It is possible that manipulation of gut bacteria might end up becoming a mainstay of immune state treatments in 20 years' time, writes Dr Stephen Hall
In this discussion, I will restrict myself to issues of granulomatosis with polyangiitis, eosinophilia with granulomatosis and polyangiitis, polyarteritis nodosa, large-vessel vasculitis (giant cell arteritis) and Takayasu arteritis.
This is probably more than enough to consider where we stand at present, where we might be in five years and where we might be in 20 years.
With respect to the current management of vasculitis, the fundamental treatment modality for all forms of vasculitis remains corticosteroids.
This is a sad reflection of where we are, since corticosteroids have been around since 1949 and first used for systemic vasculitis in the early 1950s.
GRANULOMATOSIS WITH POLYANGIITIS
The main changes that have occurred in this disease are to some extent related to nomenclature with the withdrawal of the eponymous name of Wegener’s granulomatosis substantially as a result of historical research by Eric Matteson and his colleagues, and then by consensus of the vasculitis world.
The literature has explored a variety of steroid-sparing drugs in an effort to try to minimise toxicity from corticosteroids. It is very clear that the cumulative damage in systemic vasculitis is very similar to that of systemic lupus erythematosus, with part being due to the disease and perhaps an even larger part due to the ravages of our therapies.
Methotrexate, azathioprine, mycophenolate and leflunomide have all been employed as steroid-sparing drugs.
We have the least experience with leflunomide, but in direct head-to-head studies conducted by Wolfgang Gross, leflunomide in a higher than usual dose of 30mg daily does seem to be more effective than methotrexate.
Having said this, these things are typically studied over a relatively short period of time of one to two years. Given that we are dealing with conditions of extraordinary chronicity with a notorious tendency to relapse, the long-term results really need to be better assessed. In that regard, there is more data supporting the use of azathioprine compared with methotrexate. And there is a total dearth of long-term data looking at leflunomide or mycophenolate.
It was really the introduction of rituximab as an agent for treatment of ANCA-associated vasculitis which changed the complexion of our therapies. In clinical trials, rituximab was found to be as effective as cyclophosphamide and in relapsing disease, probably more effective, according to a post-hoc analysis.
However, it still remains important that everybody involved in the care of patients with systemic vasculitis appreciate that there was no reduction in the toxicity of drugs and in particular, no reduction in the infection risk when comparing cyclophosphamide to rituximab. That suggests that in the setting of systemic vasculitis, as we have already seen in rheumatoid arthritis and systemic lupus erythematosus, the risk of infections very much lies with how much corticosteroid is employed..
Corticosteroids suffer in the broader general medical community from a degree of “familiarity breeding contempt”, in that people who have used drugs for many years see them as being relatively innocuous, whereas the fact is that corticosteroids are the most potent immunosuppressive agents that we have.
One main goal of therapy has to be to reduce the dose of corticosteroids to as low as possible. There is convincing data from pooled analyses done by Peter Merkel that the continuation of prednisone/prednisolone in doses of 5mg a day is associated with a significant lessening in the risk of relapse. Consequently, there may not be any great argument for taking people off corticosteroids totally and keeping people on a small dose seems to be beneficial.
Clearly for some people, using rituximab is preferable to using cyclophosphamide. In particular, women with childbearing potential, men looking to father children in the future, people who have already received significant amounts of cyclophosphamide and those with relapsing disease all deserve being considered for rituximab.
We recognise that there are different forms of GPA and many of these can be managed with much simpler and less toxic remedies.
Low-dose corticosteroids and methotrexate will hold many people who have more limited forms of GPA, particularly those with sinus disease, modest lung disease and unusual conditions such as disease localised to breast.
IN FIVE YEARS
One can expect that in five years’ time, the world will have changed. In particular, the multitude of biosimilars available in the market will have reduced the costs of rituximab substantially.
One main advantage of cyclophosphamide remains its minimal cost. Rituximab may well be a drug which is used more frequently in the management of GPA and use may spread to the management of less severe forms of disease in association with lesser doses of corticosteroids once there is a reduction in cost.
The advent of killed herpes zoster vaccines will also mean that the risk of shingles which is a significant source of morbidity in the setting of intensive immunosuppression will become less. However, the vaccine has not proved to be a dramatically effective treatment. There is no denying that it has some effect, but in the setting of rheumatic diseases, the degree of protection confirmed by zoster vaccine is probably no more than 50% straight after vaccination and will wane over the next three to four years.
