Turns out the established clinical relationship rule for telehealth applies to GPs specifically, but not nurse practitioners.
Earlier this week, a post about a new telehealth clinic in Brisbane promising fully bulk-billed GP services caught The Medical Republic’s attention.
Everything was not as it seemed.
“We are bulk billing. Our goal here is to provide healthcare to all without fear or favour,” My Telehealth Clinic CEO Chris O’Donnell wrote on LinkedIn.
“Neither your postcode nor your wallet size matter to us.
“Everyone deserves great care and you shouldn’t have to wait weeks on end for an over-priced appointment.”
The exact services it offers, according to the post, are medical certificates, script renewals, rapid consults and medication delivery.
On first pass – sure, bulk-billed telehealth services sound like an idea that (a) patients would like and (b) might keep people out of the emergency department late on a Friday night.
There’s just one problem: GPs cannot bulk bill telehealth services for patients they’ve never treated in person before.
But there’s nothing to stop nurse practitioners from doing so. Nurse practitioners, along with other allied health practitioners and consultant physicians, do not have to see a patient face-to-face in order to treat them via MBS-subsidised telehealth.
The clinic’s COO, Tim Irving, confirmed with TMR that nurse practitioners “are leading the first point of contact” with patients.
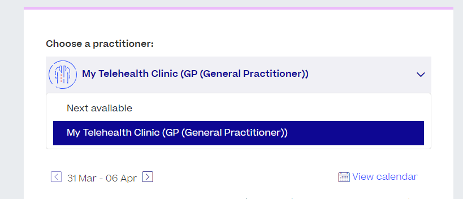
This is not immediately clear from looking at the website, which lists “general medical consultation” under its “types of appointment” tab, alongside covid consults and weight-loss consults.
On the appointments booking screen, the practitioner is listed as “My Telehealth Clinic (GP (General Practitioner))”.
TMR asked Mr Irving whether it could be considered misleading for patients booking an appointment, but he did not respond.
Mr Irving did say My Telehealth Clinic would not be focused on quick turnover cases and supported keeping patients’ regular GPs in the loop.
“Our business has GPs, nurse practitioners and dieticians in our cohort, which … gives us a lot of breadth in terms of our services and what we can offer,” he told TMR.
“We are really focused on giving good, patient-centred care.”
Under the telehealth established clinical relationship rule, it’s a legislative requirement for a GP or practice to have provided at least one face-to-face service to a patient in the previous 12 months in order for that patient to access MBS-subsidised telehealth.
There are only three exemptions to the existing relationship rule, all of which are temporary and due to expire in June.
These only cover blood-borne virus/sexual health, mental health pregnancy support counselling and covid PCR test referrals for antiviral-eligible people.
It’s not immediately clear why GPs and other primary care doctors are the only group specifically barred from MBS-subsidised telehealth with patients they haven’t seen in person.
Australian College of Nurse Practitioners CEO Leanne Boase told TMR it was potentially due to the high volume of MBS-subsidised consults that GPs do in comparison to other groups.
“There was a recent review of telehealth where it was suggested that everybody else have the same restrictions [as GPs],” she said.
“But I would argue that just because that’s in place for GPs doesn’t mean it would make it fair if it was in place for all other health professions.”
With a system as complex as Medicare, Ms Boase said it would make more sense to scrap the telehealth restrictions for GPs than to expand them to cover other healthcare professions.
“Medicare is not a way of controlling practice or business models, Medicare is a patient funding system,” she said.
Related
In her view, it ultimately came down to a question of trust.
“My way of thinking is that we’re all registered health professionals responsible to registering bodies under AHPRA and … we need to support professional people to make professional decisions,” said Ms Boase.
“If we don’t think people are making professional decisions, then that’s the angle we need to look at it from.”
RACGP vice president Associate Professor Michael Clements said that nurse practitioners being exempt from the existing relationship rule created a “double standard”.
“We need a consistent approach to the rules governing telehealth services to ensure the highest standards of patient safety are maintained and the best possible long-term health outcomes achieved for all patients,” he told TMR.
“So, if the 12-month face-to-face requirement applies to all GPs, it is difficult to understand why the same should not apply to nurse practitioners.”