Everyone knows the PSR is procedurally unfair and does not serve the public interest – so why is the government so hell bent on defending it?
As GPs gear up to start vaccinating their patients for COVID, we know that at least 500 will be receiving a letter from the PSR about potentially inappropriate billing for telehealth early in the pandemic.
It is clear from the initial number of the letters the PSR had planned to send – 9,700 – that the telehealth rules weren’t clear enough from the outset for most GPs. The rules were changed on the run. There was much panic and stress amid a pandemic.
As far as vaccinations go, there are also quite a few blurred lines and shifting goalposts for GPs to start interpreting in terms of billing rules.
When can you claim a pre-consult without actually giving a vaccine? Can you turn patients away who aren’t your normal patients? Under what circumstances will it be OK to make a co-payment for another consult during a vaccination item session? What are you allowed to advertise to patients when you get vaccine? And so on.
As the result of a rapidly evolving process, and one which naturally has to iterate in real time to meet unexpected health and logistical challenges, the rules by which GPs are claiming payment can’t ever be very clear.
So why does the government persist with a costly taxpayer-funded legal campaign to defend a compliance regime for doctors which is broken?
On the last day of a three-day hearing this week in the Federal Court testing just how broken the PSR is the judge presiding called the process a “Star Chamber” and referred to it as unaccountable and oppressive.
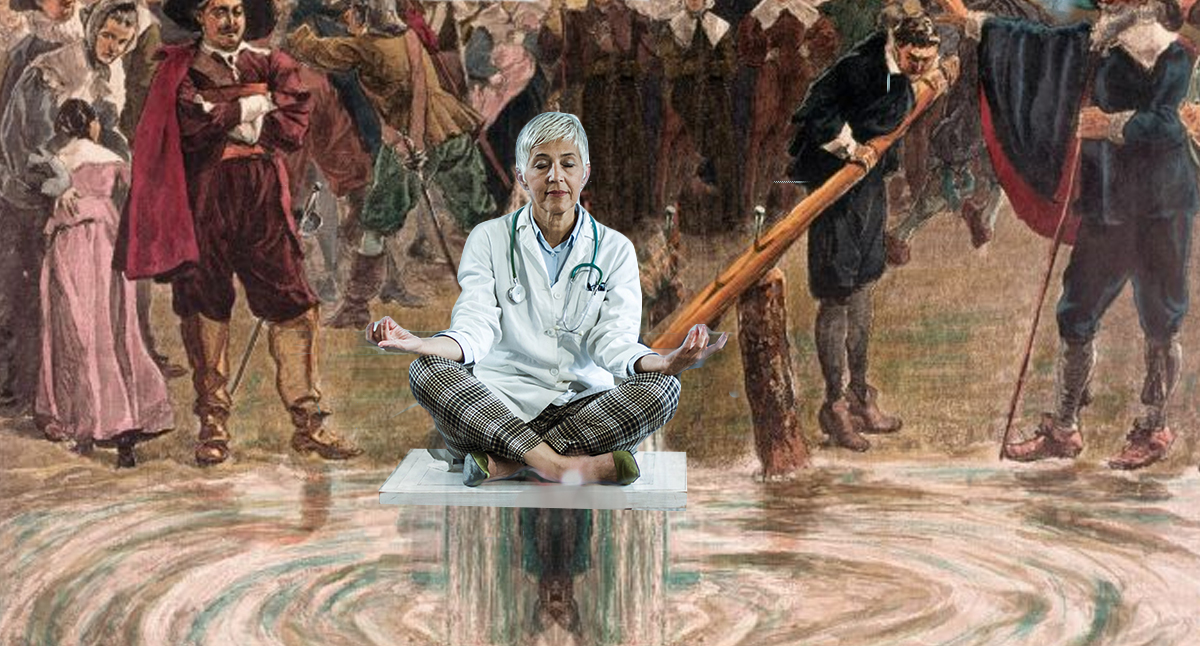
This week’s case was the government’s fourth go at knocking out an unusually stubborn doctor who fell foul of the PSR more than four years ago, and decided early in the process that something was dreadfully wrong with how she was identified, and “processed”, with virtually no rights in normal law available to her to defend herself.
Dr Anchita Karmakar was working as a GP registrar on the Gold Coast when her billing patterns came to the PSR’s attention. Her practice, despite being her supervisor, was not investigated and fired her during the process.
Dr Karmakar claimed she was denied procedural fairness as she could not have legal representation (not effective representation – you can hire a lawyer but they can’t talk) and there was no education nor any fixed standards on appropriate Medicare billing.
