When neither Medicare nor your MDO has a clue, what do you do?
Two commonly billed MBS physician items – 132 and 133 – were recently targeted by the Department of Health compliance team.
The initiative was a perfect example of how no one understands how Medicare works, including Medicare.
Item 132 is an initial attendance on a complex patient with multiple morbidities, taking at least 45 minutes, and involving the preparation of a detailed treatment and management plan. Item 133 is the follow-up of at least 20 minutes, when the plan is reviewed. Item 132 is limited to once per patient, per year, and item 133 twice per patient, per year.
So, when specialist rehabilitation physicians started receiving letters from the department that contained the below paragraphs, they were understandably confused.
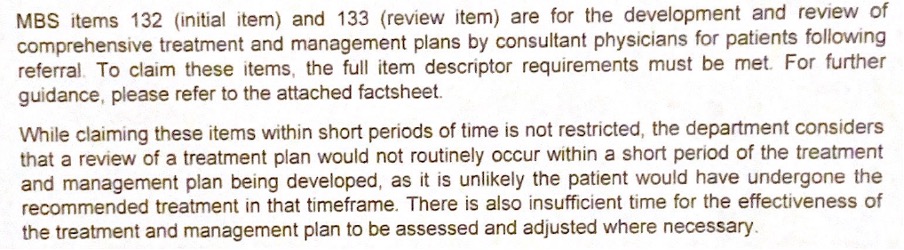
The specific concern described in the letters was the timeframe between billing item 132 and 133. The physicians had claimed the services within a two-week period, and the imputation was that this was too short.
Importantly, all of the claims were for inpatient services, which had been billed using gapcover schemes through the patients’ private health funds, and the physicians I spoke with typically worked in regional private hospitals without registrar or JMOs, meaning they did all the work themselves, and spent the appropriate time with patients.
One provider told me their MDO had asked where in the MBS it says that these services can be claimed in a hospital, because the letter suggested they were only billable in the outpatient setting. He said “I was dumbfounded. I have never seen anyone imply you can’t use a 132 in hospital. What is going on?”
Another provider told me that when they called their MDO, the medico-legal adviser they spoke with was a GP who advised them to pay all the money back because it is not possible to fulfill all relevant requirements within a two-week period. The advisor apparently said to them that patients wouldn’t even have managed to make an appointment with an allied health practitioner in that time, let alone commence treatment.
The physician was gobsmacked and described feeling completely rudderless because even the MDO didn’t seem to have a clue.
The physician asked me whether they should just follow the MDO’s advice and pay the money back. Had they done something wrong?
The answer was no, on both counts, and it’s a lesson in the importance of detail, nuance, and context.
Firstly, of course these items can be claimed in the inpatient setting. But as is often the case with the MBS, this is nowhere clearly stated. We instead have to work it out by inference. Firstly, there is a 75% rebate available (the inpatient rebate), secondly, there is an absence of a specified setting in the item descriptions which suggests the services can be provided anywhere, and thirdly, the private health insurers (PHI) have always reimbursed these services.
It is legally impermissible for PHIs to cover outpatient services, and PHIs are very good at not paying for things they are not required to cover. So, the fact that the PHIs have always reimbursed these services is the most compelling evidence we have that they are available for hospitalised patients. Not perfect, but it’s the best we have.
The concerning issue for the physicians I spoke with was that that the DoH did not appear to understand what happens when a patient is admitted to an inpatient rehabilitation unit. They seemed to have no capacity to comprehend the MBS beyond a narrow outpatient focus, and were erroneously confusing the work of community-based GPs with hospital-based physicians.
When GPs prepare management plans, they send patients into the community to access isolated therapists, but this is not what happens in hospital. For example, to achieve accreditation, a hospital rehabilitation department must have an onsite gym and therapists to enable the multidisciplinary team to start progressing proposed rehabilitation protocols and goals (the item 132) immediately.
If you think about rehabilitation planning for a patient after a fractured hip, the initial goal may be to get the patient home. The protocol and goals are then assessed and adjusted regularly throughout the admission, which would usually be around two to three weeks, because PHI contracts ensure admission lengths are as short as possible. A multi-disciplinary rehabilitation team therefore works diligently from the moment the item 132 is completed and communicated, because no one can afford to have a length-of-stay blowouts.
But, if the original goal cannot be achieved within two weeks, and it is apparent the patient will need respite care in a nursing home, the plan has to change, and the relevant consultation would usually involve an item 133 service.
After comprehensively reviewing their records and concluding all MBS criteria for every item 132 and 133 claimed had been met, the rehabilitation physician composed a lengthy reply to the department explaining that they had complied, would not be making any repayment, and pointing out that nowhere in the legislative scheme is there any indication that 133 is excluded within two weeks of item 132, and in fact, it makes no sense to suggest it should be, in the inpatient setting.
Meanwhile the MBS review taskforce suggested that the solution to problems with time-based item numbers such as these, was to add more time-based item numbers.
I think it’s a little more complex than that.
Dr Margaret Faux is a health system administrator, lawyer and registered nurse with a PhD in Medicare compliance, and is the CEO of AIMAC, which offers courses and explainers on legally correct Medicare billing.


