The options for shoulder dislocations and replacements are becoming more sophisticated
The options for shoulder dislocations and replacements are becoming more sophisticated. Here’s an update on developments
Shoulder dislocation
Shoulder instability is classified according its direction (anterior, posterior or multidirectional) and onset (traumatic or atraumatic). Anterior traumatic dislocations are most common; the typical patient is male, in his teens or 20s, sustaining the injury during contact sports.
Anterior dislocations usually occur when the shoulder is in abduction or external rotation, leading to injury of the labrum, capsulo-ligamentous structures, glenoid and humeral head. The Bankart lesion, an avulsion injury of the antero-inferior glenoid labrum is the most common injury. Glenoid rim fractures may occur and are generally small.
Larger areas of bone loss from the glenoid decrease the distance the humeral head must translate to dislocate. The Hill-Sachs lesion of the humeral head occurs when the postero-superolateral bone of the dislocated humeral head impacts on the hard, anterior glenoid rim.
These lesions are classified according to size, but the orientation of the lesion and its combination with glenoid bone loss is more significant. If the Hill-Sachs lesion is parallel to the glenoid rim in the abduction/external rotation position, it is termed an “on-track” lesion. Combined glenoid and humeral head bone loss is termed “bipolar” bone loss. Hence an on-track Hill-Sachs lesion with bipolar bone loss and a large glenoid lesion is the most severe combination of bony pathology.
Management
After reduction, the arm is traditionally immobilised in a sling in internal rotation for a few weeks followed by a period of rehabilitation with physiotherapy. However, there is little evidence to support a period of immobilisation of more than one week. There is also debate about whether the arm is best immobilised in internal or external rotation.
Theoretically, external rotation keeps the capsule in contact with underlying bone, suggesting that if healing were to occur in this position that recurrent dislocation rates would be lowered.
However, the external rotation sling is cumbersome and inconvenient, and there is little clinical data to support its use. The recurrence risk of instability is 25-95% and correlates with age and sex, being highest among males in their early 20s or younger.
Multiple recurrences are associated with the development of shoulder arthritis. As a result, it is becoming increasingly common to consider surgical intervention after first dislocation particularly in high-risk individuals, so referral to a shoulder surgeon is recommended in all patients sustaining a dislocation episode.
A Bankart lesion is treated by arthroscopic capsule-labral stabilisation using several anchors which are inserted into the glenoid rim. The recurrent dislocation rate after surgery for a Bankart lesion is around 10%.