Dr Karmakar isn’t the first doctor to stand up to the government and point out a system that is operating for doctors outside the rule of law, and which has a lot in common with other flawed government programs such as Robodebt.
It is a “guilty, until you prove yourself innocent” process, with a few slightly awkward rules thrown in for doctors in the case of the PSR, which prevent them from actually being able to prove anything during the review process, or be professionally represented.
Through a secrecy clause in the Health Insurance Act (106ZR), doctors have no access to previous case findings and deliberations to provide context to any defence, and subjects of PSR reviews are prohibited – on penalty of 12 months’ imprisonment – from discussing their case with others. Quite a catch 22, even for the Department of Health (DoH), but one that has persisted now for just over a decade.
In recent years the DoH has started doubling down on its compliance efforts through spreading fear as a means of keeping doctors in check, using targeted “nudge” letters (letters to doctors based on data analytics which warn them that they are outside the normal distribution of practice or prescribing, and under scrutiny so they should immediately review their practices and consider changing them or face further investigation).
There are numerous very serious issues with the whole PSR set up which are entirely obvious to everyone, including the government, and they’ve been obvious for a long time: while it has been rare for a doctor to take on the government in this one-sided, expensive, stressful and shaming process, some have tried to take on the PSR in the courts many years before Dr Kamarkar in an attempt to expose the system as procedurally unfair and not in the public interest.
A key underlying issue for the government was exposed as far back as 1980 in a High Court ruling in the General Practitioners Society v Commonwealth (1980) which found that “there is no explicit head of power under which the Federal Parliament can regulate private medical practice, in the sense of the physician-patient relationship … Medicare does not have a constitutional right to deliberate in that area as a government agency”.
The government had argued that doctors who bulk bill their patients enter a contractual arrangement with the government and therefore must abide by the rules of Medicare.
But the case of Health Insurance Commission vs Peverill (1994) 179 CLR 226 decided that bulk billing is actually a contract between the patient and the doctor so the doctor is not brought into a contractual relationship with the government.
The Peverill case also demonstrated that the PSR was in some instances economically coercing doctors to stop providing patient care that a patient might want and may need.
In this case a female doctor had set up a dedicated female doctor clinic to provide an alternative service after a male doctor was found to be sexually abusing female patients. Medicare statistically determined that this female doctor was rorting the system because the stats said she was a big outlier on the pap smear prescribing graph. No one enquired as to the context of the situation. This doctor was asked to settle and threatened that if she didn’t, she would be faced with going through the PSR process.
Another key element of Dr Kamakar’s case is how broadly the Health Insurance Act defines a “professional service”, and how difficult it is for doctors to define the line of what is a “clinically relevant service” or not, and then to defend themselves if the PSR deems they have crossed “the” line (that being the PSR’s determined line).
What constitutes a clinically relevant and necessary professional medical service is framed broadly by the Act in order to facilitate the “art of medicine”. Doctors are able to exercise “appropriate clinical discretion” on a “case-by-case basis”, according to the Act.
When things get to the PSR however, this particular element of the legislation tends to work against a doctor. The judgement of the “clinical line not to cross” is in essence being directed by Medicare, not a doctor. PSR detractors point out that the government does not have agency to make clinical judgements under law, especially when that judgement is conflicted significantly by the issue of collecting and monitoring monetary payment for the government.
The PSR attempts to get around the issue of clinical relevance by using a “panel of doctor peers” to help assess when a doctor argues their clinical case. “Is that something that I as a reasonable and fairly practising doctor would do?”
But the panels of “peers” – sometimes including senior fellows in college leadership positions – are clearly conflicted and do not constitute any process that would be recognised as evidence in a court of law.
The assessment in this instance is not only without due process, it could be significantly conflicted by the views of a class of doctors with potential political agendas, practising in a completely different set of circumstances to the doctor being assessed, and with sometimes strong views guided by their different experiences as Australian trained GPs.
As peers change from each PSR process to the next, the process could be deemed as quite random in terms of meaningful legal assessment of what is “clinically relevant”. Who decides who sits on a peer panel and who gets review of that assessment? At least in a court of law jury case a defendant has some influence on who sits on a jury.
Doctors have no option but to engage and comply with Medicare, despite the fact that there is limited guidance as to how the scheme works, the convoluted nature in which items can be introduced, dropped and managed (eg, recent telehealth items and new vaccination items), and how to bill correctly.
It is obvious to everyone that the system is confusing and that threshold decisions made by doctors in the best interest of their patients can create unintentional non-compliant billing to occur.
