Hydralyte, formulated to meet WHO ORS recommendations, has the correct balance of fluid, glucose and electrolytes to allow rapid rehydration while helping restore electrolyte balance
Recognising and managing dehydration with HydralyteTM
Choosing the appropriate oral rehydration solution (ORS) is an important first step in managing mild to moderate dehydration1-3 — Hydralyte, formulated to meet World Health Organisation (WHO) ORS recommendations, has the correct balance of fluid, glucose and electrolytes to allow rapid rehydration while helping restore electrolyte balance.1,4
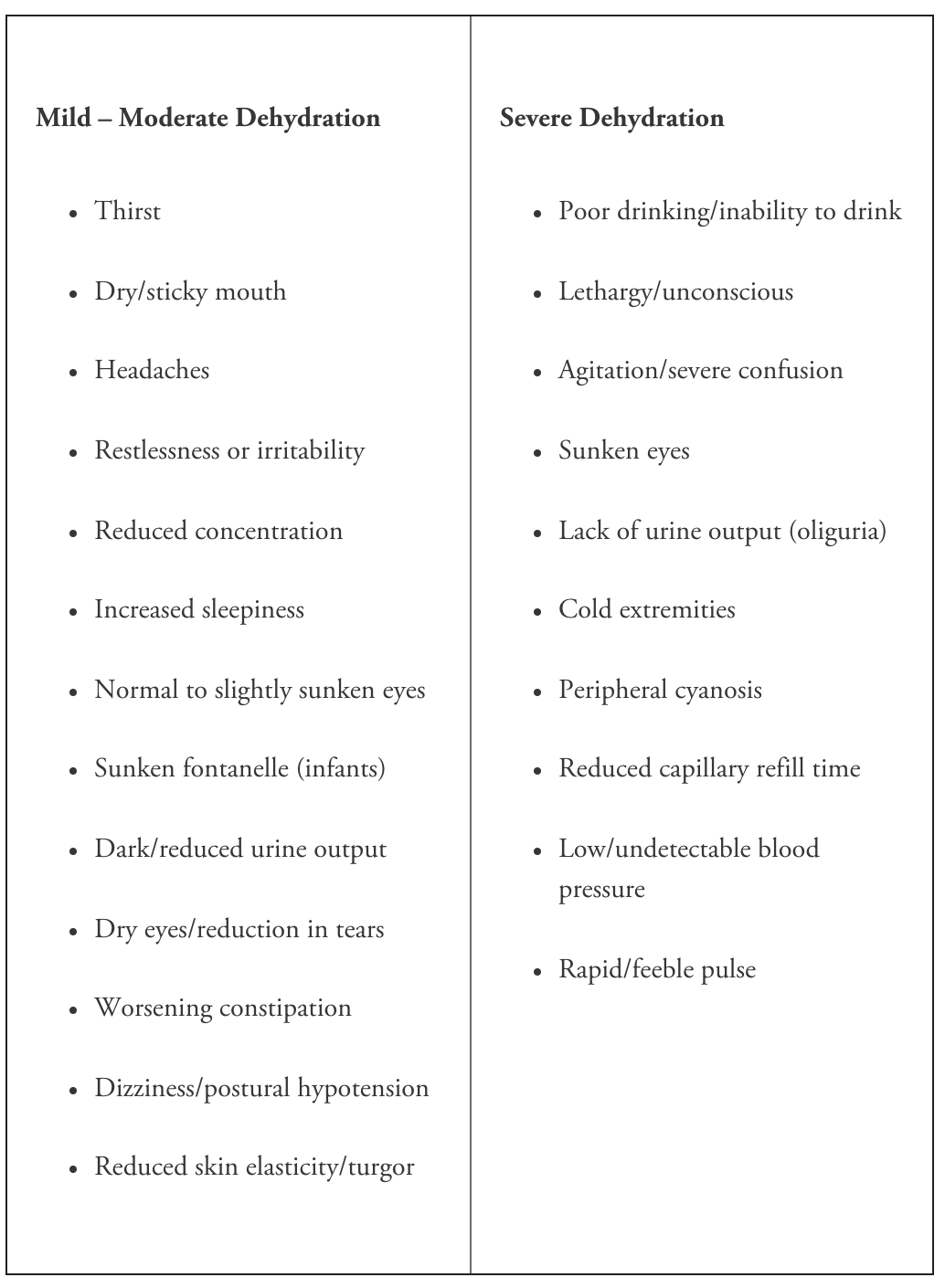
Recognising the signs of dehydration is important
Healthcare professionals (HCPs) play an important role in both recognising and mitigating the potential effects of dehydration — managing the spectrum of mild to the most severe, life-threatening cases.5
Being able to recognise the signs of dehydration is important to the patient too. The HCP also plays a crucial role in being able to predict who is potentially most at risk and educating these patients about signs to watch for, how they can manage dehydration themselves and when to seek help.5
Most healthy individuals, under normal conditions, can drink adequate amounts of fluid to maintain their body water balance — but fluid losses can easily outpace oral intakes due to ‘everyday’ causes such as excessive sweating, vomiting and diarrhoea.6 Thirst cannot always be relied on as an indicator of dehydration, particularly in older people, with dehydration resulting from both physiological and disease processes.3,6,7
Early detection is important as dehydration can progress rapidly — if oral rehydration is not addressed symptoms can quickly worsen.3,7-9
Oral rehydration therapy, using an ORS such as Hydralyte, is a simple, proven intervention that helps rehydrate patients with mild or moderate dehydration symptoms faster than water alone.1,22
Detecting dehydration
Various simple clinical signs and symptoms are often used to screen for dehydration (Box 1).3,10 However, dehydration can be difficult to diagnose as many of the ‘typical’ indicators are not reliable, can be associated with other diseases, medications or vary with age.3,11
The more useful clinical signs of dehydration include:
- Reduced axillary sweating, reduced skin turgor, dry oral mucosa, recent changes in consciousness and darker urine in older adults3
- Capillary refill time, skin turgor and respiratory pattern in children (1 month to 5 years)2
- WHO recommends four clinical signs (general condition, appearance of eyes, thirst, and skin pinch reactions) for the assessment of dehydration in both children and adults.10
While these indicators may be characteristic of dehydration, most are subjective and no one sign or symptom is thought to be sufficiently predictive of hydration status — a combination of physiological (Box 1) and biochemical measures (Box 2) along with patient history being needed to more accurately diagnose the severity of dehydration.2,9,11
Simple clinical signs and symptoms are, nevertheless, useful in aiding the initial diagnosis and prompting further investigation or action.11 Physiological, rather than biochemical signs, may be of more use (on a practical and clinical significance basis) when assessing mild dehydration and advising patients on what to look out for or prompting the use of ORS such as Hydralyte.12
Box 1. Clinical screening signs and symptoms for dehydration screening8,10
Box 2. Examples of biomarkers used to assess dehydration3,13
|
Body water balance imbalances
Having a better understanding of dehydration, its causes and risk factors can be helpful in identifying more vulnerable individuals, ensuring they receive adequate fluid intake and providing dehydration education.
