Time, patience and compassion are critical when faced with this difficult clinical issue
How do you feel when a patient reveals they have suicidal or self-harm thoughts, plans, or intent? Anxiety would be a common and understandable reaction.
Mental health-related presentations make up about 13% of GP presentations,1 a figure that is rising and with it this index expression of psychological distress. This article outlines an approach to assessing and managing patients who present with suicidal or self harming ideation that hopefully will increase GP confidence in dealing with this important clinical problem.
Terminology
Suicidal or self-harming ideas may signify a host of different intents and outcomes. Some definitions might be helpful:
Suicide – a fatal act of self injury with evidence of intent to die
Active suicidal ideation – thoughts or plans about taking action to end one’s life, which may or may not include a specific method, with an intent to die
Passive suicidal ideation – thoughts about wanting to die without a current or active plan or intent
Deliberate self harm – self injurious behaviour which may (suicide attempt) or may not (non-suicidal self injury) have suicidal intent. Non-suicidal self injury may serve multiple functions, including distress tolerance, stress relief, countering emotional blunting, or may herald future self harm with suicidal intent.
It is important, therefore, to attempt to understand the patient’s ideation or actions in context of these categories as this will guide an appropriate form of intervention.
Time, patience and compassion
Suicidal and self-harming ideas and behaviours are a complex phenomenon that is usually a product of several factors at play, and adequate assessment takes time, patience and compassion.
While this approach can be challenging to maintain in busy general practice that is rewarded for shorter consultations rather than long ones, it will ultimately lead to better access to a patient’s inner psychological world, which in turn will produce a more accurate risk assessment and better management decisions and clinical outcomes for the patient and the clinician.
The overwhelming evidence is that traditional tools of risk assessment, such as rating scales or questionnaires, are extremely unreliable in predicting future suicide and self harm.2
However, rating scales may be useful in cataloguing the presence of symptoms of mental illness which might lead a clinician to be more concerned about risk. But just simply asking a patient whether they are suicidal or not is unlikely to result in a truthful disclosure. A small qualitative study suggested that up to a quarter of patients who had attempted suicide did not disclose intent when last asked and some suggested that a fear of stigma or adverse reaction from the questioner contributed to this.3
Indeed, reasons for not wanting to discuss psychological issues in general practice include poor interview behaviours, a perceived lack of time from the GP and a sense there is little a GP can do to help.4
Adequate psychiatric risk assessment first necessitates the removal of these barriers by generating a sense of time, patience and compassion, but in a focused and well-informed manner.
Risk factors for suicide
While it may not be possible to shoehorn a patient into “high, medium or low” risk based purely on a list of risk factors, being aware of epidemiologically based risk factors might help in informing an appropriate level of concern.
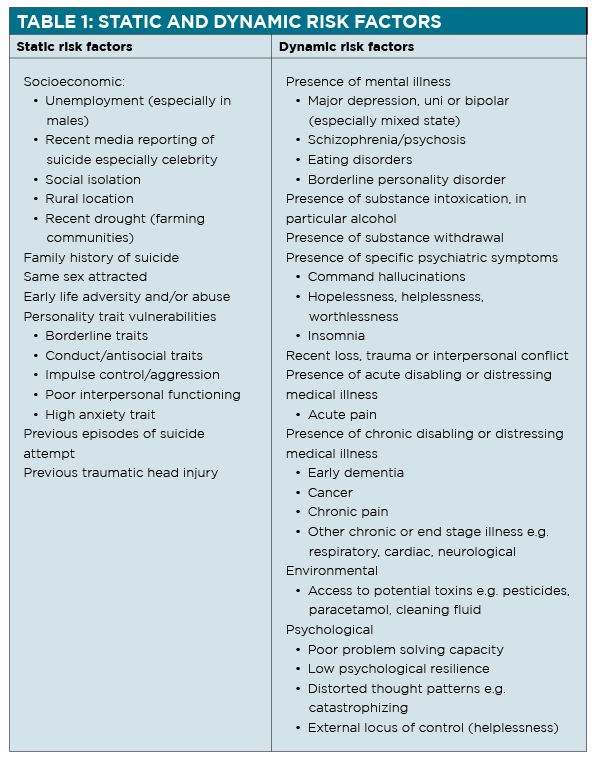
Risk factors can be helpfully divided into two broad categories: “static” and “dynamic”.
