We need to understand the systemic and societal drivers that are contributing to a consistent, reproducible gender gap in how doctors-in-training are paid.
A gender pay gap for employed hospital doctors in training makes no sense at all. They are covered by industrial awards, don’t negotiate pay rises or remuneration packages independently, and should, to all intents and purposes, be on a level playing field.
Salaries are usually determined by years since graduation (at least in the early years), and then achievement of milestones such as exam success.
So, it is fascinating to see some of the data from early-career doctors already showing a difference between male, female and non-binary doctors.
The Medical Training Survey is collected each year by AHPRA during the registration process.
This year, the Medical Board has published its first gender report. At last, openly published data makes clear the differences in trainee experience. This data was available previously but only by meticulously constructing a report from several different manual data downloads.
The new gender report is remarkable for what it shows.
For example, female trainees across Australia are less likely to be paid for their unrostered overtime than their male counterparts.
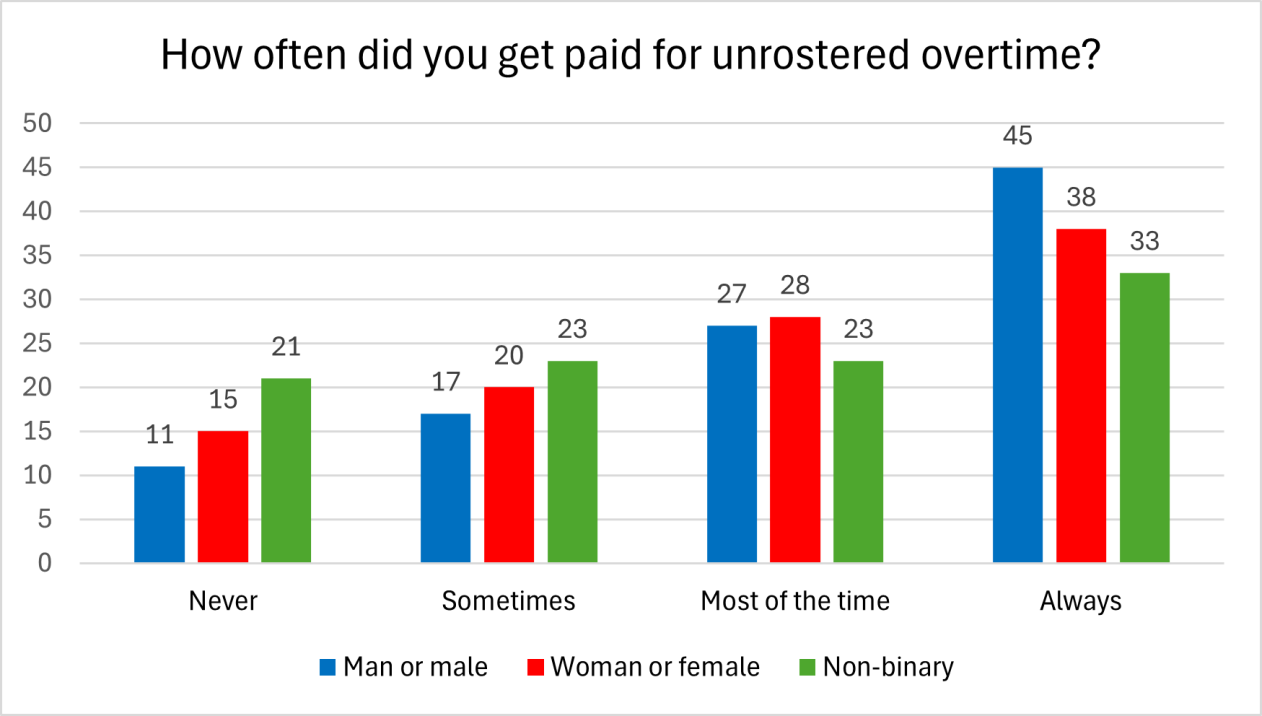
Fifteen percent of women and 21% of non-binary trainees, compared with 11% of men, reported that they were “never” paid for their unrostered overtime. Thirty-eight percent of women and 33% of non-binary trainees, compared with 45% of men reported “always” being paid. This distribution is statistically significant to the p<0.001 level – no mere coincidence. (Numbers: women n=8005, men n=6800, non-binary n=61)
Related
This is true across the entire country. Every state and territory has a gender gap in the proportion of doctors who responded. Again, no mere coincidence.
