Doctors do not endure years of training and sacrifice just to be strangulated by non-clinical tasks, writes Dr Eric Levi
Where we are today in health care is the product of our contemporary society. The drive to modernisation and industrialisation is palpable. Clinicians after clinicians have detailed the despondency, despair and desperation they feel when their clinical work is suffocated by bureaucratic burdens from Health Administrators. Read the comments from Episode 1: The Dark Side of Doctoring. This is not only for doctors and not limited to Australia alone.
It does not have to be this way. You did not go into years of training and sacrifice just to be strangulated by non-clinical tasks, programs, guidelines & protocols. We have sadly seen many colleagues who succumbed to the pressure by becoming hardened, calloused, depressed, angry, anxious, irritable, rude, disrespectful, short-fused, disillusioned and even suicidal. It does not have to be this way. For the sake of our patients and future generation of doctors, nurses and health care workers, we can shift the focus back on to the patient.
There is an elephant in the room. The elephant in my operating theatre is different to the elephant in your ward or the clinic. For some, it is a clunky Electronic Health Record software. If you have to keep on correcting and teaching a whole hospital full of well-educated doctors and nurses how to use the computer, then there’s something not user friendly with the computer. For another, it is the multi-layered paperwork process that hold back good treatments for patients. For yet another it is the unspeakable culture of bullying and harassment. It is not a single problem with an easy solution.
This is not specifically about mental health issues. Caring for the mental health of clinicians is critical and essential. If you do have mental health conditions, please be connected to your GP or mental health professional. There’s an army of mental health supporters available. But many health care workers do not have mental health problems. This is about the workplace environment of the Health Industry that can create, exacerbate or prolong mental health problems. This is about the many of us who sense that Loss of Control, Loss of Support and Loss of Meaning in our daily work experience. That sense of hopelessness and helplessness in the Health Industry may not be fixable with more cognitive behavioural therapy or more anti-depressants in some situations. And it’s certainly not fixable with more guidelines, systems or processes.
May I suggest 3 small things we can change? They’re paradigm shifts that I hope will help guide your thoughts and spark conversations in your wards, clinics and operating theatres.
1. Change your Hierarchy
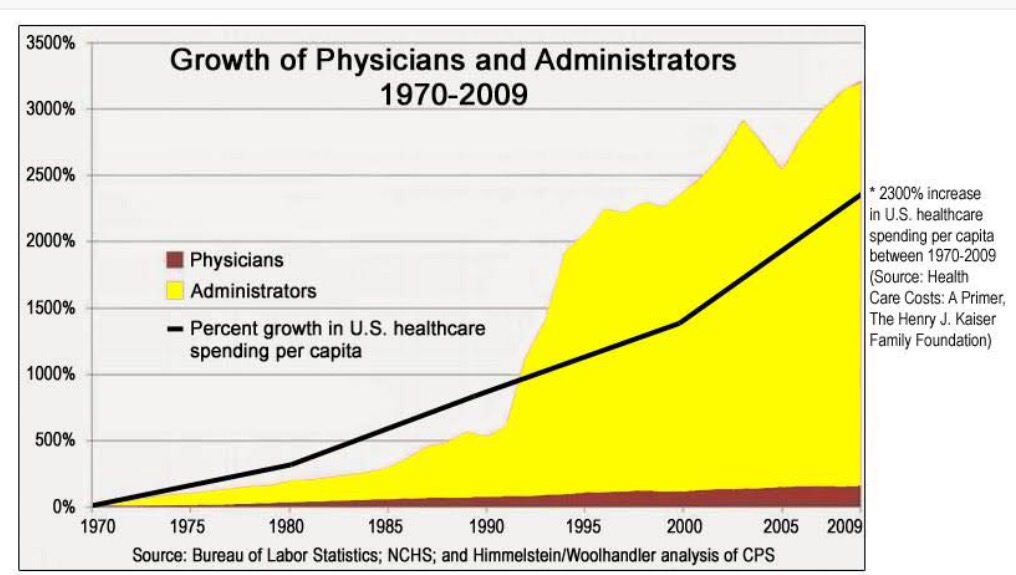
The possible antidote to Loss of Control. It’s no secret that there is an epidemic of Health Administrators. The following graph has been criticised as having poor accuracy, but the message is still the same, and the picture is clear. This graph is reproducible in any country. Is this justified? Is the elephant in the room the Middle Managers? Is this contributing to the deep sense of Loss of Control that many doctors and nurses experience?
Let me be clear. We need Medical Administrators. We need someone to Administer Health Care in a complex industry. However, we need evidence and justification that their presence in the hospital add efficiency and efficacy rather than simply adding bureaucratic complexity and complacency. Over time, the control of health care has been taken away from the blood-stained hands of clinicians and placed into the cufflinked hands of men and women in suits. We started off by employing Administrators to make our health care provision more efficient so we can be released to perform our clinical duties better. Yet we’ve ended up with a model that says Executives at the top, doctors and nurses at the bottom. And somehow we still end up carrying the burden of paperwork.