Static risk factors are unchangeable characteristics of the patient themselves that increase or decrease their statistical level of risk. Examples of static risk factors include a patient’s demographics, family history et cetera.
Dynamic risk factors are changeable characteristics of a patient’s clinical state which affect the patient’s level of risk based on their presence, absence, or severity. Examples of dynamic risk factors include the presence of substance intoxication, certain psychiatric symptoms such as command hallucinations, the absence of sleep (insomnia), or the severity of major depressive illness.
Table 1 on page 28 lists static and dynamic risk factors to consider.5
Suicidal ideation rarely occurs in isolation but usually in the context of a range of these risk factors, most commonly concurrent mental illness. Suicidal ideation is but one, albeit important, marker of psychological distress and when one addresses the patient’s overall condition in a holistic biopsychosocial/cultural framework, suicidal ideation is also often ameliorated. Focusing purely on the suicidal ideation alone is rarely helpful.
It is worth noting that suicidal ideation is relatively common in the community with a lifetime prevalence of 13.3% but only 4% having a suicide plan, and 3.3% making an attempt.6 Only 0.01% completed suicide in 2016.7
The conclusion is that while thoroughly assessing and making a management plan is important in every case of reported suicidal ideation, one must also accept a certain level of risk as long as a patient is willing to engage in ongoing treatment, monitoring and engagement.
At the point where as a clinician this fails, a referral to a more specialised or assertive service is applicable.
First things first: the psychiatric interview
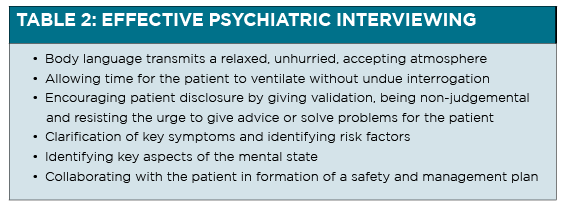
As mentioned previously, much of a clinician’s success in managing an at-risk patient depends on their ability to engage the patient in a therapeutic alliance, a process that requires time, patience and compassion. Once a good therapeutic alliance is formed, the clinician can illicit the concurrent risk factors that may or may not be able to be modified to lower the level of psychological distress and risk.
Effective interviewing is crucial to establishing good therapeutic alliance (See table 2, above).
The goal of the psychiatric interview is to determine a diagnostic formulation, or understanding of the patient’s distress from a biopsychosocial perspective. From there, a management plan addressing these issues can be produced.
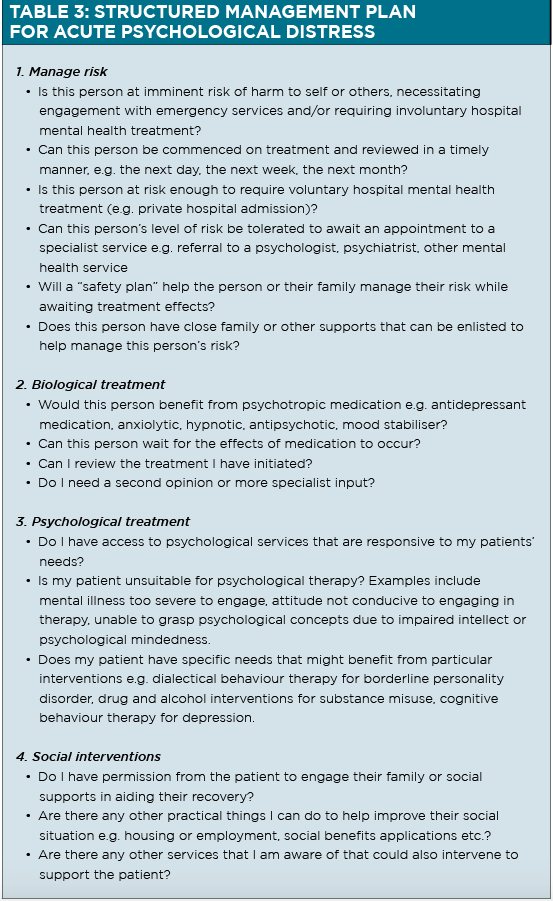
Structuring a management plan
A structured management plan for a patient presenting in acute psychological distress or with suicidal/self-harming ideation is presented in table 3 above.
