General practice clinics are getting help identifying patients hiding in their healthcare records.
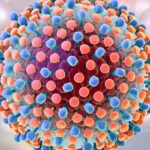
A major new project has been launched to help GPs uncover the estimated 50,000 Australians living with hepatitis C who are yet to access treatment.
The Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) estimates around 50,000 people have tested positive to hepatitis C and have not yet accessed treatment or are at a high risk of having the chronic infection.
The project, which gives clinics $1500 for participating, trains staff to audit their data using risk factors such as a history of incarceration and injecting drug use.
The aim is to help practices identify hepatitis C positive patients and treat them with the direct acting antivirals that have now cured around half of those with the disease in this country.
Heather Drummond, practice manager at Mindarie Super Clinic in Western Australia, said their clinic had diagnosed 47 patients while participating in Beyond the C’s pilot project.
“It’s important for us at a practice level to ensure that our patients know that there is a cure for hepatitis C, and then they can make an informed decision about what they want to do.”
Ms Drummond said the funding gave the clinic allocated time for data extraction and patient follow-up, using tools to streamline the data extraction process. It also enabled patients to see their GP rather than a specialist.
“It also gave us the ability to and the resources to upskill our clinical team about the treatment of hepatitis C at a practice level, because many patients previously when they were diagnosed with hepatitis C, were often sent to a specialist.
“With the introduction of antiviral medicines to the market, it meant that most patients with hepatitis C could have treatment from their general practitioner.”
ASHM hepatitis C program manager Phoebe Schroder said that anecdotally, it was common for patients to have a positive antibody test, showing they had been exposed to hepatitis C, but not remain in contact with the healthcare system for treatment.
The clinical auditing project helped clinicians search their databases to find people who maybe have been diagnosed with hepatitis C but may not have a cure or confirmatory RNA test on file.
“There are misconceptions among both patients and healthcare professionals regarding how to receive an accurate diagnosis of hepatitis C, with some patients potentially feeling as though they have hepatitis C without having the confirmatory RNA test,” Ms Schroder said.
“A practice may have a lot of people listed as having had a hepatitis C antibody test, and this project will help them understand how to do an audit and recall those patients to make sure that they have been linked into care where appropriate, that they have been tested and are aware of their status, and what will be of best use for that patient moving forward.”
Many patients may have never accessed treatment due to a lack of trust in the healthcare system and a fear of stigma and discrimination, Ms Schroder added.
“A lot of people with hepatitis C are people who are often marginalised. The most common mode of transmission of hepatitis C is via injecting drug use, and people who inject drugs are often marginalised and may face multiple barriers to engage with healthcare.”
Clinicians may need to have more than one conversation about hepatitis C with patients, who may face several barriers to seeking care, she said.
“If you ask someone to come back for a test, and it’s not the right time for them, try again, and try that respectfully, but don’t push it too hard. Work with them and make sure that it’s right for them.”
The project also allowed GPs to claim CPD hours for quality improvement activities, and clinics received $1500 after completing the program.
General practices are eligible to take part if they are accredited, have the capacity to extract data from practice software, and complete a terms of reference document before enrolling. Projects are completed in six months but can be finished earlier.