Dehydration involves more than just the net loss of body water — it alters the volume, composition, and distribution of water within the body.7 In simple physiological terms ‘dehydration’ can be related to the ratio of water to electrolyte loss:14
Dehydration is the depletion of body water (with or without electrolytes) that results from increased fluid loss, decreased fluid intake, or both.7
Hypertonic (intracellular) dehydration
Water loss is greater than solute loss — which leads to a rise in the serum concentration of sodium (hypernatraemia) and an osmotic shift of water from the intracellular fluid (ICF) to the extracellular fluid (ECF).14,15
Causes include inadequate water intake (age-related thirst impairment), excessive water loss from sweating (exercise, heat or fever related), vomiting and diarrhoea, or the overuse of osmotic laxatives and diuretics.14,15
Hypotonic (extracellular) dehydration
Solute loss is greater than water loss — with decreasing sodium serum levels (hyponatraemia) that lead to an osmotic shift of water from the ECF to ICF.14
Causes include some instances of excessive sweating or gastrointestinal fluid losses, hyperglycaemia or where fluid and electrolyte deficits are treated with only water.14,15
Isotonic dehydration
Water and solutes are lost at the same rate — serum sodium concentration remains the same (isonatremia) and no osmotic movement of water occurs.14
Causes include occasions where solutes and water are lost through, for example, burns, vomiting and diarrhoea or inadequate fluid and salt intake.14,15
‘Everyday’ causes of dehydration
Anyone can become dehydrated — but some people and some ‘everyday’ occasions have a higher risk for developing dehydration than others, including:
Common illness such as gastroenteritis, colds or influenza
- Vomiting and diarrhoea symptoms can lead to loss of water and electrolytes10,15
- Fever with increased sweating can contribute to fluid imbalances10,14
- Reduced appetite means lost fluids are less likely to be replaced13,16
- Young children and older adults are especially vulnerable to dehydration.2,8
ORS is the standard treatment for mild to moderate dehydration secondary to gastroenteritis.2
Work or sports related exercise
- Sustained or vigorous exercise can lead to substantial water and electrolyte losses through excessive sweating — particularly under warm or hot conditions13
- Women and older adults may be at greater risk of fluid and electrolyte imbalances (hyponatraemia) during and after vigorous exercise13,17
- Dehydration may be associated with increased skeletal muscle cramps and impairs exercise performance.13,13
ORS can play a role before, during and after vigorous exercise.13,13
Travellers and holidaymakers
- Low air humid and hypobaric pressure in aircraft cabins can cause dehydration and contribute to ‘travel fatigue’18
- Gastrointestinal problems, such as traveller’s diarrhoea, can be common problems19
- Unaccustomed heat or humidity, and extreme physical activities can lead to water and electrolyte losses14
- Alcohol acts as a diuretic with the degree of diuresis being proportional to the amount of consumed alcohol.20
ORS can be conveniently packed for use when travelling.19
Life stages
- Infants and children, having higher water requirements per unit of body weight than adults, are more vulnerable to dehydration14
- Pregnancy may trigger feelings of nausea leading to poor appetite and vomiting21
- Fluid demands during breastfeeding can upset the mother’s body water balance14
- Older adults’ age-related physiological changes (thirst impairment, renal function), co-morbidities or medications put them at a higher risk of dehydration3
ORS can be used by all age groups and at every life stage.1
Make rehydration simple with Hydralyte – the importance of electrolytes and water
Replacing lost fluid and electrolytes is the most important initial step in managing dehydration.
