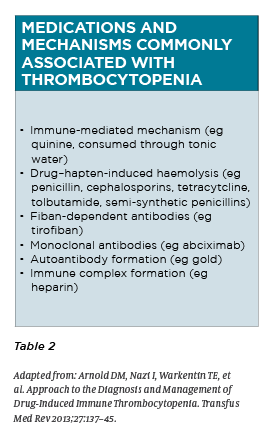
A look at some of the common causes of a low platelet count and which features warrant urgent referral to a haematologist
Thrombocytopenia or a low platelet count is often encountered in general practice incidentally when ordering a full blood count. The cause is not always immediately apparent and further investigation is usually warranted.
The patient is recalled and a focused history and exam along with further investigations is done.
Thrombocytopenia is defined as a platelet count below 150 x 109/L. This can be further classified as mild (100-150 x 109/L), moderate (50-100 x 109/L) and severe (<50 x 109/L).
Patients with platelet counts greater than 50 x 109/L are often asymptomatic. A count from 10 – 30 x 109/L may cause bleeding with minimal trauma, while counts less than 10 x 109/L increase the risk of spontaneous bleeding, petechiae, and bruising.
Spontaneous bleeding (e.g. mucosal, intracranial, gastrointestinal, and genitourinary bleeding) is most likely to occur in patients with platelet counts less than
5 x 109/L and is considered a haematological emergency.1
INITIAL EVALUATION
Clinical history
A thorough history and physical examination can provide invaluable information and greatly facilitate diagnosis. Aspects of particular relevance include:
Symptom history: easy bruising or petechiae, melaena, rashes, fevers, and bleeding.
Temporal profile of the thrombocytopenia
Medical comorbidities: e.g. autoimmune disorders, infections, malignancies, recent organ transplantation
Recent medications and immunisations
Family history of thrombocytopenia
Pregnancy status in pre-menopausal women
Recent travel history
Transfusion history
Alcohol intake and intake of quinine-containing beverages
Dietary habits (e.g. Vitamin B12, folate deficiency)
Risk factors for retroviral infections and viral hepatitis
Recent heparin exposure (within 30 days)
Physical examination
Physical examination should focus on the location and severity of bleeding risk. Thrombocytopenia typically manifests with mucocutaneous bleeding, while the presence of joint or soft tissue bleeding is more suggestive of coagulation abnormalities. The presence of an ischaemic limb or skin necrosis, especially in the context of recent hospitalisation, should raise suspicion of heparin-induced thrombocytopenia.
Other abnormalities that can help in the diagnosis of the thrombocytopenia include lymphadenopathy and hepatosplenomegaly.
PRACTICAL APPROACH
Is it a true thrombocytopenia?
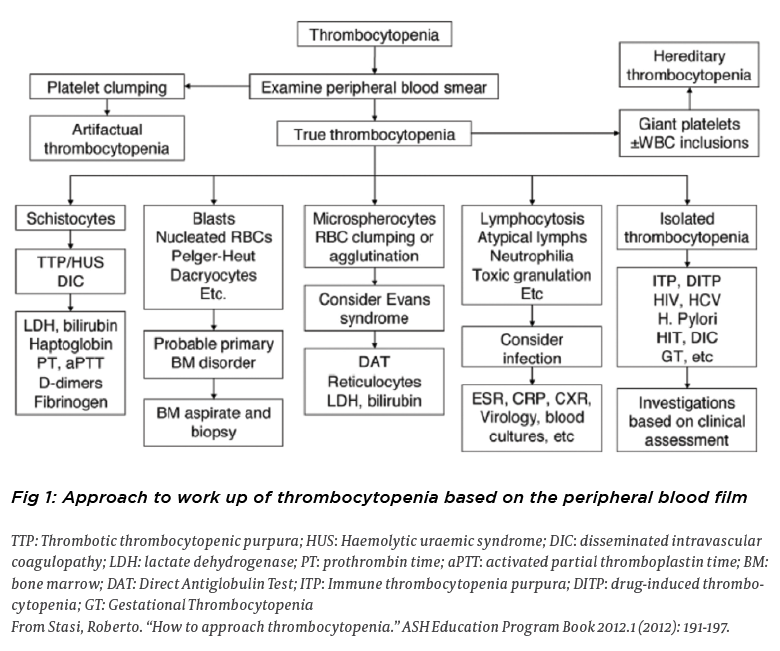
A repeat platelet count and blood film should be obtained in the case of any unexpected or new thrombocytopenia to exclude spurious results. Causes include delayed processing, laboratory error and artefactual thrombocytopenias due to fibrin stranding or platelet clumping.