There is no registration available for repeat administration of Zostavax at this stage.
Less toxic steroids
It is possible that studies on newer forms of corticosteroid will also allow the development of corticosteroids of lesser toxicity, though whether this can be achieved within a five-year window is uncertain.
Nevertheless, there are a variety of interesting compounds being analysed, looking to see whether they can maintain corticosteroid effect while at the same time, lessening the degree of steroid toxicity.
IN 20 YEARS
The question here will be whether we can predict who will develop rare forms of vasculitis. We already have GWAS studies which have looked at the genetic propensity and there do seem to be some genetics which are significantly associated with the development of GPA.
There is some evolving data suggesting that the gut microbiome might also be of relevance.
There have been reports even as recently as last year’s American College of Rheumatology conference that there are differences in gut microbiota in patients with ANCA-associated vasculitis who have active disease and those in remission.
Whether that means that one can manipulate the gut bacteria to effect a more suppressive state remains to be seen, but the association is tantalisingly suggestive as a treatment option.
However, one would hope that the main intervention which might be possible in the future will relate to vaccination or desensitisation.
There is some seasonal variation in the incidence of GPA. This type of vasculitis looks as if it may begin in the upper airways, then extend to the lung and then become a more systemic disease in many cases, suggesting that perhaps the primary allergen which triggers the process is one which is inhaled.
That lends the possibility of identification of these antigens and then at the first sign of disease, considering desensitisation via nasal spray. It is very clear that that mode of desensitisation is more effective than other forms of desensitisation.
It is tantalising to imagine that at the first sign of somebody having a systemic illness, a widespread battery of tests would be performed on small drops of blood which would then turn up genetic markers equivalent to the ANCA that we use today. On finding this, the clinician could then embark on a nasal desensitisation program which hopefully will then downregulate the immune system’s response to that allergen and then turn off the whole disease process without any further dramatic interventions.
EGPA
Eosinophilia with granulomatosis and polyangiitis is another disease which lost its original name (Churg-Strauss vasculitis) in the shuffle which led to Wegener’s granulomatosis no longer being an eponymous immortality for a German pathologist linked to the Nazi movement.
The treatment of EGPA has remained similar to the treatment of GPA, which is to say maintenance corticosteroids, steroid-sparing agents and, in particular, cyclophosphamide. The experience with rituximab has been considerably less than with GPA, but, currently under PBS guidelines, one is allowed to prescribe rituximab for EGPA on the basis of angiitis.
Prognosis for EGPA is determined by its other clinical manifestations. It is considerably rarer than GPA and consequently, my personal experience with this condition is less than it is with GPA. It still carries a significant five-year and 10-year mortality, in part related to the disease manifestations and in part related to complications of therapy.
IN FIVE YEARS
IL-5 is critical for development and proliferation of eosinophils. Mepolizumab, an antibody to IL-5 has been found to be helpful in the management of EGPA and other IL-5 agents, including benralizumab and reslizumab, are in the process of being studied. Those results will contribute to determining the direction of therapy in five years’ time. In addition, prospective studies of rituximab in EGPA now being conducted will determine if this agent will continue to be used for this condition.
IL-5-dependent cell proliferation and survival is dependent on Janus kinase-signal transduction, as well as tyrosine kinases including BTK (bruton tyrosine kinase). This would raise the possibility that small molecules such as JAK inhibitors and BTK inhibitors (many of which are already licensed for treating haematological disease) might yet have their hand turned to the management of EGPA.
These would represent potentially dramatically new approaches to the treatment of eosinophilic diseases.
IN 20 YEARS
There is considerably less data on seasonality in EGPA than there is for other more common forms of vasculitis. EGPA occurs with an incidence of about one tenth that of GPA.
Nevertheless, the nature of the eosinophilia does raise the possibility that there is an allergic aspect to this as well. Therefore, desensitisation could well be a useful approach to therapies in 20 years’ time.
This is a condition where it is very clear that the eosinophil may directly cause damage to the myocardium through toxins in the eosinophilic proteins.
This is similar to what is seen in the hypereosinophilic syndrome.
