No well-informed patient would want to undergo such an intervention, a new international guideline suggests.
An international expert panel has called for a list of interventional procedures for chronic spine pain to be used only in research settings.
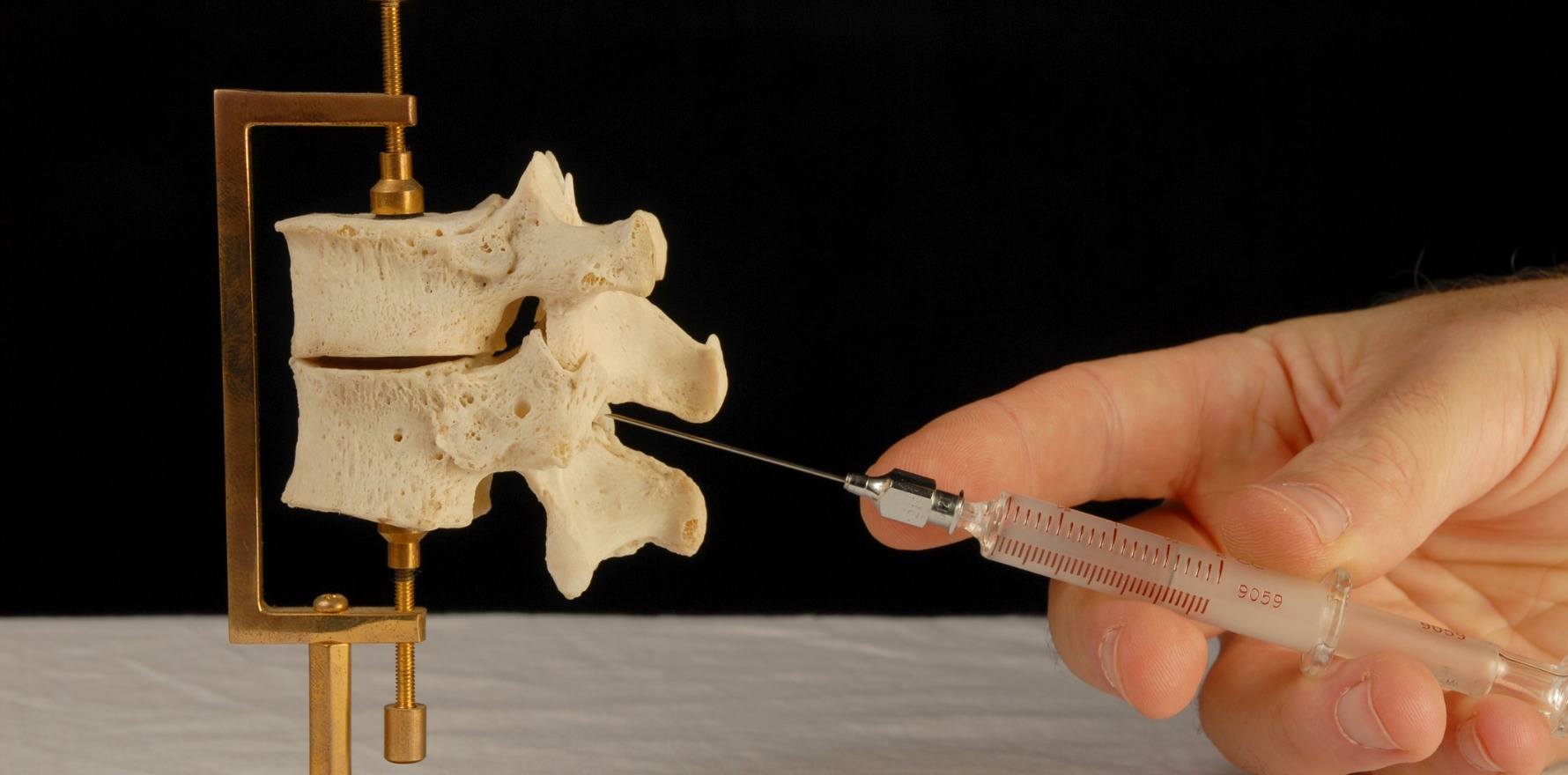
Interventional procedures such as epidural injections and nerve ablations have become common in the management of chronic spinal pain, yet the evidence supporting their use is tenuous at best.
Now, a new set of clinical guidelines, published in the BMJ, concludes that 13 commonly used procedures for spinal pain offer little to no benefit on pain relief and other important outcomes when compared to sham treatments.
“Despite the common use of spine injections in pain clinics around the world, it has been hard to come up with evidence that strongly supports this practice when applied to chronic back pain … The research and guideline recommendations are worthy of attention,” wrote Professor Jane Ballantyne, an anaesthesiologist from the University of Washington, in an accompanying editorial.
The international panel consisted of 10 healthcare professionals with experience in managing chronic spinal pain (a mix of anaesthesiologists, rheumatologists, physiotherapists, rehabilitation specialists, and epidemiologists), as well as four people with lived experience of chronic spinal pain. The individuals with lived experience had undergone a range of interventional procedures for their pain.
Importantly, no panel member had any financial conflicts of interest or had any strong opinions on the use of interventional procedures for chronic spinal pain at the outset of the process.
The panel undertook a systematic review of more than 130 trials – and network meta-analysis of some 8000 patients across 80-plus trials – of 13 different interventional procedures on eight outcomes, including pain relief, physical functioning, return to work, opioid use and opioid events.
Procedures examined as part of the review included epidural, joint-targeted and intramuscular injections of local anaesthetic and/or steroids, dorsal root ganglion radiofrequency and certain nerve ablation procedures.
“There was no high-certainty evidence of important pain relief (or benefit on any other effectiveness outcome) for any intervention for either chronic axial spine pain or chronic radicular spine pain,” the panel concluded.
“[In addition,] all interventional procedures supported by moderate or low-certainty evidence showed little to no pain relief compared with sham procedures.
“All or nearly all well-informed people would likely not want such interventions. Such interventions should not be offered outside of a clinical trial.”
Related
Professor Ballantyne felt the findings brought into question whether it was reasonable to continue to offer these procedures to patients.
“Chronic back pain is highly prevalent, a great deal of money is spent on the injections and a lot of patients’ hopes and expectations are vested in this type of treatment,” the former chief of pain medicine at Massachusetts General Hospital in Boston wrote.
“[But] it is never easy to change entrenched culture, and injections have undoubtedly become entrenched as a key component of pain clinic treatments.”
However, Professor Ballantyne noted that broader changes to healthcare funding systems may help change how spinal injections are viewed and used.
“There are many pressures on providers to keep doing spinal injections, and on payers for paying for them, but the more the evidence fails to support the widespread use of these injections, the less inclined healthcare systems will be to fund them.
“[These findings] will not be the last word on spine injections for chronic back pain, but it adds to a growing sense that chronic pain management needs a major rethink that is perhaps best achieved by a better balance of reimbursements between procedural and non-procedural chronic pain treatments.”