Platelet clumping occurs in one in 1,000 people in the general population and is commonly caused by ethylenediaminetetraacetic acid (EDTA)–dependent agglutinins.3 This has no clinical significance. The platelet count should be repeated by collecting blood in a tube with a non-EDTA anticoagulant such as sodium citrate or oxalate.
Is it an isolated thrombocytopenia or associated with other FBC abnormalities?
The most common causes of isolated thrombocytopenias are ITP and drug-induced thrombocytopenia2
A blood film should be requested and carefully examined for platelet morphology and abnormal RBC or WBC features
A blood film approach to thrombocytopenia is presented in figure 1
First-line laboratory tests when investigating a thrombocytopenia:
Renal and liver function tests
Coagulation tests and fibrinogen
Vitamin B12 and folate studies
Autoimmune serology: ANA, ENA, ANCA, Rheumatoid factor
Viral studies: Monospot/EBV serology; HIV/HBV/HCV serology
Ancillary tests
Haemolytic screen: DAT, LDH, bilirubin, reticulocyte count, haptoglobin
Abdominal U/S – exclude splenomegaly which may cause a consumptive thrombocytopenia
CXR: to exclude overt evidence of mediastinal lymphadenopathy and TB
Peripheral blood flow cytometry – if abnormal lymphocytes are noted on blood film or there is a lymphocytosis. To exclude a lymphoproliferative disorder
H. pylori screening
Bone marrow biopsy
EMERGENT CAUSES
Immune thrombocytopenia purpura (ITP)
ITP is an acquired immune-mediated disorder characterised by an isolated thrombocytopenia and the absence of other causes of thrombocytopenia. Although it is a diagnosis of exclusion, responsiveness to corticosteroids is highly suggestive of ITP. The incidence is 3.3 per 100 000 adults per year, however, 50% of cases occur in children. 4
Important differences exist between paediatric and adult ITP. In children, ITP is more likely to present with significant (non-intracranial) bleeding but is also more likely to spontaneously resolve. In contrast, adult ITP affects more females than males, is more likely to present with intra-cranial haemorrhage, and tends to remain a chronic disorder. 5
The risk of bleeding correlates with the severity of thrombocytopenia, however, other risk factors include older age and concurrent anti-platelet therapy. Patients may present without symptoms, with minimal bleeding, or with serious haemorrhage (e.g. mucosal, intracranial and gastrointestinal). 2 ITP may be primary (idiopathic) or secondary to an underlying disorder, including autoimmune disorders (systemic lupus erythematosus, antiphospholipid syndrome, sarcoidosis), lymphoproliferative disorders, and infections (e.g., HIV, EBV, CMV, varicella-zoster virus, hepatitis C virus, Helicobacter pylori). Testing to exclude other causes should be performed as clinically indicated. 6 Treatment is generally only required if PLT < 30 or <50 with evidence of active bleeding. First-line treatment is high dose corticosteroids with a response typically occurring within one week of initiation.
In the case of severe thrombocytopenia and bleeding, intravenous immunoglobulin and platelet transfusions are also incorporated. Any patient older than 60 presenting with an isolated thrombocytopenia (PLT < 100) with no apparent cause should be referred to a haematologist for exclusion of an underlying haematological malignancy such as myelodysplastic syndrome and lymphoproliferative disorders.6
Thrombotic thrombocytopenia purpura (TTP)
TTP is a rare condition with an incidence of two per million per year. 7 It is characterised by severe deficiency of A Disintegrin And Metalloproteinase with Thrombospondin type 1 motif, member 13 (ADAMTS13), resulting in widespread microvascular thrombosis, tissue ischaemia and necrosis.
Patients classically have thrombocytopenia and microangiopathic haemolytic anaemia and should be referred to hospital as a medical emergency. This condition primarily affects adults, typically young females with a peak incidence in the thirs to fourth decades. Associated features include renal impairment, neurological symptoms (e.g. headaches, disorientation, seizures), and fever. It is fatal without treatment and requires prompt initiation of plasma exchange.8
Pre-eclampsia and HELLP (haemolysis, elevated LFTs, low platelets)
Pregnant patients beyond 20 weeks’ gestation with thrombocytopenia or signs and symptoms such as headache, visual disturbances, right upper quadrant abdominal pain, or elevated blood pressure should be evaluated for preeclampsia and HELLP syndrome.