But the system is the system as far as the government is concerned.
For some reason, the PSR and the system as it currently operates has largely been left alone by the RACGP over the years as far as any serious systemic issues are concerned. The college will from time to time make representation to the DoH about how many nudge letters it intends to send and why, but it has never mounted a case that the whole system is rotten and needs to be overhauled, as it probably should if it is in the business of member advocacy.
When senior RACGP personalities sit on the peer review panels of the PSR, it can hardly reassure members the college has their backs.
For all intents and purposes the PSR is supported by the AMA, despite its clear faults. There are clear political issues in play here which are warning the major colleges away from addressing the problem. In the case of the RACGP it’s probably the same old issue that it is a training college at heart, funded by the existence of a mandate given it by the government in the first place. It can’t afford to rock the DoH boat too much.
Quite rightly the government asserts that given the huge amounts of money flowing through Medicare each year, some form of oversight and compliance is required in order to keep the system in check and protect the public purse from potential plunder.
But it persists with a system which is palpably unfair and which is very likely distorting the practice of medicine and patient outcomes. It is also likely costing doctors a lot of money as they make sure there is a large buffer between what they actually think is good practice and what they assess the PSR might end up thinking is good practice.
The government attempts to argue the point that the system must be working because when you look at how many doctors get caught out by the system each year, the number is minuscule. It is. In 2019 only 79 doctors fell foul of the system and had to repay a total of $24.4million. That’s against 88,000 practising doctors in the country and an MBS total spend per year of $20.2 billion in that year.
But is this the system working, or doctors just being good doctors? And even if the system is working for the government, it very clearly isn’t working for doctors and patients. Do they not have a say in this arrangement?
Given the history of cases and the increasing pressure that seems to be on the DoH about how it works you get the sense that the government understands that it’s a pretty rough and ready system, if you end up in the system, but it’s the best solution available and at the end of the day, its working, so let’s not change it. There’s some merit in not changing something that the government actually might have working, but is it really working when:
- the lives of doctors caught in the system are unfairly ruined or significantly disrupted unfairly
- the “the rule of law” which the government is so fond of spruiking everywhere for political advantage is simply ignored in the case of the PSR process
- the system as it stands is unaccountable , works on a “guilty until proven innocent” principle , denies doctors access to “due legal process” to defend themselves, preys on the weak (single doctors, often marginalised ones such as IMGs), and is largely non-reviewable
- the system relies on “fear” to keep doctors in check which is likely creating significant workplace issues across medical practices around the country
- the system is a government billing agency attempting to dictate “clinical management” with a view to saving money, not lives, which is likely warping clinical practice across the country in bad ways
- the system discourages a healthy patient-doctor patient relationship by retarding the doctor’s ability to care and innovate in the way they might think best and safest for their patient?
With so many factors aligned against the PSR and how it works, why does the government expend an inordinate amount of money and time acting as a non model litigant (the government is mandated to act as a model litigant) in trying to prevent someone like Dr Karmakar from proving their case? We understand the tactics to keep Dr Karmakar from progressing through her case have been particularly technical and dirty. Apparently the government will stoop to any legal argument no matter how banal or technical, that has the effect of preventing Dr Karmakar’s allegations being found true.
Principles and ethics are not in play here, as is often the case in high stakes precedent cases of law.
The most likely reason is that this case has now gone so far and become so high profile that the the potential ramifications of any precedent that the case is likely to set are ghastly for some in power. If Dr Karmakar wins she would be proving a major government department was denying access to “due legal process”. The case even has ramifications for freedom of speech.
You suspect that the DoH has persisted in holding its ground all these years because for at least the last 10 years a little persistence has brought about good returns. No one has been prepared to risk their their savings, sanity and reputation to point out that while there has to be a policeman of sorts to govern and promote sensible and meaningful Medicare billing, the PSR process of governance has been one of control through fear created by an unquestionably unfair process.
The DoH probably should have started stepping back from the this position some years ago.
But it hasn’t, and if Dr Karmakar wins on any aspects of “due and fair process” in the judgement, the ruling may well end up forming a precedent the public can start to use to challenge the undisputed champions of reversing the concept of “due process” – the Australian Tax Office.
This is almost certainly why the government is now panicking and throwing money at the case.
If the PSR process, which has all the elements of how the ATO will often rule on tax constructions, and which has a lot of Robodebt in it (fear, retribution and no easy redress for parties least able to defend themselves), is found to be systemically unfair (which it is) then we might have a precedent that is applicable across other all government agencies, including the ATO.
And won’t that create some genuine panic for everyone in government.