Oral rehydration solutions — such as Hydralyte — are appropriate for adults and children with mild to moderate dehydration, supplying maintenance requirements by correcting volume and electrolyte deficits and replacing any ongoing abnormal losses.1
ORS need to have an optimal balance of sodium and glucose — glucose facilitates the absorption of sodium (and water) in the small intestine, and sodium and potassium are needed to replace the losses of these essential ions during dehydration.1
Sodium-glucose transport (SGLT) system22
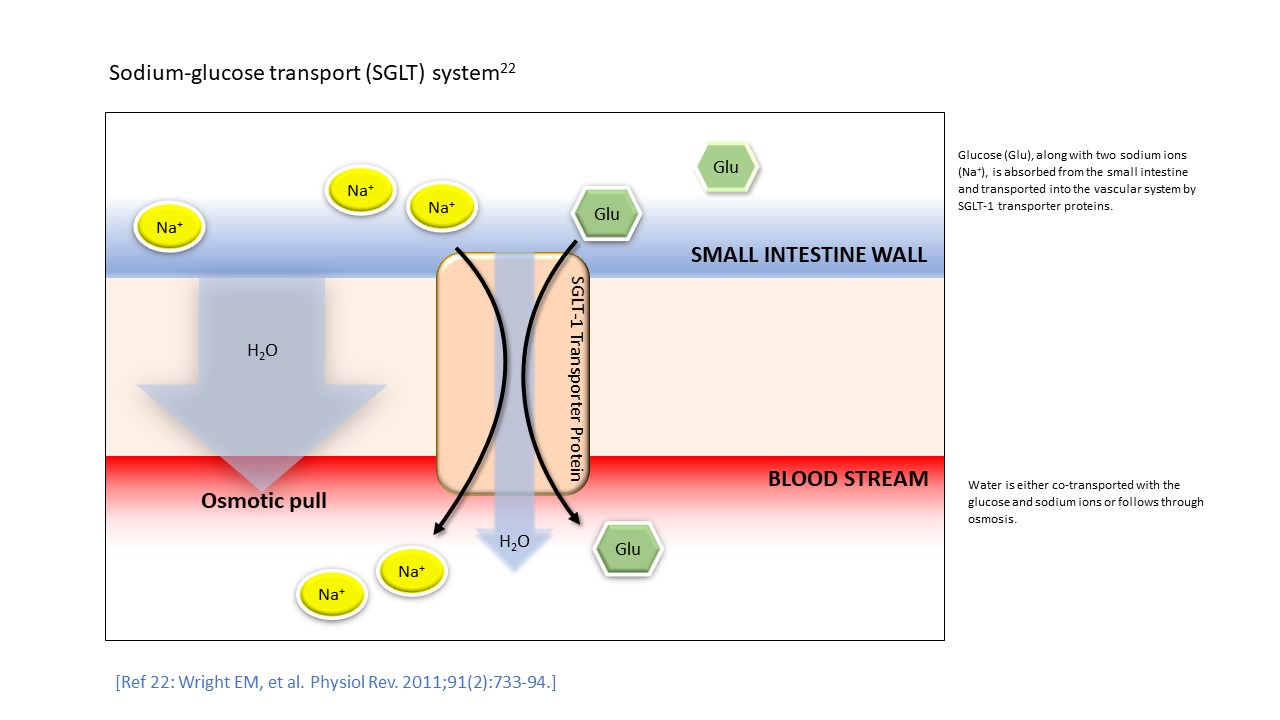
Not all ORS are the same, and ORS are not the same as sports or energy drinks— sugary drinks or water alone may not provide the correct electrolyte balance for rapid hydration.1
Why Hydralyte?
