The latest data from the ABS shows a full third of the country can’t get to see their preferred GP when needed.
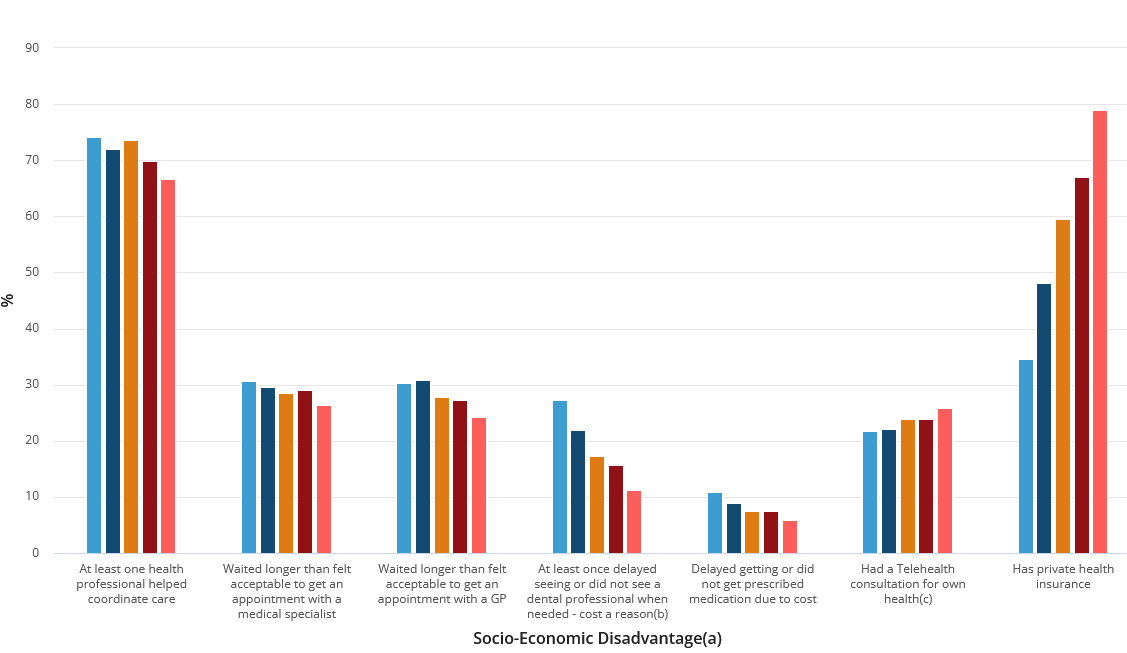
New data from the Australian Bureau of Statistics shows almost 11% of Australians who live in areas of the most socio-economic disadvantage are either delaying or going without prescription medication due to cost.
Additionally, 20.4% of people delayed or did not see a health professional for their own mental health when needed due to cost; and just 66.4% of people could always see their preferred GP when needed.
The ABS’s Patient experience survey results showed that GPs continued to be the most common health professionals seen in 2023-24, while the proportion of people who saw a medical specialist increased to 39.2% in 2023-24, from 37.9% in 2022-23.
Health service use in 2023-24 remained similar to 2022-23 for those who:
- saw a GP (82.6% in 2023-24 and 82.3% in 2022-23);
- saw a dental professional (53.2% in 2023-24 and 52.3% in 2022-23);
- visited a hospital emergency department (ED) (15.3% in 2023-24 and 15.2% in 2022-23);
- were admitted to hospital (12.7% in 2023-24 and 12.6% in 2022-23);
- saw a GP for urgent medical care (8.8% in 2023-24 and 8.6% in 2022-23);
- saw an after-hours GP (5.2% in 2023-24 and 5.5% in 2022-23).
The proportion of people who could always see their preferred GP when needed increased to 66.4% in 2023-24, from 63.7% in 2022-23.
“Areas of most socio-economic disadvantage saw 11% of people delaying or going without prescription medication when needed due to cost,” said Robert Long, the ABS head of health statistics.
“This was nearly double the rate of people from areas of least disadvantage (6%).
“More than a quarter, or 27%, of Australians living in areas of most socio-economic disadvantage also delayed or did not see a dental professional when needed due to cost,” Mr Long said.
“This was more than twice the rate of people from areas of least disadvantage, which was 11%.
“Only 35% of people living in areas of most socio-economic disadvantage had private health insurance cover, compared to 79% of those living in areas of least disadvantage.”
People living in areas of most socio-economic disadvantage were also more likely to report waiting longer than they felt acceptable for a GP or medical specialist appointment than those living in areas of least disadvantage.
They were also less likely to have a telehealth consultation.
“On a more positive note, people living in areas of most socio-economic disadvantage were more likely to receive coordination of their care than those living in areas of least disadvantage,” said Mr Long.
Source: ABS Patient experiences survey
In 2023-24, 28.6% of people reported waiting longer than they felt acceptable for a medical specialist appointment, similar to 27.9% in 2022-23.
The following people were more likely to report waiting longer than they felt acceptable for a medical specialist appointment:
- those aged 25-34 years than those aged 85 years and over (36.2% compared to 16.6%);
- females than males (30.8% compared to 25.7%);
- people living in areas of most socio-economic disadvantage than people living in areas of least disadvantage (30.6% compared to 26.3%);
- those with a long-term health condition than those without a long-term health condition (30.3% compared to 23.9%).
The proportion of people who had at least one telehealth consultation for their own health in the past 12 months decreased to 23.6% in 2023-24, from 27.7% in 2022-23.
In the last 12 months:
- 19.7% of people had a telehealth consultation with a GP;
- 4.6% of people had a telehealth consultation with a medical specialist.
The highest proportion of people who had at least one telehealth consultation were females aged 25-34 years (33.5%).
Related
The following people were more likely to have a telehealth consultation:
- those with a long-term health condition than those without a long-term health condition (32.7% compared to 13.8%);
- females than males (28.6% compared to 18.4%);
- people living in areas of least socio-economic disadvantage than people living in areas of most disadvantage (25.8% compared to 21.8%);
- those aged 65-74 years than those aged 15-24 years (25.2% compared to 17.0%).
In 2023-24, 17.0% of people saw at least one health professional for their own mental health, similar to 2022-23 (16.5%):
- 12.7% saw a GP for their own mental health (similar to 12.5% in 2022-23);
- 8.3% saw a psychologist (similar to 7.7% in 2022-23);
- 3.2% saw a psychiatrist (similar to 2.9% in 2022-23);
- 2.5% saw another mental health professional such as a mental health nurse, social worker, counsellor or occupational therapist (slightly higher than 2.2% in 2022-23).
Of people who needed to and saw a health professional for their own mental health in 2023-24, 26.2% did so at least once using a telehealth service (a decrease from 29.3% in 2022-23).
Read the ABS Patient experience survey in full here.