Who is at the top of your hierarchy? It should not be a CEO. It should be the patient. The CEO should be at the bottom. He or she should be the one facilitating, empowering and encouraging the work of everyone else in the hospital, not dictating it.
Dear Medical Administrators: I don’t work for you and you don’t work for me. We both work for the patient together.
Patients did not come to the hospital to see a Medical Administrator. They came to see a clinician. A doctor, nurse, speech pathologist, dietitian, audiologist, physiotherapist, etc. Strip off your hierarchy and understand that the most significant encounter that the patient came for is that face-to-face encounter with their clinician. The entire hospital exist for that encounter. Therefore make that encounter the focus of the system. Don’t add unnecessary layers of bureaucratic or systemic restrictions. The goal of hospital administrators should be to facilitate and empower doctors to be doctors and nurses to be nurses. Whenever a new computer program, a new process, or a new system is introduced to the hospital, clinicians need to be able to ask “Is this good for the patient?” If it isn’t, then it has to go back to the drawing board. If clinicians are bogged down and distracted by relentless paperwork, clunky medical software, and unrealistic key performance indicators, they can’t do their jobs properly. They won’t be playing their best game. Their morale suffers, the hospital suffers and ultimately, patients suffer.
It’s a mental shift for the doctors too. Doctors used to be the priests of ancient times. Whatever doctors said got done. We just can’t do that any more. Health and health care is way too complicated for any doctor to do it alone. I’m glad it is so. No longer is the doctor the repository of knowledge. We now work in teams. I’m no more important than the other specialty. Nurses are not my handmaidens. Nurses don’t serve the patient before or behind me. They serve beside me. Nurses, you are not the guardians that stop doctors from killing patients. You are fellow specialists with distinct and complementary roles. Even though sometimes the Doctor ends up being captain of the ship, a good captain will allow every crew member to function at their best.
In my simple surgical mind the hierarchy is basic. Patients at the centre, clinicians around them, and health administrators as the facilitators of service, empowering the clinicians to do their work unhindered. Strip away any unnecessary processes that interfere with the Clinician-Patient encounter. The CEO, Nurse, Janitor, Kitchen Staff, and Admin all need to know that they came to work for the patient.
2. Change your Habit and Habitat
The antidote to Loss of Support. When we talk about Loss of Support, often the answer is official support programs and help lines. Every Institution, Professional College and Hospital have dedicated help lines for staff and members. Although they are necessary, very few actually tap into those services. I struggle with the practicality of calling an anonymous helpline and speaking to them about the emotional struggles I have with Electronic Medical Records or overbooked clinics. I want to talk to the people at my workplaces because they are the ones who understand my struggles. But who do I talk to? Everyone seem overworked, preoccupied and distracted at the same time. And it seems that for many, the solution to the workplace problem is a holiday. That’s like walking out of the room to the beach and then coming back to find that the elephant is still there.
Can we look at our workplaces and think about simple creative things to make our work more enjoyable and meaningful? Can we agree that we all want to come to work to enjoy caring for patients?
The greatest asset of a hospital is not her location, reputation or state of the art equipment. The greatest asset of a hospital is her staff. If a hospital treats their staff well, the staff will treat their patients well and their patients will treat the hospital reputation well. Investing in the well being and morale of staff members will reap long term results.
Improving staff morale has to happen at multiple levels. There has to be roster regulations to prevent dangerous overworked doctors. There has to be limits to daily activities. You cannot increase productivity at the expense of sanity. You won’t fly an overcrowded plane, why do we allow an overcrowded operating list run by people who do not know the procedures. It’s dangerous.
At a more practical level, investing in staff does not have to be expensive or prescriptive. What about tweaking little activities and changing their Habits. Start shifts 15min early with coffee. Do a work stop “10 min at 10” and get all the nurses in the tea room to chat. Celebrate birthdays. Go out for drinks. I used to work in a hospital where we would go for coffee after Multidisciplinary Tumour Board Meetings. We looked forward to the Group Caffeine Therapy. Monthly journal clubs with meals together. Have a reward system. Have a formal Thank you board. Instead of recording Risk Incidents, how about recording Good Incidents. Do FitBit challenges together. Set up Facebook and Twitter groups for private chats. A few years ago I wrote my own personal challenge “30 Days to Better Doctoring” and there may be a few other ideas there. Better still, why don’t you set up a white board in the staff room and let your staff make suggestions on simple activities at work that can improve morale. You don’t have to be a Head of Unit to do this. You can change the Habit of your team over time.
To measure the pulse of a hospital, don’t go to the Boardroom. Go to the staff cafeteria. I dare every hospital administrator to take off their suits and put on scrubs. Walk into staff tea rooms anonymously, sit and listen to the conversations.
Sometimes, changing the Habit require changing the Habitat. Does your hospital have a quiet room where the CEO and the Janitor can sit quietly on the sofa? Does your hospital have a play room where the secretary can sit on the bean bag watching TV next to the radiographer? There are studies to show that workplace environment influence workplace productivities. Make hospitals hospitable. Having hot foods, snacks and crackers would lift staff morale and trigger opportunities for conversations much more than signing them up for more wellness programs or getting them to watch more self-care videos. And good coffee. Please, we all know that good coffee is the lifeline of all hospital staff.
