Take a selfie and a new algorithm will figure out your blood oxygen saturation.
In good news for respiratory health aficionados, the smartphone could soon add pulse oximetry as yet another string to its bow.
Based on a canny proof-of-principle study, published yesterday in npj digital medicine, researchers from the universities of Washington and California San Diego say they’ve shown that a mobile’s regular camera can detect blood oxygen saturation levels as low as 70%.
That’s the lowest level pulse oximeters should be able to measure, according to the US Food and Drug Administration.
Of course, the tech’s a bit fancier than basic gear like the thumbprint password reader.
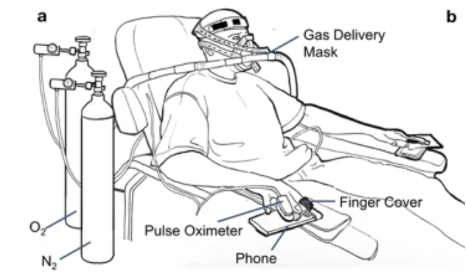
The study was conducted in a hospital environment for 14-19 minutes. Each of the six participants snorted controlled fractional mixtures of medical grade oxygen-nitrogen while resting comfortably. The experiment was designed to induce hypoxaemia in a stair-stepped manner, with the oxygen delivered at between 18% and 21% of the mixture and adjusted downwards in a stair-stepped manner every 1-2?minutes.
To gather the data, the participants had several pulse oximeter clips and a smartphone for each hand. And if that doesn’t already sound like a juggling act, they also had an ice pack put next to the smartphones to ensure they didn’t overheat while recording continuous video with the flash enabled.
The researchers then wheeled in the deep-learning algorithm they’d prepared earlier to estimate blood oxygen levels from the blood flow patterns detected in the resulting video.
They were able to collect more than 10,000 blood oxygen level readings of between 61% and 100% for each participant.
The initial findings look promising, with the phone’s regular camera able to detect low saturation levels in four cases out of five.
And there are other benefits too, in terms of not having to asphyxiate the user.
“Other smartphone apps that do this were developed by asking people to hold their breath,” co-lead author Jason Hoffman, a University of Washington doctoral student, told the Medical Xpress journal. “But people get very uncomfortable and have to breathe after a minute or so, and that’s before their blood-oxygen levels have gone down far enough to represent the full range of clinically relevant data.”
With further refinement, the data could also be sent direct to a doctor’s office, allowing for remote monitoring of the patient.
“Our results provide a positive indication that a smartphone could be used to assess risk of hypoxaemia without the addition of extra hardware in the future,” the researchers concluded in their paper, but recommended conducting further induced hypoxaemia studies to refine and test the algorithm.
And since everyone seems to have a smartphone on them 24/7, checking oxygen saturation levels several times a day while resting at home is a piece of cake.
Covid-ridden Millennials will really go for it: check your levels, jump up and down while sharing them on TikTok, text “OMG, I’m 70%” to your besties, then call 000 – all from the one device. What’s not to love?
Been told you’re a waste of oxygen? Ask penny@medicalrepublic.com.au for a second opinion.