Hydralyte is specifically formulated to meet WHO ORS criteria for effective hydration (table 1) — helping to replace water and electrolytes lost due to vomiting and diarrhoea, heavy sweating, vigorous exercise, and other dehydrating conditions.4
The Hydralyte range:
- Have the correct balance of sodium and glucose in-line with WHO ORS recommendations
- Are hypotonic — allowing effective rehydration while minimising potential side effects such as a feeling of fullness/bloating
- Have a lower sodium content – formulated specifically for the diets of developed countries
- Contain low sugar
- Are suitable for all age populations (0 – Adult)
- Available in a variety of formats and flavours.
For further information contact Care Pharmaceuticals: FREECALL Australia 1800 788 870 www.hydralyte.com.au
Table 1. Hydralyte oral rehydration solutions: ingredient comparison
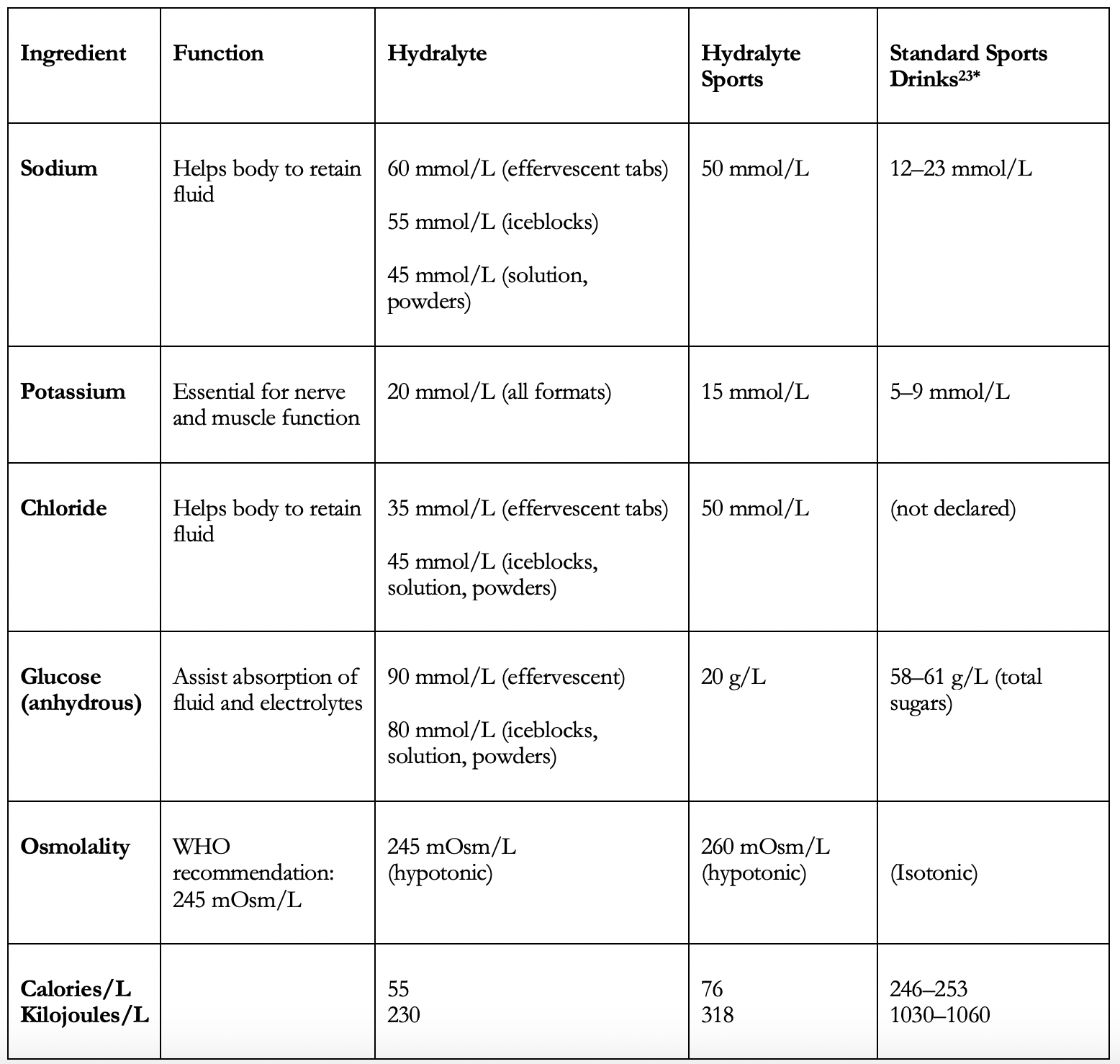
*Values from three commercially available standard sports drinks
References
- World Health Organisation (WHO). Oral rehydration salts. Production of the new ORS. 2006. Available at: https://www.who.int/maternal_child_adolescent/documents/fch_cah_06_1/en/ (accessed May 2020).
