We were going to slam the Strengthening Medicare Taskforce, but it could actually achieve something if it spies the elephant in the room.
Not long after Mark Butler’s speech at the AMA conference this week, the first draft of First Draft this week had a heading that read “Strengthening Medicare Taskforce is officially stillborn”.
It was an early draft: a gut reaction to a range of elements that already burden this taskforce.
They include:
- Its genesis as a last-minute election promise
- Its makeup, mostly, of the usual suspects: if you keep putting the same people back in same the room (most were there for the Primary Healthcare 10 Year Plan) how do you expect a new and improved outcome?
- Its singular focus on general practice: our healthcare system is an ecosystem (not withstanding our broken federated funding model), so when you push down on one part, something always pops out somewhere else and ends up blowing up the rest … if you want to fix primary care, you need to do it in sync with the rest of the system. You need to look at it as a whole. Hospitals should not be disconnected from GPs as they are. We all know that.
- The serious lack of detail on its terms of reference (is it just these selected elites at that table deciding it all, or will they take submissions and other external feedback, and will there be feedback mechanisms and reporting along the way?)
- The reluctance of anyone to clarify what the broad objectives outlined by Health Minister Mark Butler this week really mean; in particular, what he means by “fixing technology” (no one knows)
- The overt politicking: saying the ADHA, the My Health Record and aged care PIP are unfunded (which Butler did this week) was disingenuous … they are funded until the time the last Liberal government said they would be funded. Treasury isn’t sitting there saying, “Oh, we’ve no money left for the ADHA or the My Health Record next year, oops…”. That these costs have to be met next year and aren’t in long-term budget estimates is well understood public information known by Butler and his crew well before the election. And if they are genuinely surprised, then we have a bunch of rank amateurs in charge
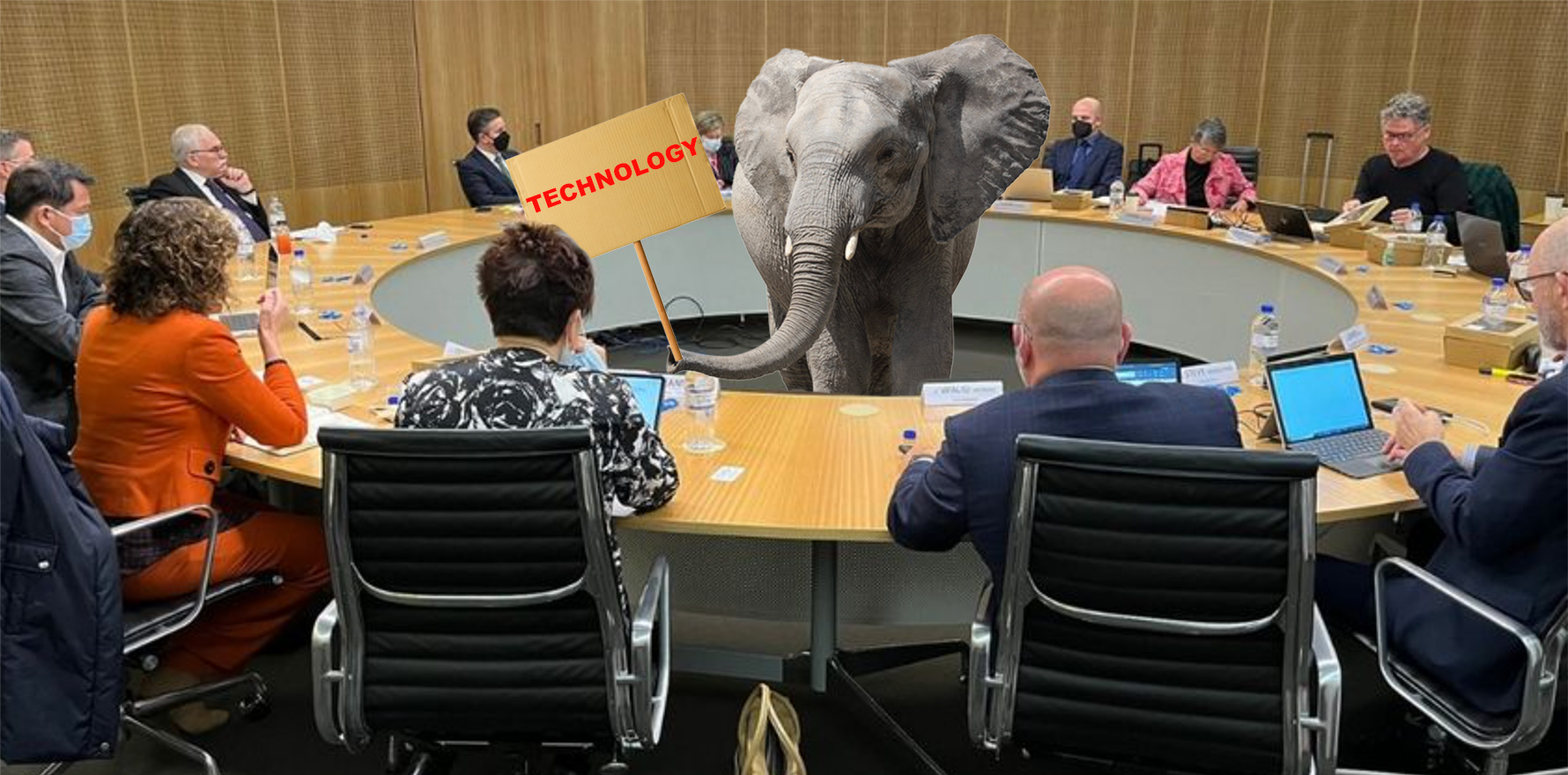
- And, finally, its lame PR unveiling this week, complete with a “health knights of the round table” photo opportunity, with all those usual suspects staring at each other hopelessly across an abyss of what looks like the same old rent-seeking and/or vested interest agendas (not everyone there has these issues for sure, but enough of them do for us to be very worried that we’re going to see yet another fight to a bitter draw where nothing changes really)
Protectionist positions need to be dumped for the greater good
