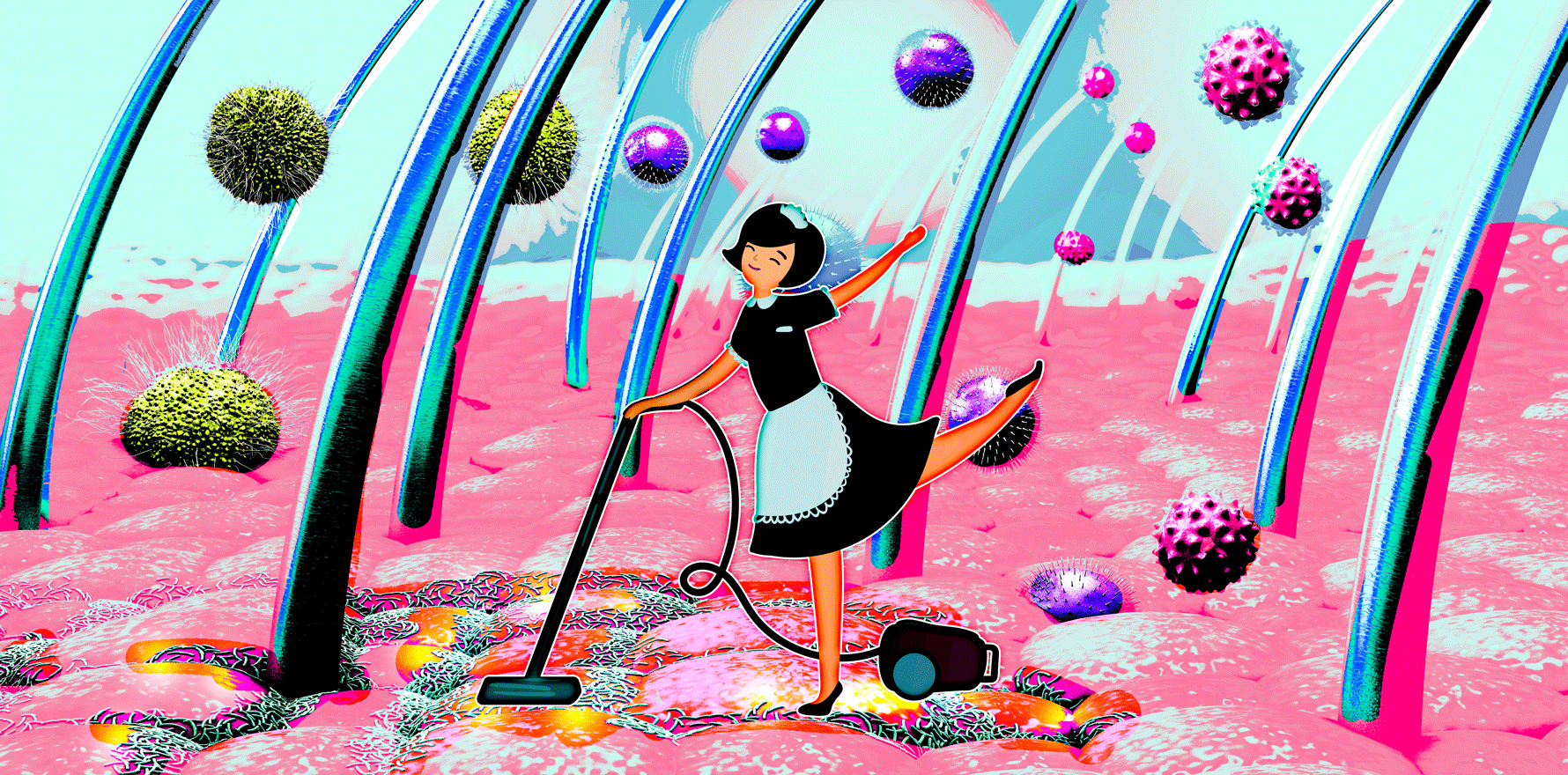
Understanding our microbial communities paves the way for new bacteria-targeting treatments for acne and other dermatological conditions.
