While one virus is upending our way of life, others may soon be a key to survival.
When Associate Professor Peter Speck’s cousin had her foot amputated, she sadly proved the statistics right. The five-year mortality following foot amputation for diabetic foot ulcer is more than 70%.
“That’s worse than most malignancies, and my cousin unfortunately succumbed to her diabetes,” says Professor Speck, a virologist at Flinders University in South Australia. “It hits home.”
Now, Professor Speck is working on a new approach to treating diabetic foot ulcer, a complication of a disease that one in 20 Australian adults has and whose prevalence is expected to double in the next five years.
He’s turning to bacteria-eating viruses.
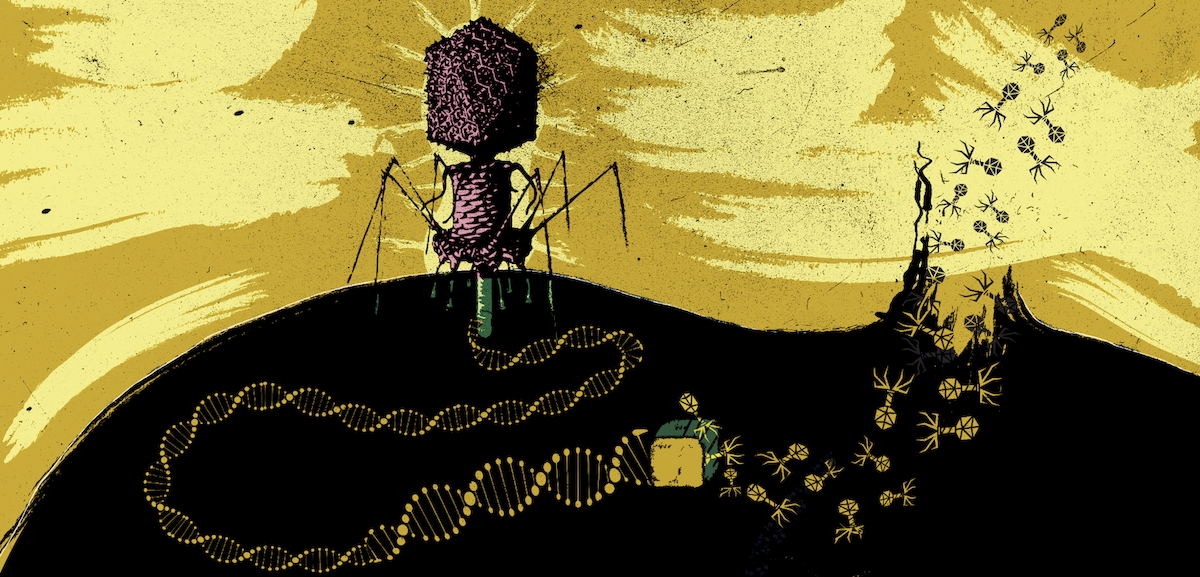
These bacteriophages, a name that literally means “bacteria devouring”, have been locked in an ancient battle with bacteria for almost as long as life has been on Earth. Each of these parasites has evolved to attack a specific type of bacteria, gaining entry and hijacking its replicating machinery to create more copies of itself. When the time is right, the baby viruses explode out of the bacterium, tearing its cell walls apart.
And Professor Speck is hoping to make a dressing with those phages on it.
Foot ulcers are one of the most common complications of diabetes, and ulcers that don’t heal invariably become infected.
One of the most common causes of infection is a species of bacteria unknowingly carried by one in three of us, in a warm and moist area like our nose, armpit or groin. And thanks to our overuse of antibiotics, golden Staph bacteria, or Staphylococcus aureus, are getting harder to treat.
To see if phages could offer a new solution, the Flinders team applied a dressing soaked in a liquid mixture of three different phages onto diabetic mice who had been wounded on the flank and infected with golden Staph. Comparison mice were treated with either saline or vancomycin, an antibiotic of last resort with nasty off-target effects on the nervous system and kidneys.
The wounds of mice treated with saline became ulcerated and full of pus and they spread. Wounds treated with either phages or antibiotics healed, but bacterial loads were significantly lower in the phage group than the antibiotic group by the end of the study, which was published in August in BMC Microbiology.
These findings are “highly likely” to be replicable in humans, given the similarity of the bug and setting of infection, says Professor Speck.
Scientists have already developed dressings bound with phages that can survive at room temperature for a year, so a version made for diabetic foot ulcer could be used in clinics and hospitals in even the most remote parts of the country.
Brought back from the dead
While this research is preliminary, phage therapy has already led to miraculous recoveries in people for whom conventional approaches have failed.
Perhaps the most well-known case is that of Tom Patterson, a professor of psychiatry who was struck down with a multidrug-resistant strain of Acinetobacter baumannii while travelling in Egypt in late 2015. The opportunistic pathogen has become so notorious among soldiers returning from Iraq and Afghanistan that it has been dubbed “Iraqibacter”, and its prevalence in hospitals around the world earned it a spot in the WHO’s most urgent antibiotic resistant threats.