As if all this weren’t enough to feed a sense of gathering pessimism, Dr Bruce Willett, standing in for RACGP president, Dr Karen Price, emerged from the first gathering to declare what is presumably the college position that, not withstanding everything else to be decided by this taskforce, fee for service would need to remain the mainstay of GP funding.
Having the RACGP come out at a major health reform round table and say fee for service is off the table before we even get started should give everyone an inkling of what we’re up against here.
Does anyone (college included) really think that in 20 years’ time, Australian patients would be best served by the system clinging desperately onto a funding paradigm that flies in the face of firm and emerging evidence around outcomes-based funding underpinned by better technology and data?
Sure, no one expects or wants fee for service to disappear overnight. But if we aren’t down to about 20-30% of the mix within 10-20 years, we are going to be in a lot of trouble – money trouble, system trouble, and patient outcomes trouble. That’s what it’s about, surely – money and patient outcomes (in a nod to Treasury, we are giving money equal billing to patient outcomes although it doesn’t sit that comfortably with us).
If we persist with idiotic starting demands like this we will almost certainly go from being 20 years behind some of the more tech-forward and reform-driven countries to being 30-40 years behind.
If that happens chronic care management will overwhelm us in the foreseeable future. It’s becoming a climate change-type issue.
It’s not in any way feasible to stick with a plan that says we are staying firmly with fee for service forever.
It’s like the coal lobby trying to stick with their climate-isn’t-really-changing line.
The college has to stop being schizophrenic: pushing outcomes-based care and GPs at the centre of it on the one hand and demanding that the funding model never move to accommodate such a system.
Shifting your funding base is of course a very scary proposition for GPs because their backs are already firmly against the wall.
Why would you willingly embrace even more uncertainty?
Because literally, we are out of time and we have to. Climate change again. We are already way behind where we need to be in order to rescue the economics and patient outcomes that we all expect of Australia in the near future.
And, it’s about the patients and the doctors, right?
Maybe Labor has got an inkling of what to do
So why did I change the heading and decide to become all optimistic-like here?
Unfortunately perhaps for Dr Willett (and maybe the RACGP) I’m next to certain the government (Department of Health included I think) entirely gets the chronic care and funding paradigm picture.
