep” (Figure 2).
Where to from here?
There is much to still learn about peak inspiratory flow in practice, such as the prevalence of suboptimal PIF, its impact on day-to-day medication-taking behaviour and how we can best measure and utilise PIF measurements to better match a patient to their inhaler.
However, we are making progress.
Several global ground-breaking studies under way at the Woolcock Institute of Medical Research are exploring the role of PIF in the medication management of asthma and COPD in primary, secondary and tertiary care.
In the meantime, at the time of prescribing and dispensing an inhaler, it important do the following:
- Determine whether a patient can breathe in “slow and steady” or “quick and deep” and prescribe the most appropriate device
- Deliver inhaler-device education when prescribing the inhaler, following that up with a face-to-face/tele-video assessment of the patient’s inhaler technique
- Continue to reassess and re-educate patients on inhaler technique over time.
It continues to be of critical importance to support our patients in the use of their inhaler. Unless we emphasise the importance of inhaler technique, our patients may not prioritise the correct technique and this is likely to make a difference to clinical outcomes.
If you are interested in contributing to our understanding of peak inspiratory flow and its role in medication management, contact Prof Sinthia Bosnic-Anticevich via woolcock.respimedicines@sydney.edu.au.
Sinthia Bosnic-Anticevich is a respiratory pharmacist and researcher. She is a professor at the Woolcock Institute of Medical Research, Faculty of Medicine and Health, University of Sydney.
References
1. NPSMedicineWise. Inhaler technique Device Specific checklists. https://d8z57tiamduo7.cloudfront.net/resources/Inhaler-technique-checklist_NPS-Medicinewise_2020.pdf. Published 2020. Accessed 24 March 2020, 2020.
2. Sanchis J, Gich I, Pedersen S, (ADMIT). obotADMIT. Systematic Review of Errors in Inhaler use: Has Patient Technique Improved Over Time? Chest. 2016;150(2):394-406.
3. Bosnic-Anticevich S, Kritikos V, Carter V, et al. Lack of asthma and rhinitis control in general practitioner-managed patients prescribed fixed-dose combination therapy in Australia. J Asthma. 2018;55(6):684-694.
4. Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. Journal of Allergy and Clinical Immunology. 2007;119(6):1537-1538.
5. Price DB, Roman-Rodriguez M, McQueen RB, et al. Inhaler Errors in the CRITIKAL Study: Type, Frequency, and Association with Asthma Outcomes. J Allergy Clin Immunol Pract. 2017;5(4):1071-1081 e1079.
6. Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119(6):1537-1538.
7. Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Counseling about turbuhaler technique: Needs assessment and effective strategies for community pharmacists. Respiratory Care. 2005;50(5):617-623.
8. Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: The effect of two educational interventions delivered in community pharmacy over time. Journal of Asthma. 2010;47(3):251-256.
9. Toumas-Shehata M, Price D, Basheti IA, Bosnic-Anticevich S. Exploring the role of quantitative feedback in inhaler technique education: a cluster-randomised, two-arm, parallel-group, repeated-measures study. NPJ Prim Care Respir Med. 2014;24:14071.
10. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2007. Available from: http://www.goldcopd.org/Guidelines/guidelines-global-strategy-for-diagnosis-management-2007.html Accessed December 10, 2014. In.
11. National AC. How to-videos. Published 2017. Accessed 23 October 2017.
12. Laube BL, Janssens HM, de Jongh FH, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37(6):1308-1331.
13. Jahedi L, Downie SR, Saini B, Chan HK, Bosnic-Anticevich S. Inhaler technique in asthma: How does it relate to patients’ preferences and attitudes toward their inhalers? Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2017;30(1):42-52.
14. Usmani OS. Choosing the right inhaler for your asthma or COPD patient. Ther Clin Risk Manag. 2019;15:461-472.
15. Sulaiman I, Cushen B, Greene G, et al. Objective Assessment of Adherence to Inhalers by Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2017;195(10):1333-1343.
16. Loh CH, Peters SP, Lovings TM, Ohar JA. Suboptimal Inspiratory Flow Rates Are Associated with Chronic Obstructive Pulmonary Disease and All-Cause Readmissions. Annals of the American Thoracic Society. 2017;14(8):1305-1311.


