The Medicare watchdog clawed back almost $32 million from practitioners this financial year.
For the first time in five years, the Professional Services Review didn’t find any evidence of practitioners committing suspected Medicare fraud – but findings of inappropriate practice at the committee stage remain at 100%.
The PSR released its annual report for the 2023-24 financial year last week, revealing it had made agreements and final determinations for repayment orders totalling $31.6 million; an increase of $10 million on the 2022-23 year and $12 million on 2021-22.
It’s a big number even by pre-pandemic standards; total repayment orders were $26.4 million in 2019 and $16.2 million in 2018.
In fact, before 2018, the agency had never cracked $10 million in total repayment orders.
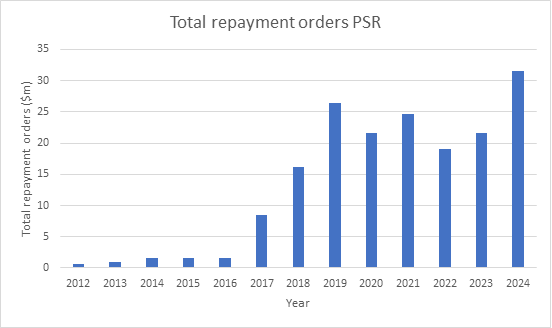
Source: PSR annual report archive
The PSR does not collect nor receive any of the money it orders repaid; that process is managed by the Department of Health and Aged Care.
Despite the record high repayment figure, the number of cases referred to the agency by Medicare – 109 – was consistent with the 102-case average over the previous six years.
Once a case is referred to the PSR, there are three stages.
In the first instance, the director may choose to take no further action, which is akin to a not guilty verdict in that no repayment has to be made and no reprimand is recorded.
No further action was taken in nine cases this year; while lower than 2023’s seven-year high of 19, it was still significantly higher than the four years immediately preceding it.
At the next stage, practitioners can elect to negotiate an agreement with the PSR in which they admit to having engaged in inappropriate practice.
This normally involves a repayment order as well as a reprimand, counselling order or a partial disqualification from the MBS.
Consistent with previous years, 87 practitioners entered into negotiated agreements with the PSR in 2024.
The highest single repayment order at the negotiated agreement phase was $1.2 million.
Practitioners who do not enter into an agreement may be referred to a committee of their peers, who make a judgement on whether they have billed inappropriately.
These take time and rarely work out in the practitioner’s favour.
Over the last six years, just one practitioner has emerged from a committee hearing with a finding of no inappropriate practice.
Of the 14 cases before committees that reported back in 2024, all 14 resulted in findings of inappropriate practice.
Related
In one case, a practitioner was ordered to repay close to $2 million.
The most commonly pinged items for GPs this year were level B, C and D consultations (MBS items 23, 36 and 44), chronic disease management items (MBS items 721, 723 and 732), mental health items (including 2713 and 2715) and their equivalent telephone consultation items.
Video telehealth items “did not feature as a concern”.
“As in other years, submissions made by practitioners reviewed by PSR indicate that a great majority made positive changes to their practice as a result of the review process,” agency director Dr Antonio Di Dio wrote.
“In most cases reviewed during 2023–24, inappropriate practice involved inadequate clinical notes, failure to comply with the requirements of the MBS items, inadequate clinical input into services, or prescribing concerns.”