The development of specific agents capable of blocking the effect of these chemicals would go a long way towards minimising tissue damage. In this situation, as is the case with GPA, tissue damage would have the potential to be modified by regenerative medical approaches which does require very specific stem cells capable of regenerating myocardium or nerve tissue along the lines of the discovery of specific stem cells for skeletal tissues.
POLYARTERITIS NODOSA
Polyarteritis nodosa is, with EGPA, the least common of the major systemic vasculitides.
Currently, the diagnosis is made on either deep tissue biopsy, angiography or electromyogram depending on the pattern of involvement.
It is important to recognise that cutaneous forms of polyarteritis are highly unlikely to ever evolve into systemic disease and their presence does not mandate the use of aggressive treatments. These are essentially benign local variants of vasculitis and usually do well with low-intensity treatment, such as corticosteroids in moderate doses, coupled with methotrexate.
There are significant differences between polyarteritis and the ANCA-associated vasculitides (AAV), particularly in terms of prognosis.
Polyarteritis has a much lower rate of recurrence than do the other forms of vasculitis and it would be far more typical to be a “one shot” disease while AAV is notorious for its tendency to recur.
There are no immunological markers equivalent to ANCA and thereby the rationale for rituximab is lacking. However, there are case reports of this agent being used in the management of polyarteritis with what seemed to be good results.
There are complexities to the diagnosis of polyarteritis on angiography, particularly related to the increasingly use of CT angiograms as a way of surveying vascular beds.
Unfortunately, the limits of resolution of CT angiograms do not lend themselves to a confident diagnosis of polyarteritis. One has to then perform selective direct injection of vascular beds to try and get down to vessels of 1-2mm diameter, which is typically the target vessel of polyarteritis.
While much attention has been placed on the presence of aneurysms as a form of diagnosis, the irregularity of vessels is probably a more common angiographic manifestation of polyarteritis, and one that needs to be searched for with a good vascular radiologist.
We have little to guide us in terms of treatment. There are no clinical trials of classical polyarteritis and we borrow from the trials of other forms of vasculitis which are rather more common.
Corticosteroids remain the mainstay of treatment and methotrexate or azathioprine are typically used as steroid-sparing agents, though depending on people’s preference, micophenolate mofetil or leflunomide may also be employed.
Cyclophosphamide is used for very aggressive forms of polyarteritis and then those forms which are associated with hepatitis B infection, which is increasingly rare in our community, the use of anti-viral therapies coupled with short-course steroids can lead to total remission of vasculitis with no evidence of recurrence.
