The association has proposed a single-payer model of healthcare for vulnerable groups.
Could our troubled and “inelegant” state/federal health funding divide ever disappear, if only for part of the population?
That’s the ultimate but somewhat remote aspiration of an AMA discussion paper that outlines the failings of the status quo and proposes a single-payer model targeted at populations at high risk of preventable hospitalisation.
“The Australian healthcare system is regarded as one of the best in the world, however in recent years its ranking has slipped as it has struggled to adapt to meet the health needs of a changing population,” says the AMA in the paper.
“A significant change in the funding arrangements is needed to ensure the sustainability of our health system.”
Currently the federal government is responsible for preventative care through the primary system and states for acute hospital care.
“For patients who are at a high risk of preventable hospitalisations, this division in responsibility creates a disconnect and offers little incentive for governments to collectively prioritise preventive care and early intervention,” AMA President Professor Steve Robson said in a media release.
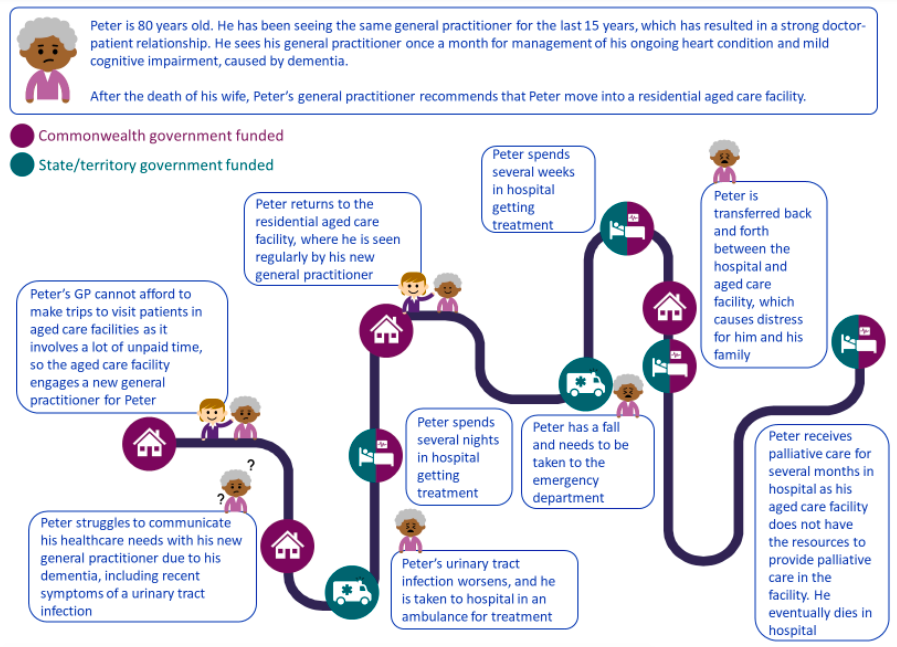
Any new model must incentivise prevention over reactive acute care, says the AMA.
“Governments must recognise that aspects of our current health funding arrangements aren’t working, with a hospital logjam crisis unfolding across the country and many Australians struggling to access care,” said Professor Robson.
“One of the best ways to ease pressure on our hospital system is to prevent the need for hospitalisations in the first place, and one way to do this is through preventive care and early intervention.”
The single-payer model proposed by the AMA would involve one entity funding all care for a particular population or populations.
“While a single-payer funding model does not guarantee more cost-effective and coordinated healthcare, it is undeniably an elegant approach to incentivise behaviour that could lead to achieving such outcomes,” says the paper.
The group said this type of funding could work for a number of populations but suggested it should be targeted at populations at high risk of preventable hospitalisation, particularly the elderly.
The AMA’s analysis found that Australians aged 65 and above accounted for half of potentially preventable hospitalisations, likely to result in $31 billion in costs over four years.
It suggested targeted single-payer models could also work for groups with chronic diseases, and for diverse groups – including lower socioeconomic groups, Aboriginal and Torres Strait Islander peoples, culturally and linguistically diverse groups, LGBTQIASB+, and rural and remote Australians – as they also have higher rates of hospitalisation.
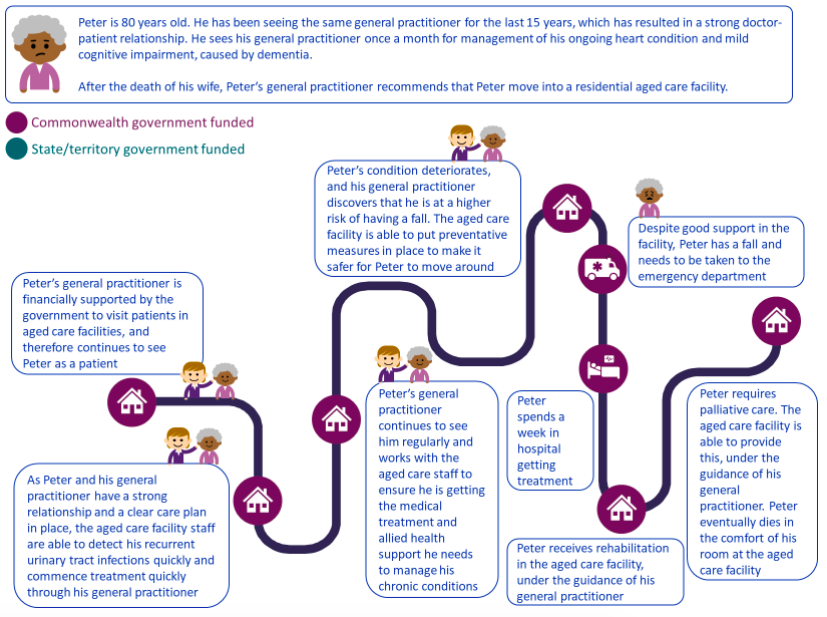
“Australia’s health system looks less and less like the system needed to care for a growing and ageing population with increased complex and chronic disease,” adds the paper.
But it wouldn’t be an easy ride.
“Transiting the current healthcare system to a single-payer model would require radical health system reform and it is unlikely the benefits from this transition would outweigh the costs and effort to redesign the system,” notes the paper.
The group suggested it may be achievable through a “healthcare card” – similar to the use of white and gold cards for veterans.
Another option would be a reimbursement model which involves the federal government paying states and territories for services provided.
They also suggested a pooled funding similar to the Aged Care Multi-Purpose Services Program.
The group flagged the possible caveats of the model.
Namely increased use of the services by the target group, risks of underfunding, being under or over selective in the target population and high implementation costs.
It also warned against a transition to capitation.
There are other options, says the paper, but the targeted single-payer model stood up to scrutiny in the AMA’s analyses.
“While a single-payer model for targeted populations is presented as an example of innovative funding reform worth exploring in Australia, it is important to note it is not the exclusive option,” said Professor Robson.
“The intent of our discussion paper is to initiate a dialogue on funding reform in Australia to deliver care that is efficient, coordinated and patient-centred.”