Severe pre-eclampsia occurs in 15-20% of pregnancies, while HELLP accounts for <1% of causes of thrombocytopenia in pregnancy.16 Other laboratory abnormalities may include anaemia, elevated liver enzymes, elevated lactate dehydrogenase, and proteinuria. The definitive treatment is delivery of the foetus. 9 Other important causes of thrombocytopenia that can mimic HELLP syndrome include DIC and TTP. Generally speaking, pregnant patients with PLT < 80 should be referred for haematology review in conjunction with obstetricians in the high risk antenatal clinic. 16
Other emergent causes of thrombocytopenia
Aplastic anemia, chemotherapy, irradiation, acute leukaemias, and myelodysplastic disorders may result in severe or symptomatic thrombocytopenia. Similarly, hospitalised patients with sepsis, trauma, burns, or malignancy, can develop disseminated intravascular coagulation with resultant thrombocytopenia.
Paroxysmal nocturnal haemoglobinuria is associated with haemolysis, renal disease, and thrombotic complications, typically in unusual locations. Diagnosis is by flow cytometry.10
NON-EMERGENT THROMBOCYTOPENIA
Drug-induced thrombocytopenia (DIT)
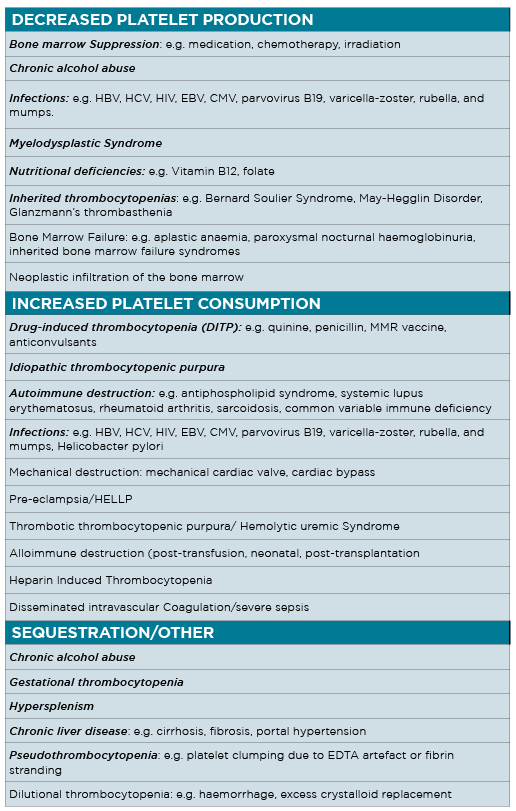
One of the most common types of thrombocytopenia in the outpatient setting is DIT. The annual incidence is approximately 10 cases per ine million persons. 11 Drug-induced thrombocytopenia should be suspected in all patients presenting with an acute drop in platelet count. It typically occurs within five to seven days of exposure to the causative agent and usually resolves within seven to14 days after discontinuation. 12
Most patients with drug-induced thrombocytopenia have moderate to severe thrombocytopenia reaching a nadir platelet count of 20 × 109/L. 13
Quinine is a common cause of drug-induced thrombocytopenia and often is missed in the patient history. Table 2 lists the common medications and their proposed mechanisms of action. 13 If drug-induced thrombocytopenia is suspected, the causative medication should be discontinued and the patient’s platelet count should be repeated in one week.
Liver disease
Chronic liver disease usually causes persistent thrombocytopenia, and manifests as cirrhosis, fibrosis, and portal hypertension. The most common cause is chronic alcohol abuse; 2 however, other aetiologies include viral hepatitis, drug-induced hepatotoxicity, non-alcoholic liver disease, and metabolic disorders.
Thrombocytopenia can result from direct toxic marrow suppression and/or splenic sequestration associated with hypersplenism and portal hypertension. 14 Folic acid deficiency (related to malnutrition) often coexists with alcohol abuse and represents another cause of thrombocytopenia. Abstinence and nutritional replacement often lead to platelet normalisation in three to four weeks in the absence of chronic liver disease. 2
Gestation thrombocytopenia
Gestational thrombocytopenia is the most common diagnosis of thrombocytopenia in pregnancy, occurring in 8% of pregnancies 15, but accounts for 70-80% of all causes of thrombocytopenia in pregnancy.16
It is a diagnosis of exclusion and typically occurs in the mid- second to third trimester. Two-thirds of individuals have a platelet count above 130 x 109/L and the PLT count is rarely below 70 x 109/L.
