The toxic expectation of universal bulk billing is being chipped away, slowly.
Amid all the angst and hand-wringing we’ve done as a collective, I think (I hope) general practice is slowly on the way out of the mess we’ve created for ourselves as a collective over the last decade since patient Medicare rebates were frozen and we continued to absorb the cost.
It’s been at least 18 months, possibly longer, since we began the long and hard road, paved with many angry patients, politicians and members of the public, to charge gap fees.
Yes, our voices wavered. Yes, our hands shook. Yes, we felt guilt and continue to when we say no.
And through all of that, we have continued, in large part, to hold to our boundaries.
Some of my patients who are GPs spoke last year dispiritedly about being unable to move away from universal bulk billing, and hoped the tripled bulk-billing incentive from November would slightly boost their revenue and take-home income.
November came around, with rising costs of living – which affects all of us who are self-employed, not once but twice – and not much changed.
So, imagine my surprise earlier this week when I took a walk to drop off a letter to a local GP who’d referred a patient to me at a nearby practice. At this previously universally bulk-billing clinic there were clear signs advertising a gap fee of $30 for a standard consultation (one item per standard consultation only) and $50 for a long one. There were also fees for late cancellations and no-shows.
As I stood in the queue to hand over my letter to the referring GP, I overheard the reception staff talking to someone on the phone about an appointment and advising about the gap fee. The person must have asked her to check with the doctor about the fee, to which she replied: “It’s not the doctor’s call to make about charging the gap fee. Would you like to continue?”
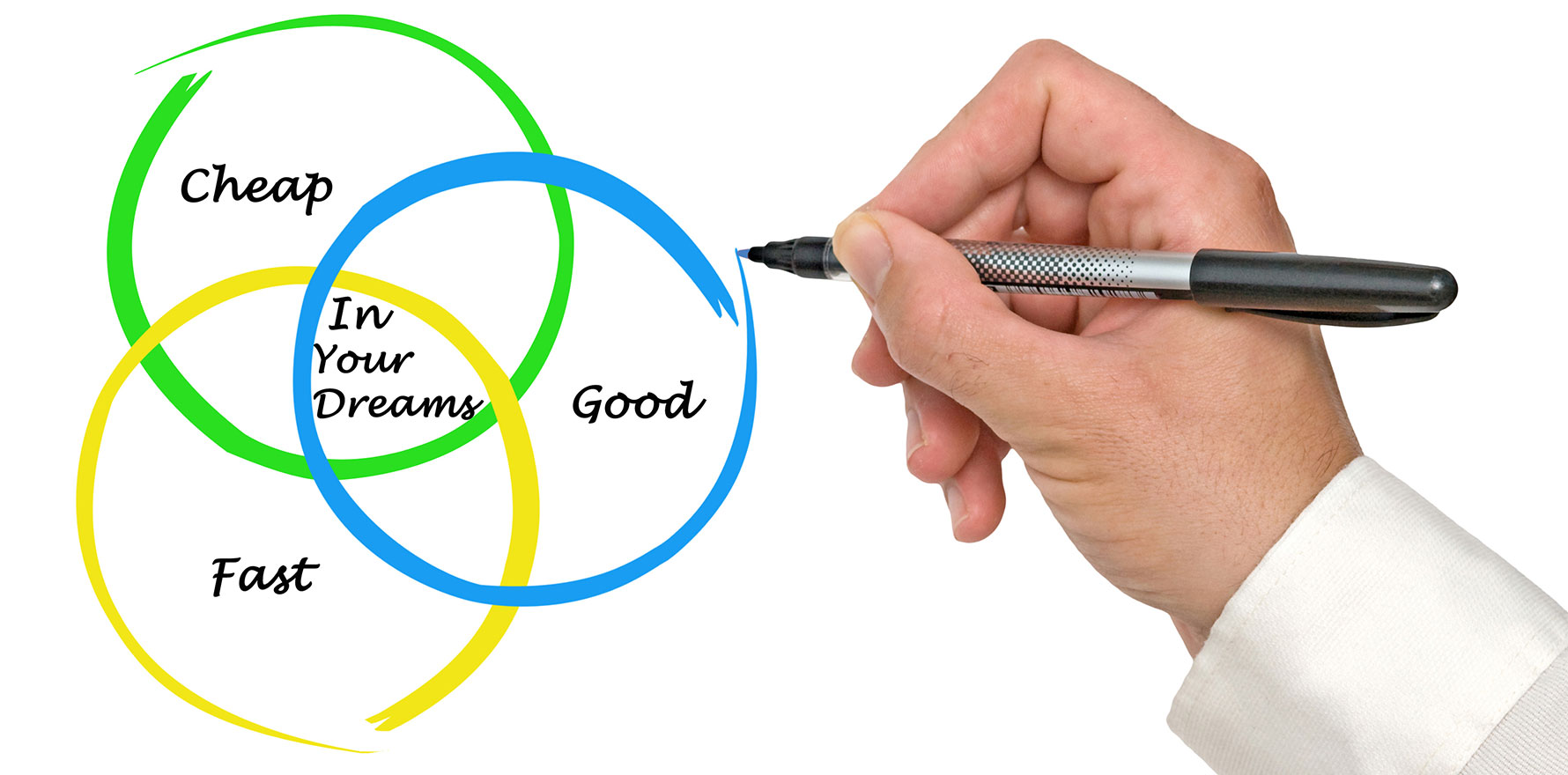
For far too long, we’ve been caught off-guard at the end of a good consultation by the dreaded sentence as a patient is walking out the door: “By the way, can you bulk bill me please?” Most of us, in this crucial moment, cave and mutter “just this once”, effectively undercutting the practice revenue by 50% and knowing we have worked for free that consultation.
Most of us complain bitterly about this yet felt powerless to do anything to change it, so witnessing this was a pleasant change. It’s not your doctor’s decision not to charge the fee any more than it is the waiter’s decision to give you a free meal at a restaurant you choose to frequent.
