The state’s first patients have begun treatment with medically enhanced psychotherapy for PTSD and treatment-resistant depression.
The first clinic in NSW to offer psychedelic-assisted therapy has begun seeing patients with post-traumatic stress disorder and treatment-resistant depression.
Evolution Medicine Enhanced Therapy saw its first patient – an Indigenous woman from southwest Sydney with transgenerational trauma and a history of abuse – last Wednesday, the same day as an FDA advisory committee recommended against the approval of therapeutic MDMA in the US.
The committee’s specific concerns about the research from Lykos, the company applying for approval, overshadowed concerns about MDMA itself. These included a perceived lack of rigour, accusations of misconduct and a history of pro-MDMA activism at the company, which was previously known as MAPS PBC – a subsidiary of the Multidisciplinary Association for Psychedelic Studies (MAPS).
Evolution MET’s treatment involves extensive preparation then either two or three cycles of dosing sessions followed by multiple psychotherapy sessions.
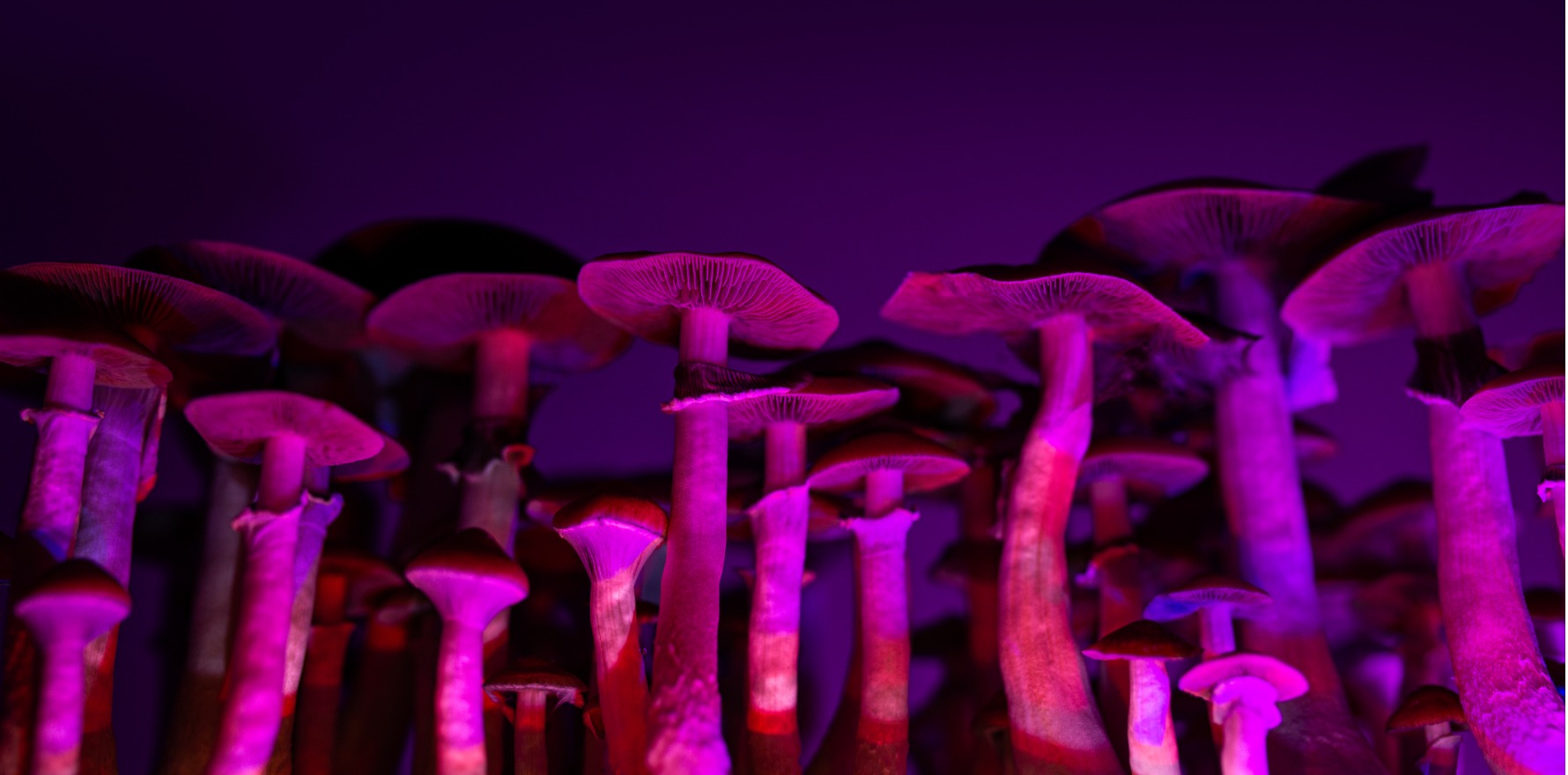
In a controversial world first, the TGA downscheduled MDMA and psilocybin in February last year, allowing them to be prescribed by psychiatrists for PTSD and treatment-resistant depression respectively.