Overnight, Chris Callewaert acquired body odor. The bioengineer, then a student, had led a largely odorless life. But several years ago, in the space of just 12 hours, he suddenly noticed that he had acquired a distinctly unpleasant smell. The question of what and why has since set him on a scientific mission to understand how the population of bacteria, viruses, and fungi that colonize human skin—known as the skin microbiome— can influence the body’s fragrance.
“From birth on, our skin microbiome then goes through an evolution throughout life,” says Callewaert, now a postdoctoral fellow at Ghent University in Belgium who also goes by the name of “Dr. Armpit” on account of his research focus. These changes are influenced by internal factors such as diet, immune system function, and diseases, and also by external factors like pollution and microbial exposures, he says. Callewaert suspected that his swift transformation from odorless to smelly was related to such a change in his skin microbes. “I somehow knew that that had to do with bacteria,” he says.
While research on the skin microbiome lags years behind studies of the gut microbiome, there is now emerging evidence that microbial imbalances, or dysbiosis, on the skin could play a role not just in body odor but in conditions including acne, eczema, and even autoimmune diseases such as psoriasis. The pharmaceutical sector is showing keen interest in the subject; already, deals worth hundreds of millions of dollars are being made by companies including GlaxoSmithKline, Sanofi, and Bayer, as the industry looks for ways to alter the skin microbiome to treat dermatological conditions that until now have been relatively underserved by medicine.
But while the microbiome that covers each person’s roughly two square meters of skin might be more accessible than that of the gut, that doesn’t mean it’s equally amenable to scientific study or manipulation, say researchers who spoke to The Scientist. There is also a risk that adding or removing species could destabilize the delicate balance of organisms and potentially do more harm than good. Although he sees a bright future in this area of research, Callewaert, who now holds patents on the use of prebiotic (substances that selectively nourish or inhibit specific bacteria) and probiotic treatments for body odor, says “it’s also very complex. . . . There’s thousands of species, and they all have an influence.”
What lives on the skin?
Sara Saheb Kashaf has long been interested in atopic dermatitis and the possibility that the condition has ties to the skin microbiome. Antibiotics have been shown to work as a treatment for the condition, which causes red and itchy skin, suggesting a microbial influence. But when she started digging into the problem a few years ago, “it was really interesting to me that we didn’t really know the true composition of the microbiome of our skin,” she says.
To address this, the MD/PhD student, based at the European Molecular Biology Laboratory’s European Bioinformatics Institute in the United Kingdom and at the US National Institutes of Health, recently conducted a comprehensive survey of skin microbes. Each of a dozen or so volunteers had samples taken from multiple sites on the body—including the forehead, hands, feet, groin, armpits, and ears—and some of the volunteers were sampled again on three or four different occasions over several years.
Saheb Kashaf and colleagues used metagenomic sequencing to detect the genes in each sample, and then employed computational methods to reconstruct individual genomes and identify the organisms present. Two key challenges were the low biomass of microbes on the skin and the risk of environmental contamination, so for every patient sample, the team also took a negative control by waving a swab in the air. “The microbial load is that low that you need to do that, or else you end up thinking that microbes that are really contaminants of your reagents are parts of your microbial community,” says study coauthor Julie Segre, a microbial genomicist and senior investigator at the National Human Genome Research Institute.
Overall, the team’s study identified 622 species of microbes, including 174 new-to- science species of bacteria, 12 fungal species, and 20 types of large bacteria-killing viruses known as jumbo phages. The exact composition of the skin microbiome varied by body part. For example, the area between the toes was teeming with viruses, the back of the head was dominated by the well-known skin-dwelling Cutibacterium, the bottom of the heel housed almost entirely Staphylococcus species, and the cheek microbiome featured the greatest relative abundance of a newly identified bacterial type, which the team dubbed Candidatus Pellibacterium.