I would not anticipate any great changes to our treatment options in five years’ time. I do not believe that there will be any clinical trials developed to investigate polyarteritis. Currently there are no such trials registered on clinicaltrials.gov.
At this point, I it is unlikely there will be any change to the way that we make the diagnosis, which is essentially established on either:
1. Tissue biopsy, usually muscle, or
2. Angiography, or
3. Electromyography demonstrating mononeuritis multiplex which in the appropriate context allows for a clinical diagnosis of polyarteritis.
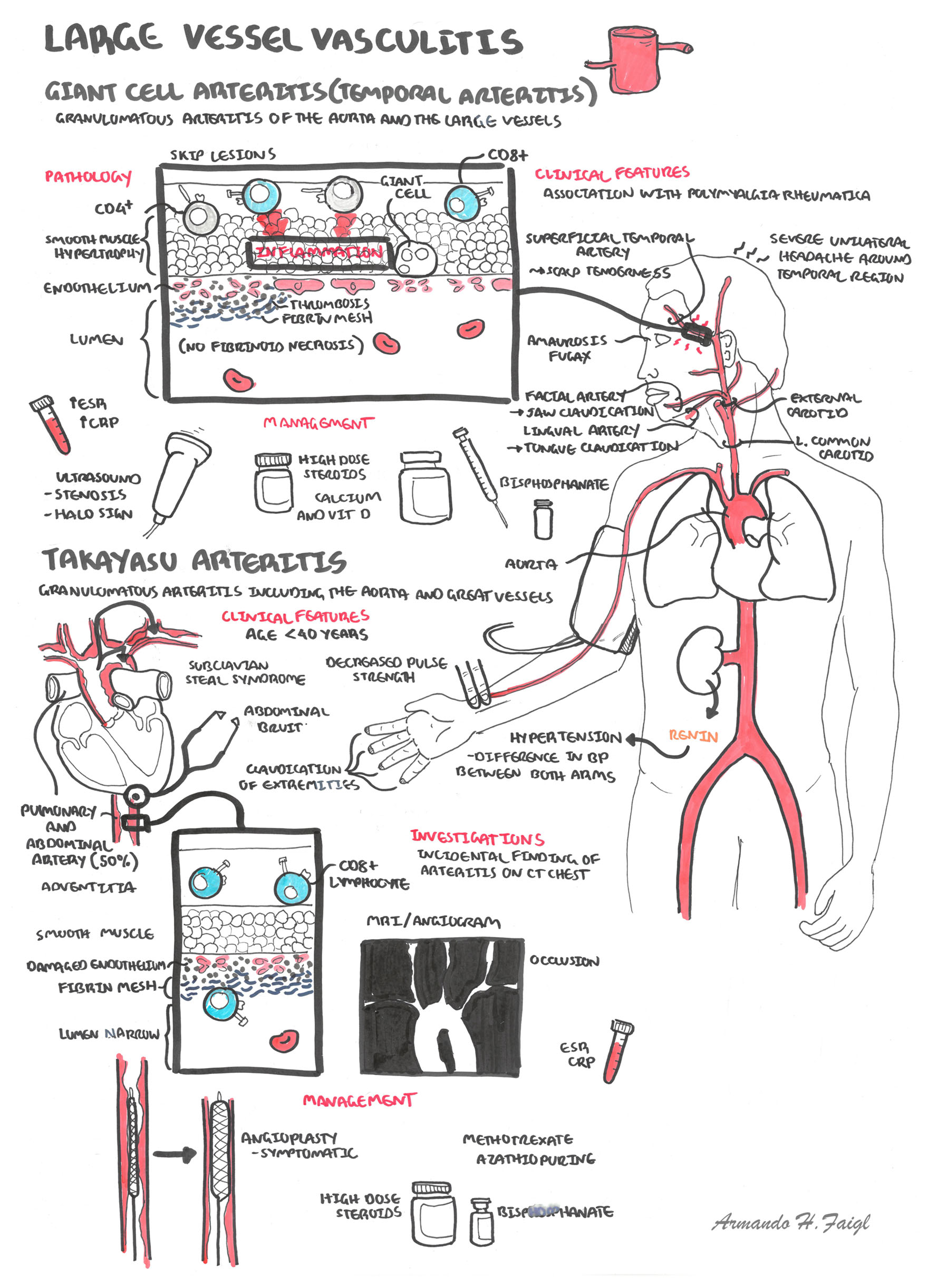
GIANT CELL ARTERITIS
The current state of play is that giant cell arteritis (GCA) has expanded its spectrum of involvement in recent years.
Having always been considered to be a classical condition of “cranial arteritis” characterised by headaches, visual loss, jaw claudication, scalp tenderness and association with polymyalgia rheumatica, the development of other imaging modalities has allowed the recognition of diseases which are centred more around other large vessels, particularly the aorta and its main branches, most commonly in the supradiaphragmatic aorta.
The probability of having positive temporal artery biopsy in the setting of having a positive imaging of large vessels is only about 50% and there seems no purpose served by pursuing the issue any further once the diagnosis of large vessel vasculitis has been established through imaging.
The approaches to establishing a tissue diagnosis have centred around whether one performs unilateral or bilateral biopsies. My prejudice has always been to perform bilateral biopsies based on studies which are now almost ancient.
However, more recent studies presented this year at the ACR have confirmed that the bilateral biopsies dramatically increase the probability of having a positive biopsy and that biopsies should be of 3cm on each artery or longer.
This will improve the yield on biopsy by a factor of two.
The treatment for large vessel vasculitis has still centred around corticosteroids.
Significantly, in cases of visual loss, there is absolutely no evidence that any treatment makes any difference in the first two weeks of therapy and it is in that first two weeks after presentation that a person who presents with visual loss in one eye has a 50% chance of developing visual loss in the contralateral eye.
It is very rare to lose vision after the first two weeks of high-dose steroids, virtually irrespective of how well controlled the GCA was.
We are currently in the throes of great enthusiasm for tocilizumab as a treatment for GCA based on the 12-month studies conducted by Roche and a smaller pilot study conducted independently as an investigator-initiated study from Switzerland.