Director Associate Professor Ranil Gunewardene from Macquarie University told The Medical Republic that Evolution MET was the only credentialled operator on the TGA’s authorised prescriber scheme so far in the state, with three others in Victoria.
His clinic is treating patients in a registered Phase IV “real world” clinical trial to help add to the body of evidence, which critics of the TGA decision said was lacking.
Professor Gunewardene said the treatment was only for specific classes of patient.
“These are people for whom traditional and conventional treatments have been either ineffective or had very limited effect,” he said.
“Conventional treatments still have an important role, but if they’re not working, then exploring alternative treatments that do have an evidence base is reasonable, provided the safety and tolerability have been established. And in my opinion, the studies that the MAPS group did in the US were large, high-quality, multi-centre studies that did establish safety and tolerability.
“There is a need for more research and more evidence, and that’s why we set up our service as a phase IV clinical trial to assess how effective these treatments are in the general public.”
Related
After being screened for excluding conditions, patients undergo four preparatory sessions to identify goals for the therapy and learn more about what to expect. That’s followed by a full “medicine day” with MDMA dosing, then three “integration sessions” of psychotherapy to make sense of what happened in the MDMA sessions; a second dosing day and three more integration sessions; and a third dosing day and three more sessions, after which patients continue treatment with an outside therapist.
This is in line with protocols from the MAPS trials, as is the dose schedule of 120mg with a 60mg top-up two hours later to prolong the effect.
For this triple treatment cycle, which is the minimum for any trauma patient, Professor Gunewardene said the cost would be $17,000, or $13,000 for a double cycle.
“People ask why it’s expensive,” he said. “Per hour, you’re getting treated for less than normal private practice rates, but it adds up when you have that many hours of therapy.”
The preparatory sessions uncover the specifics of the patient’s trauma. When dosed, the patient processes these experiences while listening to music and wearing an eye mask.
“Your brain and mind dives into your past, your experiences, relationships, traumas, setbacks, failures, disasters and pain and suffering. But … you’re revisiting it in this enlightened state of mind. The amygdala – the fear centre – gets shut down or tuned down by MDMA, and the patient’s cosseted by the dopamine, oxytocin and serotonin being released. You’ve got this protective wellbeing, but you can still feel pain and suffering – there’s a lot of crying and distress, but the enormity of the pain is altered.
“You feel many emotions while you’re experiencing this thing, but you’re in a state of compassion and understanding and wisdom.
“The analogy I use is that it’s a little bit like the Dalai Lama revisiting your life story instead of you, and the hope is that the story gets rewritten with different beliefs and perspectives, as opposed to the vulnerable child experiencing these terrible things.”
He said trauma was a “massive cause of impairment and suffering in the community” and was not well understood. PTSD was still popularly associated with the military experience, he said, while most of it in fact resulted from abuse and violence in families of origin.
Another large category was road trauma, which included parents who had had to identify their children’s bodies, read autopsy reports and so on.
Another one of his patients who consented for their details to become public was Adam Bray, the father of one of the victims of last year’s Hunter Valley bus crash.
Professor Gunewardene said the process for treatment-resistant depression was similarly structured, though psilocybin was a very different drug.
The nature of treatment-resistant depression was that everything else had failed, which meant an alternative was worth trying even if the odds were somewhat stacked against recovery, he said.
“The response rates in this group are not going to be necessarily overwhelming, but even if it is helping a number of people, that’s worth exploring in a careful and judicious way.”