An 80-year-old gargoyle showing what body parts loom largest in your brain may also explain this phenomenon in chronic pain.
Why would a patient with persisting pain in their leg begin to develop symptoms in their face?
Why would an amputee one day experience pain in their genitalia – or orgasm in their missing foot?
When people suffer from persisting pain for months or years, their brains can begin to lose precision in identifying body parts.
The phenomenon is known as “central sensitisation”, but Australian pain scientists Professor Lorimer Moseley and Dr David Butler call it by the more evocative name of “brain smudging”.
When it occurs, pain messages coming from the peripheries might become blurred and confused, making it harder for the brain to understand which area exactly needs protection. Patients begin to feel the pain moving across their bodies and slowly conquer areas seemingly unrelated to the initial injury.
Some of our understanding of this effect comes from the work of Professor Herta Flor, a neuroscientist at Humboldt-University in Berlin, who in 1995 set up an experiment to understand the origin of chronic phantom limb pain in arm amputees.
Previous studies on adult macaques had suggested that the plasticity of the somatosensory cortex – the part of your brain that receives and processes sensory information from the entire body – could account for some non-painful phantom limb phenomena in amputees but had a pain-preventing function.
But other theoretical and empirical work on chronic back pain had revealed a relationship between the amount of cortical alteration and the magnitude of pain.
Professor Flor and her team hypothesised that phantom limb pain could also correlate to changes in the somatosensory cortex.
To demonstrate their hypothesis, the researchers looked at the brain of 13 upper-limb amputees using non-invasive neuromagnetic imaging techniques while pressure stimuli were applied to either side of their lip.
Those who suffered from chronic phantom limb pain showed changes in the region of the somatosensory cortex where the missing arm is located.
“We don’t know if they are the cause or the consequence, but those brain changes are associated with phantom limb pain,” says Professor Flor, now scientific director of the Department of Cognitive and Clinical Neuroscience at Heidelberg University in Germany.
Why would anyone feel pain in the arm when poked in the face?
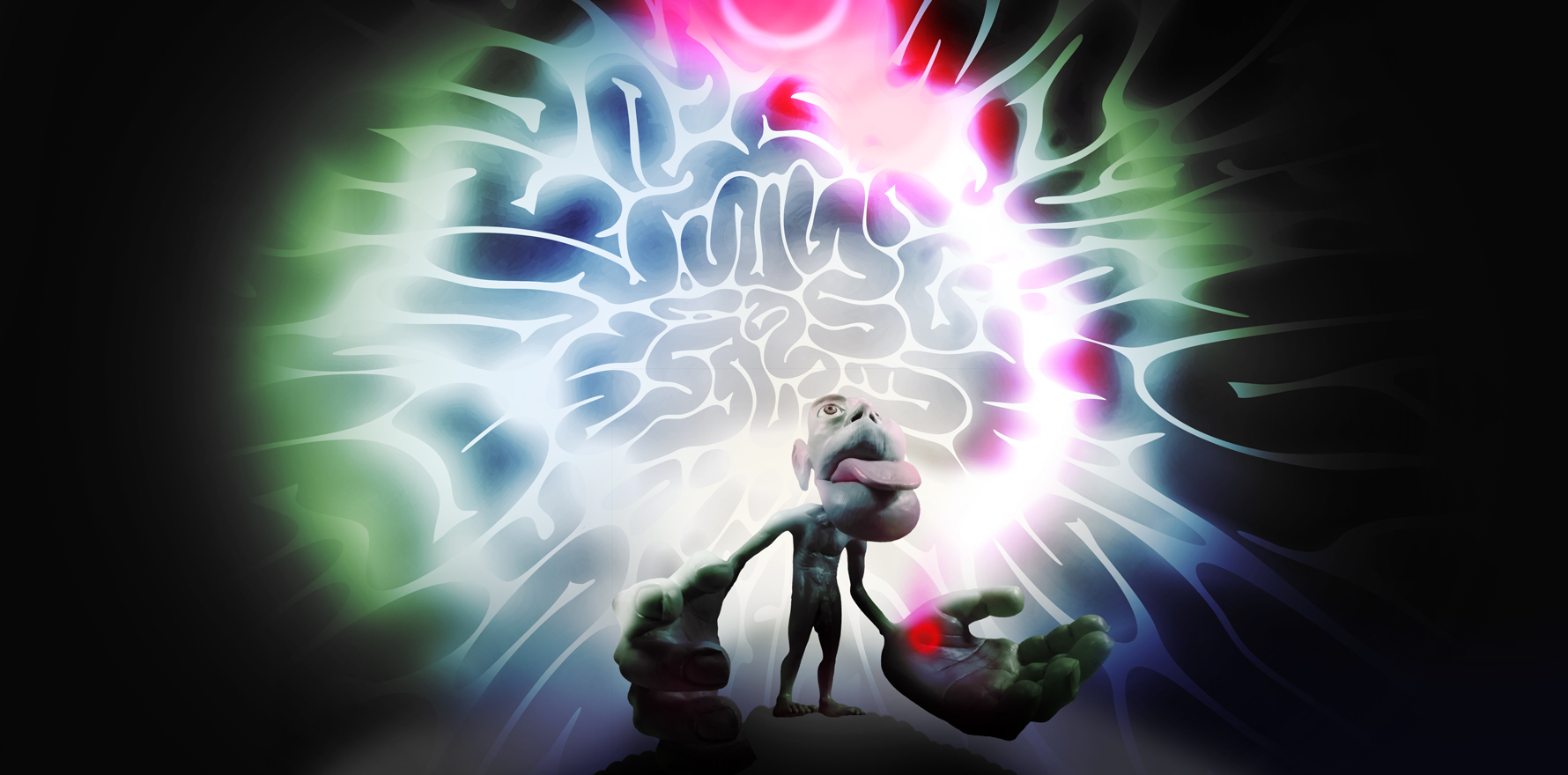
The somatosensory cortex contains a map of our body – the so-called somatosensory homunculus.
The homunculus, “little person” from Latin, represents a tiny human being inside our brain and maps what areas of the brain oversee each part of our body.
This mapping results from the way connections in the brain are ordered and arranged. The ordering of neural pathways between different parts of the brain and those going to and from our sensory organs produces specific patterns on the brain surface.