Early discussions I have had with medical leaders about this aspect of a gender pay gap have shown (again) a willingness to ascribe it as the trainees’ fault – “the women don’t claim it” – with a surprising lack of curiosity about why that might be the case.
What systemic issue could be operating in every single jurisdiction that results in women and non-binary trainees being 15% and 26% respectively less likely than their male counterparts to “always” be paid for unrostered overtime?
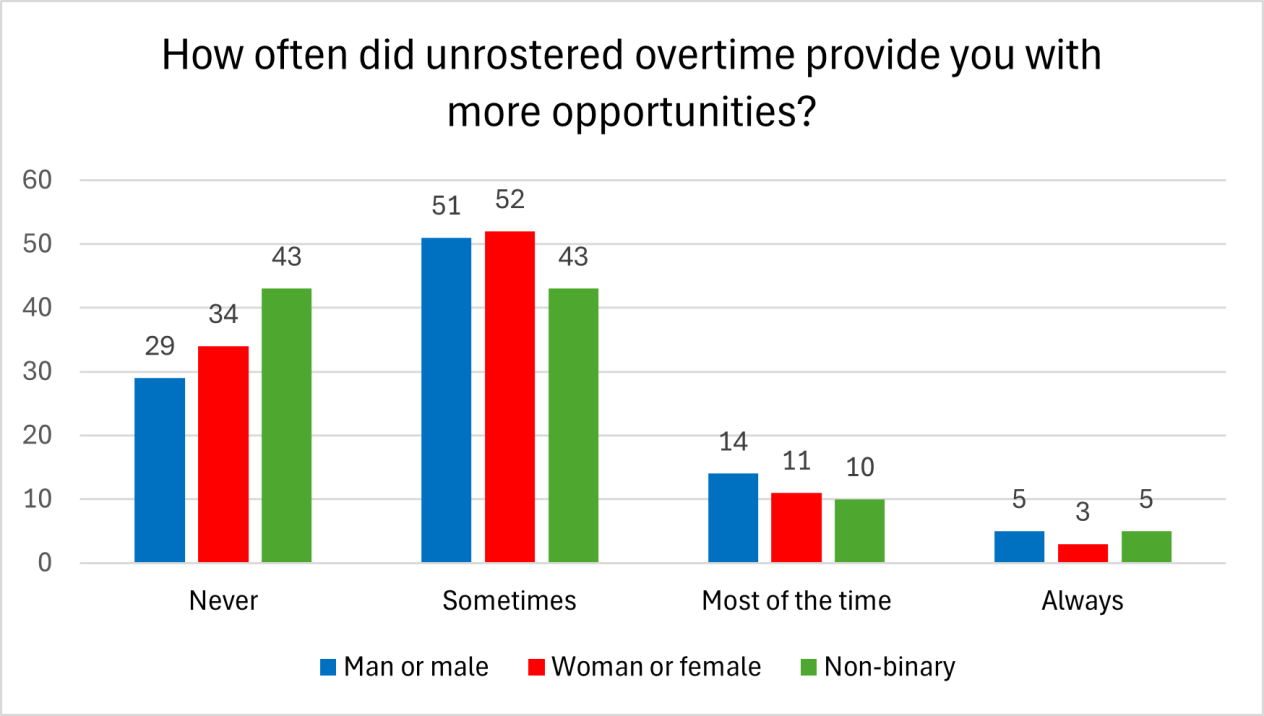
What is also interesting is that female and non-binary trainees are more likely to report that unrostered overtime never contributed to better opportunities.