- Harris C, Wilkinson F, Mazza D, Turner T; Health for Kids Guideline Development Group. Evidence based guideline for the management of diarrhoea with or without vomiting in children. Aust Fam Physician. 2008;37(6 Spec No):22?9.
- Woodward, M. Guidelines to effective hydration in aged care facilities. Aged & Residential Care Services, Heidelberg Repatriation Hospital. April 2013. Available at: https://www.semanticscholar.org (accessed May 2020).
- TGA Public summary. Hydralyte Orange Flavoured Electrolyte Powder. Available at: https://www.ebs.tga.gov.au/servlet/xmlmillr6?dbid=ebs%2FPublicHTML%2FpdfStore.nsf&docid=F229C741C69FCC78CA25832B003CB904&agid=(PrintDetailsPublic)&actionid=1 (accessed June 2020).
- Sankoff J. Heat illnesses: a hot topic in the setting of global climate change. Aust Fam Physician. 2015;44(1-2):22?6.
- Cheuvront SN, Kenefick RW, Charkoudian N, Sawka MN. Physiologic basis for understanding quantitative dehydration assessment. Am J Clin Nutr. 2013;97(3):455?62.
- Thomas DR, Cote TR, Lawhorne L, et al. Understanding clinical dehydration and its treatment. J Am Med Dir Assoc. 2008;9(5):292?301.
- Campbell, N. Recognising and preventing dehydration among patients. Nursing Times. 2014;110:20-1.
- Fortes MB, Owen JA, Raymond-Barker P, et al. Is this elderly patient dehydrated? Diagnostic accuracy of hydration assessment using physical signs, urine, and saliva markers. J Am Med Dir Assoc. 2015;16(3):221?8.
- World Health Organization (WHO). The treatment of diarrhoea: a manual for physicians and other senior health workers (4th rev). 2005. Available at: https://www.who.int/maternal_child_adolescent/documents/9241593180/en/ (accessed May 2020).
- Bak A, Tsiami A, Greene C. Methods of assessment of hydration status and their usefulness in detecting dehydration in the elderly. Curr Res Nutr Food Sci. 2017;5:43-54.
- Vivanti A, Harvey K, Ash S, Battistutta D. Clinical assessment of dehydration in older people admitted to hospital: what are the strongest indicators? Arch Gerontol Geriatr. 2008;47(3):340?55.
- American College of Sports Medicine, Sawka MN, Burke LM, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377?90.
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA); Scientific Opinion on Dietary reference values for water. EFSA Journal 2010; 8(3):1459. [48 pp.]. Available at: www.efsa.europa.eu accessed May 2020).
- El-Sharkawy AM, Sahota O, Lobo DN. Acute and chronic effects of hydration status on health. Nutr Rev. 2015;73 Suppl 2:97?109.
- Pilgrim AL, Sayer AA. An overview of appetite decline in older people. Nurs Older People. 2015;27(5):29-35.
- Brun SP. Clinical considerations for the ageing athlete. Aust Fam Physician. 2016;45(7):478?83.
- Huyghe T, Scanlan AT, Dalbo VJ, Calleja-González J. The Negative Influence of Air Travel on Health and Performance in the National Basketball Association: A Narrative Review. Sports (Basel). 2018;6(3):89.
- Leder K. Advising travellers about management of travellers’ diarrhoea. Aust Fam Physician. 2015;44(1-2):34?37.
- Shirreffs SM, Maughan RJ. Restoration of fluid balance after exercise-induced dehydration: effects of alcohol consumption. J Appl Physiol 1997;83(4):1152?8.
- Patil CL, Abrams ET, Steinmetz AR, Young SL. Appetite sensations and nausea and vomiting in pregnancy: an overview of the explanations. Ecol Food Nutr. 2012;51(5):394?417.
- Wright EM, Loo DD, Hirayama BA. Biology of human sodium glucose transporters. Physiol Rev. 2011;91(2):733?94.
- Data on file (standard sports drink ingredients).