The somatosensory homunculus was created by neurosurgeons Wilder Penfield and Edwin Boldrey in 1937. This grotesquely malproportioned little octogenarian is still one of the most represented figures in modern neuroscience (and still notably male, for relative lack of attention to the female somatosensory cortex).
Penfield and Boldrey used the data from electrical brain stimulations of 126 live and awake patients between 1928 and 1936. The patients had received only local anesthesia so that they could be relied upon to participate by giving verbal recognition of sensation and elicited movements.
The two neurosurgeons were treating these patients for severe epilepsy. Penfield assessed the related sensory and motor functions using electrical stimulation paired with the patient’s verbal or movement feedback to determine the correct brain areas to treat.
For each patient, Penfield and Boldrey painstakingly recorded each stimulation point. They then generated the somatosensory homunculus from 170 stimulation point maps indicating the number and location of the stimulation points for each body part.
These sensory maps of the brain do not map “areas” of sensation onto equivalent areas of the cortical surface. But the more receptors there are in a given area of skin, the larger that area’s map will be represented on the surface of the cortex. As a result, the size of each body region in the homunculus is related to the density of sensory receptors.
Our hands, for example, take up a large area of the map because they are an instrumental and sensitive part of our body. We know exactly where our hands are in space and what they are doing, if they are being touched or are touching something. We can move our fingers in space with great precision – some of us use them to play the piano, others to perform delicate surgeries.
The representation of our hands in the brain isn’t static. If we taped our left index and middle fingers together for a while, the representation of our left hand in the brain would change. But within a few hours from restoring normal movement, the representation of the left hand in the brain will reverse—the magic of cortical plasticity.
A similar phenomenon occurs when people suffer from persisting pain.
If a patient has experienced pain in their index and middle finger, they are frightened to move them and limit their use, the brain might conclude that the two fingers need extra protection and call upon neighbouring parts of the brain to help out. The brain map of the patient’s hand changes.
This remarkable defence tactic might be helpful in the short term, but in the long term, the patient might begin not to be able to distinguish one finger from the other or use them with great precision and independently.
The pain might start to smudge to other areas of the hand and even the rest of the body.