Recurrence rates in the setting of bone loss are higher and so other techniques are employed such as bone grafting the anterior glenoid (using the coracoid process – the Latarjet procedure – or iliac crest bone graft) or by addressing the Hill-Sachs lesion (most commonly by filling the defect with capsule and infraspinatus tendon – the Remplissage procedure).
Reverse shoulder arthroplasty
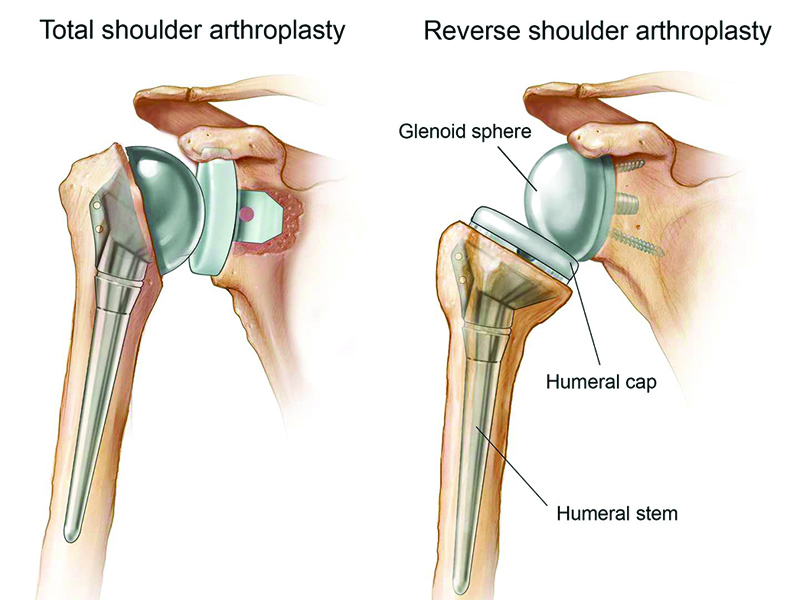
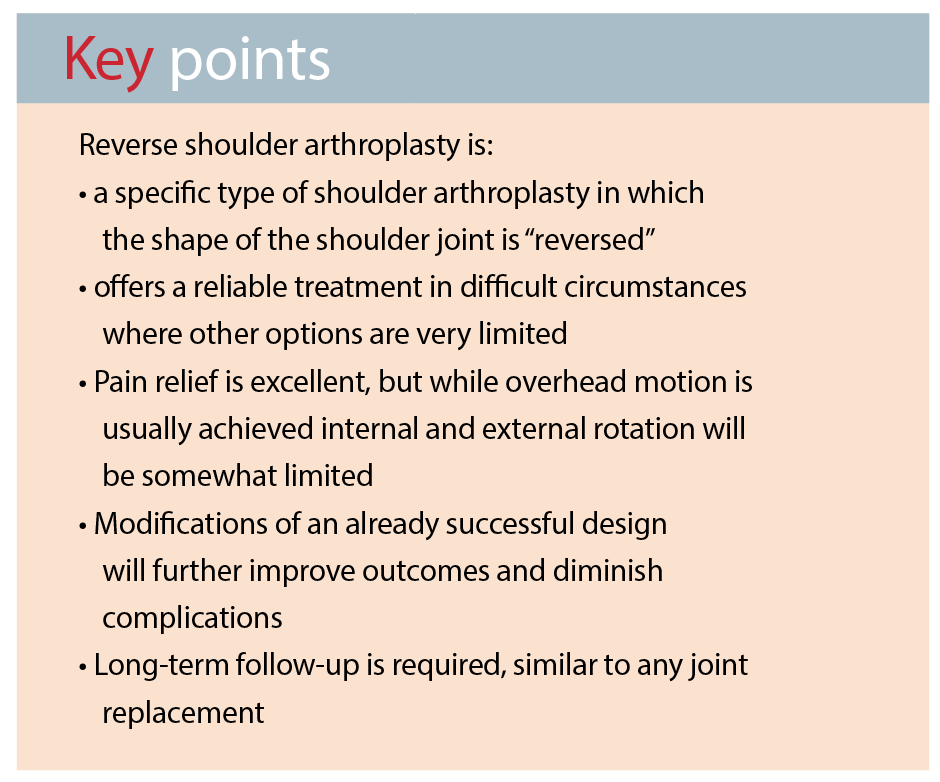
An increasing number of patients requiring shoulder joint-replacement surgery are being treated by reverse shoulder arthroplasty. Normal anatomy has the ball of the humeral head articulating with the socket of the glenoid, and an anatomical total shoulder replacement replicates this. In the reverse procedure, developed 20 years ago, the glenoid component is hemispherical and the humeral component carries the socket – reversing the normal anatomy. In the last two years, the number of reverse shoulder replacements performed has overtaken that of anatomical procedures.
Why use it?
Patients with large rotator cuff tears may develop arthritis. If a traditional shoulder replacement was used in this situation, active movement would be very limited and the glenoid component would quickly loosen.
Before the advent of reverse arthroplasty, no successful treatment option existed. The altered biomechanics after this procedure give the deltoid muscle a mechanical advantage so that it can power forward-elevation of the arm even in the absence of a functional rotator cuff. The results in terms of pain relief and range of motion are good enough that the indications have expanded to include large irreparable rotator cuff tears without arthritis, revision shoulder replacement and some proximal humeral fractures.
What are the downsides?
As with any arthroplasty, infection, instability, wear and loosening are potential complications and require surveillance for the lifetime of the prosthesis.
The most common problem specific to reverse shoulder arthroplasty is diminished internal and external rotation, which can affect the patient’s ability to perform personal hygiene and dressing. This occurs because of the deep socket of the humeral component that is required for stability in the absence of a functional rotator cuff.
Another potential problem is bone loss from the scapula (notching) that, if very severe, can cause loosening of the glenoid component. We expect that these complications will become less frequent with new design modifications. However, currently the use of this procedure should be limited to specific situations in which other treatment options are not viable.
Dr Geoffrey Smith is an orthopaedic shoulder and elbow surgeon providing services in Sydney’s North Shore, St George and the Sutherland Shire districts. He holds public posts at St George Hospital and Sutherland Hospital and is a conjoint lecturer with the University of NSW
References available on request