It is desperately seeking a means to start moving the system to measurable, data-driven, outcome-centric models of care and funding. They know if they could get there it would be transformative for both care and cost management (so too of course do a lot of doctors).
But it is struggling big time to draw itself a workable roadmap. One that caters sufficiently to all the interested parties while moving the dial on outcome-based care. It’s not surprising. Governments are struggling everywhere to get it right.
One of the reasons our government has been struggling for a while now is that a lot of the people at our health knights roundtable above have a history of fighting bitterly to a draw every time they sit down to agree on reform.
Nothing happens because too many interests need to be satisfied.
Ironically, many of the people at the table haven’t been picked because they can contribute ideas and IP to reform. The ideas are clear. They’ve been picked because they need to be bargained with and brought into a reform tent together, not because they are leading transformation.
Any roadmap will need to be politically palatable for all the knights we see in the picture above, some of whom are unwittingly (some maybe knowingly) still taking positions that would anchor us to the past.
It’s probably important to note that each of these groups usually mean well. They are fighting for their members. But each is only representing one part of a multi-player eco-system. They aren’t seeing or representing the whole system. And in doing this they are blurring the overall patient outcome perspective.
It’s not so much the map and route, but the people who get on the bus
If we get any form of workable reform roadmap it’s going to need a navigator of sorts (a captain?) to keep us all in line and on the map.
While on the one hand such a map (and the idea of a captain – think leadership) feels like a highwire act in terms of managing the politics and vested interests gathered to sort out this problem, on the other it’s not exactly rocket science, is it?
Australian healthcare operates on 1990s, siloed, server centric technology platforms in a lot of areas (not so much hospitals but we will get to that).
Countries that are getting their act together in health operate on cloud friendly, modern, distributed web platforms that can securely share data which you can more easily harness and analyse. You can’t manage what you can’t measure, and we certainly can’t measure general practice today, nor a patient’s journey out of hospital into the community and back.
The UK is about to undertake a potentially transformative federated healthcare data project which would longitudinally align data from tertiary to primary and community care, allowing far greater fidelity on outcomes-based funding (we have zero fidelity by the way) and health system planning.
The US is going crazy with open API web sharing alignment and innovation, brought about by the 21st Century Cures Act, and while in some respects things are getting more complex and crazier in terms of data, now all their major software systems can at least talk to each other across the country with meaningful data, and talk to patients. It’s generationally better already.
We have none of this. It’s getting embarrassing.
In 1990 in Australia we did our banking in physical banks, with real people, bank tellers, often still using paper bank books, and our money flowed, oh sooo slowly.
Today we do all our banking on our phones at light speed.
Healthcare in Australia is still using the equivalent of bank tellers in banks and in many instances, bank books (90% of GP surgeries still have a fax machine).
In a manner, the technology (or the lack thereof) in our healthcare system is one giant elephant sitting dead centre of that round table pictured above.
Note: State e-health departments are probably going to try to argue with this assessment. They are rapidly upgrading to sophisticated EMR systems, some of which have cloud capability. But none of it is being done with a view to having a wholly connected system. And most of it isn’t being co-ordinated across the states, or in some cases, even within the states.
The good news for this Medicare taskforce is that it looks like the Health Minister (and clearly some of his advisors) have spied the technology elephant, and want to see if they can’t start eating it bit by bit.
Butler said that technology was one of his three priorities for the taskforce.
Frankly, I’ve forgotten the other three he mentioned, they are so less relevant at this point of time to meaningful reform (OK, I remember patient enrolment, but it’s a distraction by comparison).
It’s not rocket science, it’s a people and structure problem
Let’s try to simplify things as much as we can for the person who might end up captain and head navigator of a potentially meaningful reform journey.
Take Butler’s priorities for this taskforce (I’ve had to look the others up for this paragraph): voluntary patient enrolment, facilitating multidisciplinary care (see technology), technology and sustainable business models for general practice (see also technology).
Ask yourself, which one is going to give us the biggest bang for our buck if we want reform that will meet our impending chronic care crisis head on, and provide the system with the agility and continuity to significantly improve efficiency and standards of care.
It’s technology, hands down.