Misplaced pain
Smudging is a metaphor that refers to the changes in the brain areas devoted to detecting the stimulation of body parts and performing functions that begin overlapping. This process can explain why some body parts may become difficult to use, or other areas become sensitive compared to the injured area.
Here is what happens at a neurobiological level.
Imagine two nociceptive neurons sitting next to each in the brain. Each neuron receives nociceptive stimuli from a specific location in the body. Nearby neurons receive stimuli from nearby body locations. An immune cell sits on top of these two neighbouring neurons and modulates the communication between them – the three cells form a synapse.
Now imagine a second synapse adjacent to the first looks after the adjacent body location, and so on. This is how our brain accurately localises painful stimuli in normal circumstances.
In a patient with persistent pain, synapses that receive stimuli from the body part in pain are constantly “turned on.” Immune cells move within the central nervous system towards areas of elevated activity and release chemicals, called neurotransmitters, that make neurons more responsive. Excess of these chemicals start to leak out and activate more synapses in proximity. Now the patient feels pain over a larger area that is less specifically localised.
Because the face representation in the somatosensory homunculus is next to the representation of the arm, Professor Flor explains, in upper-limb amputees who suffer from chronic phantom limb pain the two areas overlap.
“This process is at play in every form of chronic musculoskeletal conditions,” says Dr Daniel Lewis, a rheumatologist and chronic pain specialist in Melbourne. Central sensitisation, he says, is a driver of the fibromyalgia pain patterns, for example.
“If you put somebody who doesn’t have chronic pain in a functional MRI scanner and you whack them on the thumb, the thumb area of the brain will light up. But if you did the same experiment with someone with fibromyalgia. The brain lights up like a Christmas tree.”
The contemporary understanding of how the brain changes in patients with persisting pain supports the biopsychosocial model of pain and suggests that a multidisciplinary, non-pharmacological treatment of chronic pain is the best practice, says Dr Lewis.
“People keep chasing that pain as if it was an ongoing injury,” he says. “More rheumatoid arthritis, more drugs. More back pain, more injections in the spine.
“It’s the brain amplification, not the injury that’s causing the problem.”
Neural plasticine
If brain plasticity is the problem, brain plasticity can also be the solution.
In treatment studies, Professor Flor stimulated the residual limb stump of arm amputees with electrodes then asked them to identify the exact location of the stimulus on the stump.
She noticed that those who did not suffer from phantom limb pain could efficiently complete the task. But those who had struggled with persisting pain could not tell where the stimulation had been applied.
However, Professor Flor noticed that the more these patients practised, the better they became in differentiating one location from the other. As a consequence, their pain gradually decreased. They had started to remap their brain.
A similar study is currently under way in Australia for people who suffer from chronic back pain. In one experiment, participants are touched in random locations of their back with either a wine cork or a pen lid. Their task is to identify what tool was used and where exactly they had been touched. In another experiment, participants have to guess a letter or a number the researcher draws on their backs.
Professor Moseley, foundation chair in Physiotherapy at the University of South Australia and one of the scientists involved in this study at NeuRA (Neuroscience Research Australia) says this sensory discrimination training helps patients reinstate brain precision.
“[The training] works a bit like a fine tuner on your radio,” he says. “It recruits these complex and potentially powerful brain mechanisms to fine-tune the signals that are coming in.”
All experts interviewed by The Medical Republic agree that educating patients on pain neuroscience and central sensitisation is the first step to recovery. “It reassures people that their body is not becoming more broken,” says Professor Moseley.
“If your pain is spreading from your lower back to your neck, it’s very unlikely that you have a back problem that’s spreading up. It is way more likely that your brain is losing the precision in localising body parts.
“It can be quite reassuring.”
“That is the way we treat fibromyalgia,” agrees Dr Lewis. While most rheumatologists in Australia prescribe medication as the first step of therapy, he says, treatment of fibromyalgia and other rheumatoid diseases should begin with pain neuroscience education.
“The first step is reassurance that we are dealing with a central sensitisation process. It’s an educational process.”
Professor Moseley adds that because central sensitisation is caused by an immune system response, anything that calms down the immune system can help.
“Green leafy vegetables, reduce your simple sugars, exercise, get your 7.5-8 hours sleep – all those things are relevant when the immune system is overactive.
“One more reason to have a healthy lifestyle.”