Related to this, many practices around me have taken to charging the entire fee upfront as a prepayment for consultations for new patients to the practice.
My own practice does this, and when we advised a patient of this recently, it was met with “Seriously?”
“Yes, seriously.”
“Why?”
“Well, this is time you reserve with the doctor and prepayment means that in the event that you cancel late or don’t show up, that time is not wasted. Would you like to continue?” Most do proceed to book and prepay and do show up.
Related
There will be those who will say it’s unfair. And then there are the practicalities of small business ownership which means that if we don’t have walk-ins and you reserve my time, it needs to be paid for regardless.
Regardless of whatever policy you choose to impose, the fact remains that we inform patients of this clearly prior to booking and paying so they don’t have grounds to say they were not informed or aware.
Prior to taking prepayment, staff used to lead with: “We are not a bulk-billing practice. Would you like to continue?” And then lead with information about fees, rebate etc.
The landscape for general practice is changing rapidly and while there is still much need and many of us continue to discount even when we know we ought not to, the fact remains that if we don’t enforce boundaries, our welfare and ultimately our businesses and ability to remain viable will suffer.
So when I feel guilty (and I still feel guilty regularly after 11 years) I remind myself: would my patients prefer I remain in business, do good work and be able to serve them, and choose to discount a small handful that genuinely need it, or see them for next to nothing and go out of business?
When I signed up, did I anticipate it would be this hard to work in medicine as a self-employed person (which was never even discussed in med school or after)? If not, is it my responsibility to educate myself so I can avoid burnout and remain viable as a small business and fulfilled as a doctor?
We all have choices. We can ask for what we need, including recognising that it is not possible to save others without also safeguarding our own health – financially, physically and mentally.
We did not sign up to be charities nor to be martyrs. We are small businesses and the best way to help the majority of our patients is to charge most of them appropriately and to choose a small handful to discount or even bulk bill because they are in genuine need.
Dr Imaan Joshi is a Sydney GP; she tweets @imaanjoshi.