The team also found that the microbiome changed at different rates over time depending on the body site. “In oily sites, we had [low rates of change] in the microbiome,” Saheb Kashaf says. In regions such as the back of the head, the crease alongside the nose, and the cheek, the makeup of the microbiome hardly changed over the course of the study. “But then there were other body sites, which may be very intuitive, like our hands and feet, that are constantly in flux,” she says, adding that much less is known about what microbial species live on these sites.
Despite these variations, other research has shown that the overall skin microbiome changes throughout our lifetime in such a predictable fashion that its composition can be an accurate predictor of age. Belgian biotechnology company S-Biomedic has characterized some of these changes in the microbiome of the face, and the Cutibacterium species that dominate there.
There is already considerable interest in altering the microbiome by eliminating pathogenic species, transplanting beneficial species, or selectively engineering microbes so as to reduce harm or increase benefits.
The abundance and composition of this part of the skin microbiome are affected by major life events, says synthetic biologist Bernhard Päetzold, S-Biomedic’s cofounder and chief scientific officer. “Right when we are born, in the first days, there’s a lot of Cutibacterium that then disappears,” says Päetzold. “It stays flat until the moment when puberty comes, and at that moment, our sebaceous glands switch on.” When those glands become active, they create the perfect environment for Cutibacterium, he says, and the microbe becomes the dominant inhabitant of the follicles connected to those glands.
The association between increased Cutibacterium and puberty had suggested to some researchers that the bacterium’s presence was a major contributor to adolescent acne, leading biotech companies such as S-Biomedic to investigate the species as a therapeutic target. But it appears the simplistic notion of “good” and “bad” microbes—a healthy or unhealthy microbiome— doesn’t capture the true nature of microbial diversity and how it influences health and disease, says Päetzold, making the question of how to treat skin conditions a challenging one to answer.
Good or bad microbes
Segre says that there isn’t yet a good sense of what makes a skin microbe beneficial, but there are some obviously pathogenic species that set off alarm bells. One of these is methicillin-resistant Staphylococcus aureus (MRSA), which can cause infections of the skin as well as of the lungs and bloodstream. The mere presence of MRSA—in the nose, for example— poses such a threat that people going in for surgery who are found to carry the bacterium are given prophylactic antibiotics to clear it, Segre says. Another pathogen Segre has worked on is the fungal species Candida auris, which is classified as a global health threat because of its association with bloodstream infections that are resistant to common antifungal drugs.
But that’s where the easy labelling of “bad” microbes ends. For example, Cutibacterium has been unfairly demonized, Päetzold argues, as one of several bacteria thought to be a causal factor in acne. “There was this conundrum: people said it must be a bacterium causing acne because when we put antibiotics or disinfectants on, [acne] gets better,” he says. But Cutibacterium is also commonly found in people without acne.
Päetzold says acne is likely the result of interactions between particular strains of Cutibacterium and the person they’re living on. “If you have a host that is particularly resilient to acne-inducing factors, you could have a more aggressive strain on your skin and you wouldn’t see anything,” he says. “But if you’re a person who is susceptible to it, it’s very important which strains you have and which ones are there, because that can shift the balance [of the skin microbiome] over” to an acne-promoting composition.
Similarly complicated is our skin’s relationship with S. aureus. Even strains that aren’t methicillin-resistant can be associated with flare-ups of atopic dermatitis. Moreover, Saheb Kashaf notes, while the bacteria become more abundant during disease flares and decline as symptoms start to improve, it’s not clear whether these dynamics are a cause or a consequence of the disease. “Is this Staphylococcus species just expanding on this dermatitic skin because [this environment provides them] the nutrients that they need to survive?” she says. “Or is it actually playing a part in the disease process? Is it worsening the symptoms of these patients by having these species on their skin?”
Shifting the balance
Despite unanswered questions such as these, there is already considerable interest in altering the microbiome by eliminating pathogenic species, transplanting beneficial species, or selectively engineering microbes so as to reduce harm or increase benefits. In 2020, Bayer invested $8 million in US medical dermatology biotech company Azitra, which has focused on identifying potentially beneficial strains of Staphylococcus epidermidis for use in skin care products and in therapies for conditions such as atopic dermatitis. Sanofi spent an undisclosed sum in 2021 to acquire Austrian company Origimm for its vaccinebased immunotherapy, which targets Cutibacterium—specifically C. acnes.