Change how healthcare providers generate, share and analyse data between themselves and their patients, and you change the game fundamentally. The change will almost certainly help you resolve the other three priorities you’ve given this taskforce. It affects everything.
Technology also has a sneaky way of getting around archaic funding structures, such as federal primary care, versus state tertiary care funding. The right technology will almost certainly lead to an ability to safely alter these old funding setups to modern ones that suit a system that needs to manage chronic care much better.
Above all, technology will eventually provide you the data to manage a common sense transition to outcomes-based funding.
When we get there, we are going to start taking massive costs out of a system that today is increasingly being weighed down by a heavy reliance on very expensive tertiary care infrastructure and focus.
You will also provide primary care the ability to talk to the rest of the system around it (allied, tertiary and aged care) so you can start killing lots of cost and connected care birds with technology stones – interoperability and alignment of data across tertiary, primary and allied care (see web data sharing technology and even AI solutions evolving to crack all this open).
At this point you might notice that it is that it’s hard to spot anyone sitting around the roundtable pictured that understands the first thing about eating such a big technology legacy elephant in such a considered and strategic manner.
Of course, some punters will point to the representation on the roundtable by the Australian Digital Health Agency (ADHA) and ask (quite rightly), shouldn’t they be doing that?
They should.
But they haven’t for some time now, having cast themselves upon the rocks of centring nearly all their strategy and money around some more 1990s-style technology – The My Health Record – for the past 15 years.
Less than two years ago, everyone who stranded (scuttled?) the ADHA ship on those rocks left within a few months.
We then put an entirely new crew on board a ship that was … already wrecked on rocks.
You have to feel for the new crew a little.
“See that ship wrecked on those rocks over there, with a once-in-100-year storm building around it? Well, can you repair it and get it back out to sea please?”
It was a dumb thing to ask of new management. Demotivating even.
But that was the Liberal party in its death throes of government.
While we aren’t going to blame those currently running the ADHA for our predicament, neither can we necessarily rely on them to help that much either, given their current standing orders which remain focussed on the My Health Record.
They’re still busy attempting the impossible, as instructed by the previous government.
Some of them also don’t have the requisite skill set to help. The new crew was chosen pretty fast and not with genuine reform in mind.
What to do now?
The logic to think of this taskforce is the most important in Australian history goes as follows:
- We have an energetic, enthusiastic, and hopefully integrity-riddled new government, who wants to help.
- By chance (an artifact of an election promise really) this government is putting most of the right people in a room early and asking them, “OK, where to from here everyone”. The power of this can’t be underestimated. There’s even a bit (not much) money to throw around.
- The way healthcare is being run overseas is dramatically moving using new technology. We have plenty of evidence and even examples of how, for what we could now do.
- Australia is woefully backward now in health technology terms (hospitals aren’t a tragedy, but primary and allied care are). Something has to give.
- There seems to be a basic understanding that technology begets data which will gradually provide an increasing ability to achieve fidelity on outcomes based funding and care, and, that it can cross artificially created bureaucratic boundaries, such as state versus federal management and funding of different parts of the system, in order to achieve longitudinal care for a patient across a whole system.
- Everyone – even the ones fighting to protect short term member interests – really wants what is on offer here. There really aren’t any bad guys (eg, private health insurance) in the room.
Really, you could hardly ask for a better set of circumstances to trigger meaningful reform.
There’s lots of issues still with this taskforce of course:
- It’s got no detailed terms of reference to speak of
- It needs more non-vested interest and smart members who can tell everyone the hard truths, without worrying about getting shot when they get back to the office
- It needs to have mechanisms for more external stakeholder input, reflection, feedback and reporting. The people at that table are important and smart, but they are not going to make it by themselves
- It needs a determined leader to hold it together and curate it to the future (is that Mr Butler? We hope so)
But mainly, it’s an incredible place to find ourselves in terms of opportunity to effect meaningful reform to our healthcare system.
Fingers very tightly crossed.
If you’re interested in the topic of health reform, early bird tickets are now on sale for Wild Health’s next summit, No greater time to align our digital health strategy with our health reform agenda, October 18 in Melbourne. You can use this code to get 20% off all ticket types until August 18 – TMRWH20.