We are simply overworked humans in a complex health care industry. We need practical support that can come with a good friendly chat over coffee. We care for sick patients. Allow us the Habit and the Habitat to care for each other.
3. Change your Heart
I know. Why should a surgeon talk about touchy-feely heart stuff. I am a champion whinger. If there is ever a competition on whinging and whining, I would be world number 1. Whinging and whining is cathartic and therapeutic. We all do that sometimes. But in the midst of that whining about workplace problems, I need to remind myself that I am caring for some truly unfortunate patients who have been plagued with diseases. I have operated on kids in their first day of life and on adults in their dying days. I have said goodbyes to patients and been invited to their funerals. I have had letters of thanks.
I am grateful that I have been given the awesome privilege of being a surgeon. I’m not removing tonsils, I am giving this child and her family the gift of sleep. When I’m reconstructing a face that has been disfigured by cancer, I am giving my patients a tangible hope that life would be better after the operation. When I operate on the ear, the tongue or the voice box, I am returning to my patients some of the most basic senses of being a human.
The road to being a surgeon is tortuous and torturous. Being deprived of basic human needs such as sleep, social contact and a routine is torture. But I chose it. I chose this path. I expect to be trained hard and to work hard. My years of training mean that I can wake up at 3 am and save an exsanguinating patient if I had to. Resilience is built into the training. When the mindless administrative bureaucratic elephants sit on my chest, I need to remind myself that I’m here for the patient. When I’m close to the edge of bureaucratic burnout I need to be thankful for this crazy job I have.
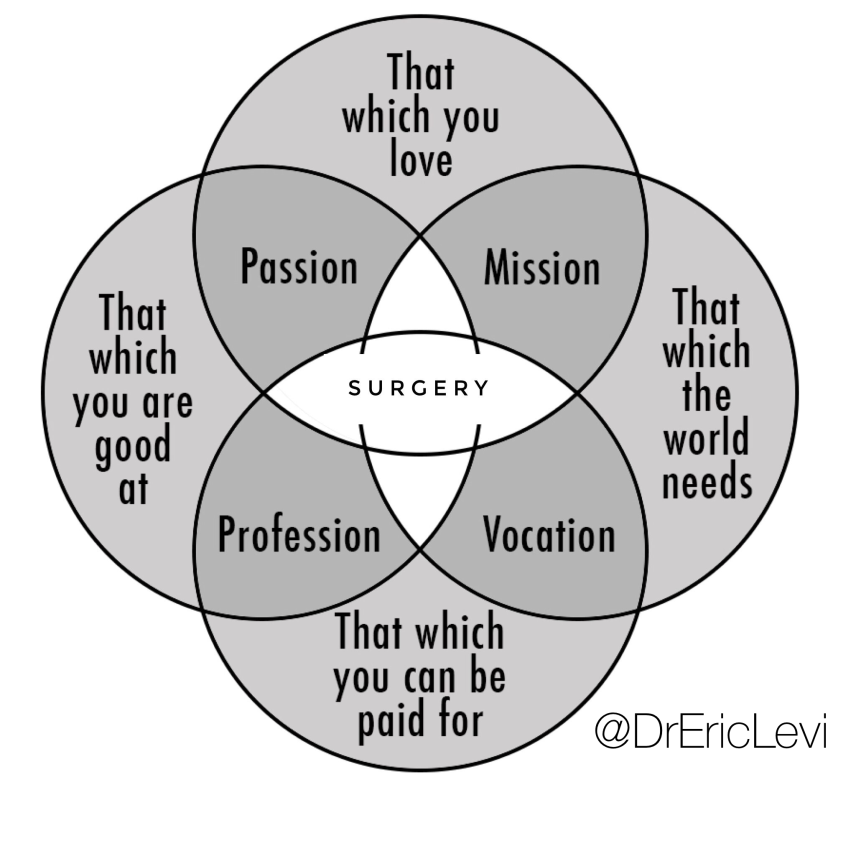
Perhaps the antidote to a Loss of Meaning is an attitude of gratitude. You can call it what you like. A sense of purpose, a calling, a vocation. You can link this to something bigger than yourself. I know where I stand when it comes to that. As a Health Care Worker I dispense hope and care to the ill patients I see everyday, together with my colleagues. Sometimes that care comes in the form of medicine or surgery, other times that care comes in the form of my words. Every day my words and actions have an influence on others. And that’s something I am thankful for. Here is how my Ikigai look like. Yours may be different.
Perhaps the secret to an attitude of gratitude, the antidote to the Loss of Meaning is loving what you do more than doing what you love.
To the many Medical Students and Junior Doctors who have asked me, the answer is this:
Yes, I cannot think of being anything else but a surgeon.
Yes, it has been a worthwhile sacrifice.
Yes, I would do it all over again.
Dr Eric Levi is an Australian otolaryngologist, ear & nose & throat, head & neck surgeon. This blog was originally published on Dr Levi’s blog.