It seems fairly clear that the use of tocilizumab will improve the inflammatory numbers so that ESR and CRP will decline substantially, leaving physician and patient much more comfortable engaging in progressive steroid reduction.
Systemic effects of this disease will also improve markedly with the resolution of fevers and polymyalgic symptoms.
However, there is considerable debate as to whether IL-6 inhibition actually makes a lot of difference to the large vessels themselves and there is considerable basic science data to suggest that thid might not be the case.
While there is clinical trial data suggesting that intravenous pulse steroids administered at the beginning of the treatment will allow more effective steroid reduction and a less accumulative dose of steroids over the longer term, there seems to have been very little enthusiasm for adopting this approach in the rheumatology community at large.
The vogue for commencing people on aspirin to prevent occlusive events is now waning and there is a recognition that the data supporting their use occurred not from interventional studies, but rather from observational studies that those people who developed the disease while on aspirin had a lesser risk of visual loss and other occlusive events.
Methotrexate has long been popular as a steroid-sparing agent and pooled analyses suggest that it might be of somewhat effective though it is fair to say that the two largest of the three trials which have been conducted of this treatment have not shown a positive result.
Nevertheless, rheumatologists do feel comfortable with methotrexate as a steroid sparing agent.I suspect that until something else better comes on the market, methotrexate will continue to be our default in terms of steroid-sparing options.
Experience with other treatments such as azathioprine, mycophenolate, leflunomide and cyclophosphamide has been very limited and anecdotal.
IN FIVE YEARS
My personal prediction is that IL-6 will have a role as a steroid-sparing agent, but it may well be that JAK inhibition through inhibiting both IL-6, reducing both IL-6 levels and interferon gamma levels may well prove to be more effective. There is one trial of a JAK inhibitor about to be conducted.
There is evidence suggesting that JAK inhibition will reduce interferon gamma levels, which is significant given that interferon gamma is the cytokine most associated with occlusive events in giant cell arteritis.
There have also been preliminary studies looking at abatacept which has yielded some positive results. Ustekinumab, which is an IL-12/23 inhibitor, has also been suggested to be of benefit in giant cell arteritis.
IL-12 is a significant factor promoting the generation of interferon gamma. Levels of IL-12 also correlate positive with IL-6 and it is thought that this agent might have the potential to also affect both the interferon gamma and IL-6 pathways, making it a promising agent for the treatment of giant cell arteritis.
Preliminary data using PET scanning has suggested methotrexate probably has little effect on vasculature in large vessel vasculitis, whereas IL-6 has a moderate effect. It is certain that neither of these agents will render an “inflamed” vessel to a non-inflammatory state as assessed by PET scanning.
It remains to be seen whether other agents that affect interferon gamma will be more effective in that regard and my prediction is that we will find that there will be a role for JAK inhibition.
In five years, the patent for tofacitinib will probably be coming to an end and therefore we have the possibility of having access to relatively inexpensive generic products capable of acting as steroid-sparing agents and modifying giant cell arteritis.
IN 20 YEARS
The prediction of what will happen in 20 years is rather more problematic.
Again, one would have to speculate that there are new agents. These new agents could either more specifically target blood vessels or have corticosteroid effect with abrogation of the risk of toxicity, which is the main long-term problem in giant cell arteritis.
There might possibly be novel agents directed at other phenomena.
We do have evidence that the innate immune system is involved in the genesis of temporal arteritis, and there is a strong correlation between patterns of toll-like receptors on different parts of the vasculature and the involvement of those different parts of the vasculature in different forms of large vessel vasculitis.
It is possible that this will give a clue as to what factors might be the triggers for different forms of large vessel vasculitis, and with respect to Takayasu arteritis as well as giant cell arteritis, it may well be that there will be very different triggers which could be addressed in quite different ways.
Once more I suspect that we will find the microbiome has influences on this type of inflammation and manipulation of the microbiome may prove to be very helpful and less toxic than current therapies.
The increased recognition that biological drugs have an effect on the microbiome and the microbiome has an effect on the immune state does lend for the possibility that gut manipulation of bacteria might end up becoming a mainstay of treatment in 20 years time.
Dr Stephen Hall is a private practice rheumatologist with a long interest in vasculitis and a commitment to conducting clinical trials