Professor Patterson was eventually medevacked back to the hospital at the University of California, San Diego, where he and his wife, infectious disease epidemiologist Steffanie Strathdee, worked together as AIDS researchers.
What had started as a gallstone lodged in his bile duct, triggering pancreatitis, soon became much worse. The bacteria thriving in the abscess in his abdomen had become resistant to more than a dozen antibiotics, and it quickly became clear that Professor Patterson was dying.
Several times the superbug leaked into his bloodstream, triggering septic shock, and he lost more than 40kg over the course of the illness.
“I took his hand while he was in a coma and I asked him if he wanted to live,” Professor Strathdee tells The Medical Republic. “And if he did, to squeeze my hand.”
He managed to hear her and squeeze her hand.
That moment stands out to Professor Strathdee as one of both excitement and terror.
“I was excited that he wanted to live, but on the other hand I was terrified, because what am I going to do, right? I’m not a medical doctor. But I decided that if he was going to die, I wanted to make sure that I had left no stone unturned.”
Professor Strathdee went home that night and quickly found a paper describing alternative treatments for A. baumannii, one of which was phages.
“I knew what phages were because I had a rusty old degree in microbiology from the 1980s as a student,” she says. “I just never knew that phages are used to treat bacterial infections.”
In fact, they have been for a century.
French-Canadian microbiologist Félix d’Hérelle is credited as discovering bacteriophages in 1917, and using them to successfully treat dysentery and cholera in the following years.
Nevertheless, Alexander Fleming’s discovery of penicillin a decade later ushered in the antibiotic age. The practicality and reliability of delivering antibiotics in pills to wounded soldiers on the front line quickly drove interest up.
While phages have been used since in parts of Eastern Europe and former Soviet Union countries, they were largely discarded in the West. This was for many reasons, not least of which was the fact that Russia was an enemy after World War II, and this was considered to be Russian kind of medicine.
“Some people say that if phage was discovered after penicillin, we would probably still have been using it to this day,” says Professor Strathdee.
Although she had no luck finding a phage doctor who would treat her husband, Professor Strathdee turned to her network of friends and colleagues. Remarkably, the emails quickly began to flood in from researchers and clinicians around the world who offered their expertise.
One of the researchers who offered to help was Australian microbiologist Dr Jeremy Barr, who was completing his postdoctoral research at San Diego State University at the time. Phages started coming in from total strangers around the world who had viruses that matched the particular A. baumannii strain.
After receiving the phages, Dr Barr and his colleagues had 36 to 48 hours to clean and prepare them.
Echoing Professor Strathdee, he calls that period both “exciting and terrifying”.
“We’d never prepared a phage cocktail for use in a patient before,” says Dr Barr. The methodology was similar to their usual routine, “but the stakes were just higher”.
Cleaning the viruses is a vital step to make them ready for treatment in humans. This is because scientists often source the phages from sewage. There are an estimated million trillion trillion phages on the planet, and around 30 billion are believed to move through each of us each day, so sewage is the perfect hunting ground.
“Wherever you have a lot of bacteria, you have the perfect predator that preys on them,” says Professor Strathdee.
Cleaning is also important because phages are grown in the lab in bacteria, and when they erupt from the cell, they leave potentially toxic bacterial debris in their wake. If impurities are not filtered out, it could trigger septic shock. Professor Patterson already had had seven bouts of septic shock, and another could kill him.
“There wasn’t any room for failure,” says Dr Barr. “We worked around the clock, 24 hours a day, for two or three days to get this ready so they could be administered to Tom as fast as possible.”
The treating clinicians decided on a dose of one billion phages, which they would inject into his bloodstream. This too, was a bit of a gamble. Unlike static antibiotics, the number of phages in a patient’s body will grow and shrink depending on how well the viruses encounter bacteria, reproducing and killing them. This means that clinicians have to match phages to the specific strain of bacteria, deliver them in the correct form and make the dose high enough.
The team decided to err on the high side.
“People thought he was within hours of dying. His lungs were failing, his heart was failing and now his kidneys were failing,” recalls Professor Strathdee. “There is no question that he was going to die.”
Because the bacteria had now spread throughout his body, doctors were forced to deliver the phages intravenously and through catheters in his abdominal cavity rather than the typical topical or oral route. They also chose a cocktail of three phages, to make it harder for the bacteria to develop defences.
“There is this invisible war at a microscopic level going on between the phage and the bacteria,” says Professor Strathdee. Bacteria multiply every half hour and the phages multiply even faster.
But because these phages kill their bacterial host, the survivors of the war quickly become the bacteria who aren’t vulnerable to those phages. Luckily phages, unlike antibiotics, are ready to rapidly mutate to find new chinks in the bacteria’s shifting armour.
Within days of the phage cocktail injection, Professor Patterson woke from his months-long coma, raised his head from the pillow and kissed his daughter’s hand. Their nightmare appeared to be over.
The excitement was unfortunately short-lived, as he quickly fell deathly ill again.
The phages had been so effective at killing off the A. baumannii that a different bacteria living in his gut rapidly proliferated in Professor Patterson’s weakened body and triggered another bout of sepsis.