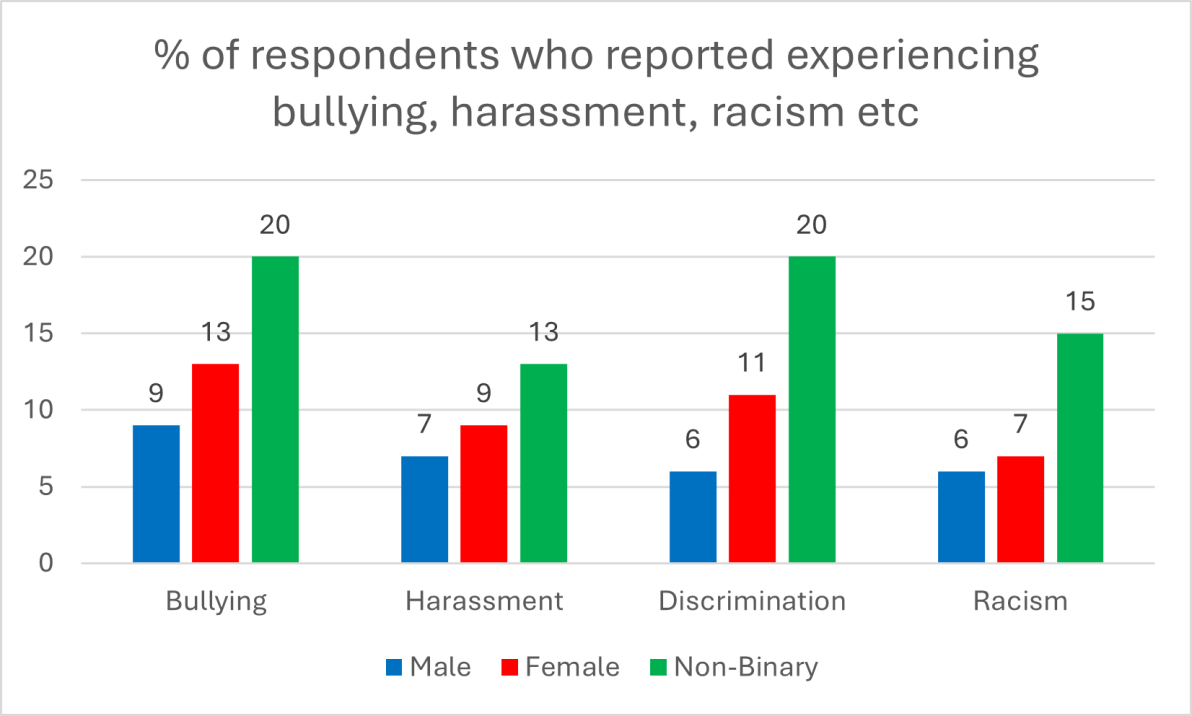
The bottom line is that female and non-binary trainees already report higher levels of experiencing bullying, racism, harassment and discrimination.
They are already made to feel “lesser” than their male counterparts by a workplace that still, even after 50 years, has not yet fully accepted that women and non-binary people belong in the medical workforce.
These trainees can already feel vulnerable, so the chutzpah to put in a claim to be paid when you weren’t rostered might just be ascribed to this. It is also possible (and I acknowledge that this is speculation) that female and non-binary trainees are lumped with “scud work” that contributes to their overtime, but to them, does not feel meaningful enough to warrant a claim for pay.
This hypothesis is supported by the gap in perception of contribution of overtime to meaningful learning.
Whatever the driver, it is no longer acceptable to simply tell people to claim.
We need to understand the systemic and societal drivers that are contributing to a consistent, reproducible gender gap in how doctors-in-training are paid. For this to happen, every employer and every college must become curious about gender differences in the reported experience of their medical workforce.
Dr Jillann Farmer is a GP and medical administrator. She is former medical director of the United Nations, currently working as a rural emergency department locum, and as CEO of A Better Culture.