Safety plans: how useful are they?
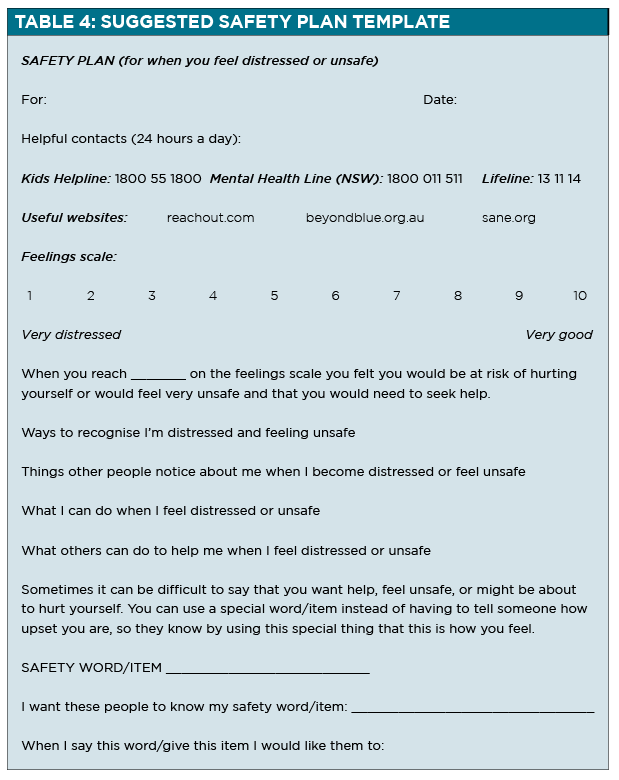
As mentioned previously, focusing purely on a patient’s suicidality and risk without a holistic approach is rarely helpful. However, a safety plan giving a patient a contingency in a period of crisis might be helpful.
As always, a safety plan should be completed in a collaborative manner and should not be relied upon as the sole intervention to manage a patient’s risk of suicide. Discussing a safety plan in isolation may communicate a lack of understanding or interest in what the patient feels is the most important problem they have, which is often not their suicidal ideation.
Table 4 above shows a suggested structure for a safety plan.
Conclusion
General practitioners are uniquely placed to make significant contributions to the mental health of their patients. They are often trusted physicians with a long and wonderful relationship with not only a patient but their families.
With a focus on time, patience and compassion in the consultation room, a general practitioner can be a highly competent health professional in managing not only suicidal ideation and risk, but mental ill health in general.
Dr Terry Lim is consultant psychiatrist at the Hills Clinic Private Hospital in Sydney. He is interested in managing a wide range of conditions including adult ADHD, psychosis, mood and anxiety disorders and has a special interest in managing clients with co-existing mental and physical illness. He is also a clinical lecturer of the University of Sydney.
References:
1. Mental Health Council of Australia. Not for service: Experiences of injustice and despair in mental health care in Australia. Canberra: Mental Health Council of Australia, 2011.
2. Carter G, Milner A, McGill K, Pirkis J. Predicting suicidal behaviours using clinical instruments: Systematic review and meta-analysis of positive predictive values for risk scales. B J Psych 210 (6); 2017: 387-395
3.Richards JE et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: A qualitative study. Psychiatr Serv 2018 Nov 20
4. Cape J, McCulloch Y. Patients’ reasons for not presenting emotional problems in general practice consultations. Br J Gen Pract 1999;49(448):875–79.
5. Turecki G, Brent DA. Suicide and suicidal behaviour. The Lancet 387 (10024); 2016: 1227-1239
6. https://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-m-mhaust2-toc~mental-pubs-m-mhaust2-hig~mental-pubs-m-mhaust2-hig-sui
7. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by+Subject/3303.0~2016~Main+Features~Intentional+self-harm:+key+characteristics~7