Longer scripts to cut pharmacy fees, government-funded tests and more bulk-billed non-GP services would be a start.
Nearly every Australian uses some part of the health system every year, whether it be going to the GP, getting a prescription filled, or seeing a specialist.
Despite having a universal health-care system, we often still pay for these services out of our own pockets.
Sadly, these out-of-pocket payments are unaffordable for many Australians – so they skip the trip to the doctor, or defer going to the chemist.
This is bad for those individuals, but also bad for taxpayers and the economy. It makes people sicker, widens inequities, and puts further strain on the health system down the track.
In the Grattan Institute’s latest report, we identify what governments should do to make health care more affordable for more Australians.
Who is missing health care because of cost?
In 2020-21, more than half a million people deferred or did not fill a prescription because of cost. Nearly half a million decided not to see a specialist because of cost.
People with chronic conditions have much higher health-care costs, particularly if they have multiple chronic conditions; they spend between A$200-600 on average on health care each year.
But they are also less likely to be able to afford their ongoing care because their chronic condition can make it more difficult to keep or get a job.
Many of these people who are forgoing health care due to cost are younger, particularly younger women:
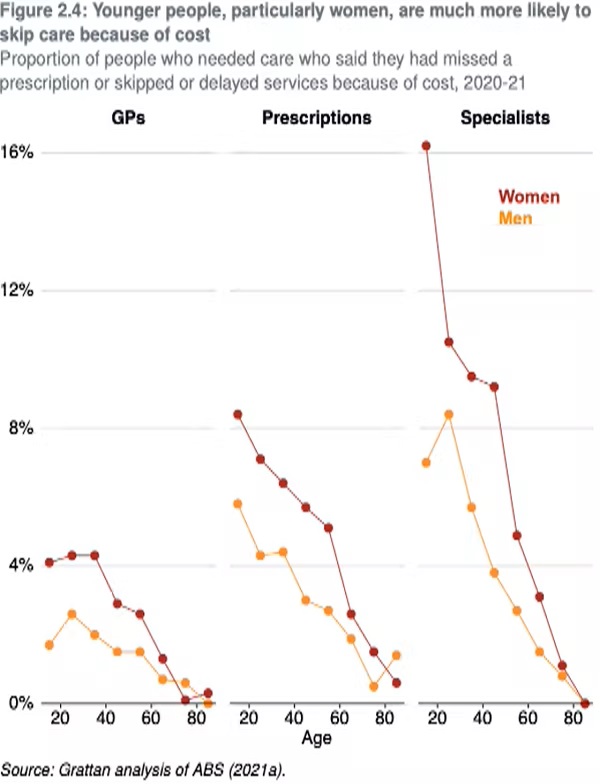
Younger people tend to have fewer savings, and can therefore find it harder to afford care. And women are more likely to have chronic health conditions. About 55% of people with two chronic conditions are women, and 60% of people with three or more chronic conditions are women.
Chronic conditions are becoming more common, so more and more Australians will be facing higher health-care costs and are at risk of missing needed care.
Over the past ten years, average out-of-pocket payments rose by 50%, and they will continue to rise unless governments act now.

What can be done?
The federal government can do much more to reduce out-of-pocket payments and avoid unnecessary costs down the line.
Cost of medicines
While Australia has a world-renowned Pharmaceutical Benefits Scheme (PBS) that helps keep many medications affordable, Australians are still spending nearly A$3 billion on PBS-listed prescriptions each year, including A$1.5 billion on mandatory co-payments and A$1.4 billion on PBS-listed prescriptions which cost less than the co-payment.
The federal government should lower the cost of prescriptions for people taking five or more medications for chronic conditions, after their GP conducts a medication review triggered by a computer-generated alert.
We estimate this could reduce inappropriate medication use for about 300,000 patients.
The government should also extend the duration of prescriptions for some medications to reduce the number of Pharmaceutical Benefits Scheme co-payments people have to make to pharmacies.
Tests and scans
The government should abolish the out-of-pocket burden from diagnostic services, such as blood tests and scans.
Australians spend about A$400 million on these services each year – even though patients aren’t the real users of these tests, doctors are.
With these services now frequently provided by large corporations, the federal government should fund them directly through a commercial tender instead.
Patient enrolment
The government should expand the voluntary patient enrolment scheme to people with two or more chronic conditions.
Patient enrolment is where a patient can enrol in a GP practice and nominate a GP to be their “usual doctor”. It can help make care more affordable for people with chronic conditions by reducing their exposure to out-of-pocket payments.
Greater GP stewardship over a person’s care could reduce inefficiencies in areas such as routine repeat prescriptions and routine renewal of specialist referrals.
The government has already committed to this reform for people older than 70. If it was expanded to younger people, we estimate an additional 1.7 million people would be eligible for the program.
Bulk billing
The vast majority of health services people receive outside hospital are “bulk-billed” – meaning the patient pays nothing out of pocket. But bulk-billing rates for specialists and allied health are still far too low – at about 46% for specialists and 56% for allied health.
The federal and state governments should expand the number of health-care services provided free of charge, particularly in lower-income areas and areas where bulk-billing rates are especially low.
Our analysis shows that if state and federal governments invest an additional A$710 million a year on these reforms, they could save Australians about A$1 billion in out-of-pockets a year, and enable more people to get the care they need, when they need it. That’s a healthy return on investment.
Professor Stephen Duckett is director of the health and aged care program at the Grattan Institute.
This article is republished from The Conversation under a Creative Commons license. Read the original article.