“The phages were actually, if anything, too effective,” explains Dr Barr. While phages can radically reduce the bacteria in a person’s body, they will never totally clear an infection. Once the predator runs out of prey, it can’t survive long either.
Instead, something else, like the patient’s immune system or antibiotics, is needed to finish the job.
A tiny arms race
Similarly, clinicians have to be ready with back-up phages in case the bacteria evolves resistance. In Professor Patterson’s case, his A. baumannii adapted within weeks, requiring new phage cocktails over the following six weeks of treatment.
This relentless arms race has a remarkable benefit for us though, explains Professor Strathdee. It can revive defunct antibiotics.
“When bacteria is being attacked by an antibiotic and phage at the same time, metaphorically speaking, the bacteria is going to make a genetic decision as to what mutation is going to allow it to live.”
In her husband’s case, the superbug dropped the capsule the phages use to attack them. This capsule was the physical barrier that protects the bacteria from antibiotics, making them vulnerable to antibiotic treatment again.
“Some failing antibiotic regimens that have been sitting on the shelves, not working any more because of multidrug resistance, could be resurrected by phage,” she says.
It was this combination that finally enabled Professor Patterson to kick the infection, eventually leaving hospital and returning to work. His case was a watershed moment for medical phage research.
Compassionate usage cases have dramatically increased around the globe and experts working in the field say it has prompted a flurry of activity.
Since then, the Center for Innovative Phage Applications and Therapeutics at UC San Diego, established by the husband-and-wife team, has treated 14 patients with phage therapy and consulted on dozens of others in the US and abroad.
But the pressure is now on clinicians and researchers to back up these exciting anecdotal findings with more rigorous clinical trials. Only then will phages be ready to take their place among packets of antibiotics at your local pharmacy.
“In Australia, we’ve probably treated around 18 people,” says infectious diseases physician Professor Jon Iredell. This kind of compassionate access is welcome to treat patients when nothing else is working, but “it doesn’t really advance our knowledge significantly,” says the University of Sydney clinical microbiologist.
In this quest to establish good evidence, Professor Iredell and his colleagues published a paper in Nature Microbiology earlier this year, showing phage therapy could be safely administered intravenously to patients with severe Staphylococcus aureus infections in the blood.
These 13 Westmead Hospital patients were given both a cocktail of three phages and antibiotics over two weeks, and no adverse reactions were found.
He is careful not to trumpet this approach before we can thoroughly answer fundamental questions around safety, efficacy and dosing. “It’s my job to be the sceptic,” he says, cautious that phages have at times been treated with a cavalier, alternative medicine approach.
“People turn to things like this in desperation.”
And while Professor Iredell believes phages should be part of mainstream medicine, with all the scrutiny that entails, previous clinical trials have been surprisingly disappointing. Some blame this on methodological problems such as underdosing and treating with the wrong phage for the type or strain of bacteria. Many believe that personalising phage treatment will be more successful.
It is both an advantage and disadvantage that phages typically only attack some of a single species of bacteria, sometimes only strains. This makes them safer in many ways than antibiotics, because they are a trained assassin homing in on one target, compared with the carpet bomb approach of antibiotics.
Scaling up
But for phage therapy to truly make a difference, we won’t be able to wait days while labs identify, purify and ship out bespoke phages for each individual case. The most popular idea is to develop a nationwide or global phage library for the most common and highest priority pathogens.
“We could start with a pathogen of interest, understand the phage biology, isolate a phage-resistant mutant, and then we could already pre-select phages that can kill that phage-resistant mutant,” says Dr Barr.
This way, clinicians could know that this pre-prepared phage cocktail would be active against up to 90% of those isolates, and begin treating the patient immediately. Then researchers such as Dr Barr could begin optimising the cocktail for that specific pathogen.
Unfortunately, this approach still requires an enormous investment of time and resources, and the field remains “severely” underfunded, says Dr Barr. He believes time is running out to develop the workforce and knowledge needed to meet the existential threat of antibiotic resistance.
Right now, more than 700,000 people die each year due to drug-resistant diseases, and WHO estimates that figure to rise to 10 million by 2050. That is one person every three seconds.
This is where phages are a crucial weapon, says Professor Strathdee.
“Fewer and fewer antibiotics are being developed by pharmaceutical companies because their shelf life is so short because of resistance, and they are being told by agencies like the World Health Organisation that any new antibiotics have to be kept in reserve,” she says.
“The pharmas have a disincentive to get into the field.”
Meanwhile, her clinic is increasingly fielding calls from COVID-19 survivors who have developed secondary infections while sick and in treatment.
“We are going to be facing a world very soon where simple elective surgeries won’t be possible because the risk of antibiotic-resistant infections is too high.”
Professor Speck is frustrated that governments don’t seem to grasp the nature and magnitude of the threat of infectious diseases, all while spending eye-watering amounts on military budgets.
“Even in this coronavirus era, they still don’t get it.”
An earlier version of the story misstated that Russia was an enemy during WWII.