A targeted, species-specific approach to microbiome tinkering is favored by Parisbased biotech company Eligo Bioscience, which late last year signed a research agreement with GlaxoSmithKline worth up to $224 million to develop a CRISPR-based approach to treating acne. Edith Hessel, a mucosal immunologist and chief scientific officer at Eligo, says that when it comes to the skin microbiome, precision strategies are better than transplants like the ones that have shown promise in manipulating the gut microbiome to treat conditions such as ulcerative colitis and Clostridium difficile infection. In her view, transplanting new species or removing existing species carries “a big risk of causing dysbiosis.”
Eligo’s platform targets bacterial genes specifically associated with diseases of the skin and other organs—for example, the company has worked on the Shiga toxin gene that is found in some E. coli bacteria and is a cause of gastroenteritis. Using CRISPR to introduce a double-stranded break in the DNA of that gene selectively kills any bacteria carrying it. CRISPR methods can also selectively disable a gene, such as one for antibiotic resistance, without killing the bacteria. “The ability to alter a gene but leave the bacteria in place has tremendous applicability,” Hessel says. Like Sanofi, the company is using its platforms to develop treatments that target C. acnes, which, while associated with conditions such as acne vulgaris, is also important for skin health. “You don’t want to completely eliminate the C. acnes bacteria because it actually does a lot of good for health,” she says. “You want to very specifically just eliminate those C. acnes [strains] that carry disease-associated genes.”
There isn’t yet a good sense of what makes a skin microbe beneficial.
Others have more hope for the directtransplant route. After his own experience acquiring body odor, Callewaert conducted a trial involving 18 volunteers with body odor who received a course of spray-on transplants of skin microbiome samples cultivated from a non-malodorous donor, usually a family member. He says that early results, still unpublished, hint at improvements in recipients’ body odor, as assessed by a panel of eight trained odor assessors, for at least a month following treatment, although the lack of a control group prevents clear conclusions. Callewaert says he managed to get rid of his own acquired body odor partly by using this method, although it took three years to do so.
Another team of researchers, including Päetzold, did an open-label pilot study a couple of years ago in which eight volunteers with mild-to-moderate acne received one of two topical formulations containing a mix of C. acnes strains that are associated with healthy skin. After participants applied their formulation twice daily for five weeks, the team saw the composition of the facial skin microbiome shift toward the transplanted species, and noted a decrease in the frequency of non-inflamed lesions— the precursor of inflamed lesions characteristic of acne—but no significant decrease in inflamed lesions themselves at six weeks. However, the authors commented in their paper that the treatment duration was short, and the study lacked a control group, meaning the role of the formulations in the reported changes was unclear.
Segre is interested in whether it’s possible to alter the skin microbiome using a prebiotic approach—that is, applying treatments containing particular nutrients that shift microbial community composition— in conditions such as atopic dermatitis. There’s also the possibility of using the microbiome as a way to predict when disease flares might occur, she says. “For example, with the studies we do on atopic dermatitis or eczema, we’re looking at: When do you see changes in the skin microbiome, and when does the child or the parent start to perceive that the kid is having a flare of eczema?” She envisages a future when treatments for conditions such as eczema could be tailored to an individual’s skin microbiome profile, and analyses of one’s skin microbiome could enable early intervention with preventive treatments to stop flares before they develop.
Getting to that point will require a much better understanding of the many and varied species of microbes that inhabit the skin. On this front, Segre says she’s excited by the possibilities offered by technologies such as metagenomic analysis. “With these genomic advances, we can more fully identify all of the components of the skin microbiome: the bacteria, the fungi, and the viruses,” she says. “We can even see bacteria that we can’t yet culture, but we know their genomes, and that means that we can see things that we never could see before.”