The mechanism is unknown, but is thought to be related to haemodilution and accelerated platelet clearance. Gestational thrombocytopenia is a benign clinical condition not associated with adverse maternal or neonatal outcomes and is characterised by spontaneous resolution after delivery. 16
Recommendations for the initial evaluation of thrombocytopenia in pregnancy include a thorough history, physical examination, FBC and blood film. Additional studies are determined on the basis of these findings. Mild ITP and gestational thrombocytopenia often are indistinguishable, however, a distinguishing feature of gestational thrombocytopenia is that the platelet count is rarely lower than 70 x 109/L and often presents in the third trimester.
In contrast, thrombocytopenia in ITP often precedes the pregnancy, typically manifests in the first two trimesters, and the PLT count is not infrequently below 70 x 109/L. 17
ITP in pregnancy requires a careful management plan between the obstetrician and haematologist to ensure PLT are at a safe level for delivery and invasive procedures such as Caesarian section and neuraxial anaesthesia. This involves the use of corticosteroids with or without IVIG close to the time of delivery.
As many as 12 to 15% of neonates delivered to women with ITP will develop platelet counts of less than 50.18 Therefore, the platelet count in infants must be closely monitored when ITP is suspected in the mother.
MANAGEMENT IN THE GP SETTING
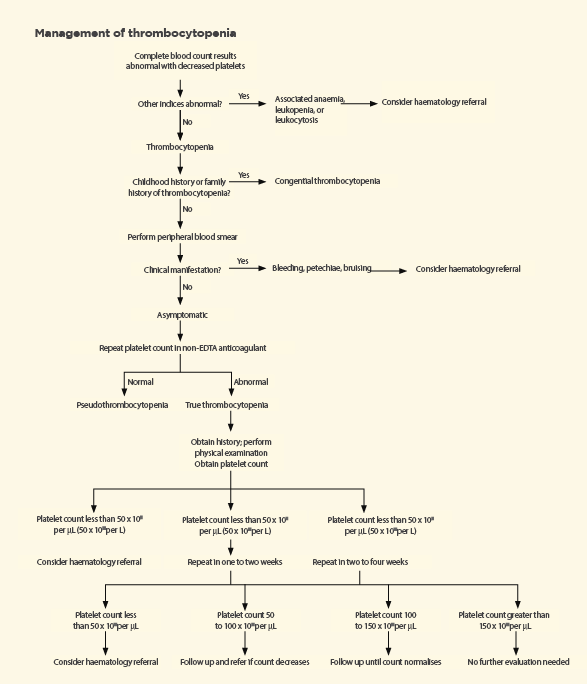
A suggested algorithm for the management of thrombocytopenia is shown in Figure 2 on page 26. Symptomatic patients require immediate evaluation. Patients with incidental mild-moderate thrombocytopenia (PLT 50-150 × 109/L) who are asymptomatic should have a platelet count repeated in one to four weeks depending on the severity of thrombocytopenia.19
Reassessment should be performed immediately if patients become symptomatic during the surveillance period. Additional laboratory evaluation should be performed as clinically indicated, and a trial of discontinuing medications known to decrease platelet counts is recommended.
Patients with transient thrombocytopenia in the setting of a known infection stable thrombocytopenia in the setting of chronic alcohol excess, chronic liver disease, known nutritional deficiencies, infective causes of suspected drug-induced thrombocytopenia do not require haematology referral and can be managed by the GP.
Patients with unexplained severe thrombocytopenia, decreasing platelet counts, additional haematological abnormalities, or associated bleeding complications should be referred to a haematologist.
ACTIVITY PARTICIPATION AND INVASIVE PROCEDURES
A platelet count greater than 50 × 109/L is adequate for haemostasis and is unlikely to be clinically recognised. Patients with a platelet count greater than this level can engage in most activities, but should use caution if participating in contact sports. 2
Patients with platelet counts less than 10 × 109/L should be restricted from contact sports and other potentially traumatic activities. Most surgical and invasive procedures can be performed safely in patients with platelet counts greater than 50 × 109/L. The exceptions to this rule is neuraxial anesthesia which requires a PLT count of > 80 × 109/L and neurosurgical procedures, which require PLT ? 100 × 109/L. (20)
LONG TERM OUTCOMES
The findings of isolated thrombocytopenia in an outpatient setting have prognostic implications.
A prospective study evaluated the long-term outcomes of patients with incidental thrombocytopenia. The study followed 217 persons with platelet counts from 100 to 150 × 109/L over a 10-year period. In 64% of patients, platelet counts normalised or remained stable.
The probability of developing immune thrombocytopenic purpura or an autoimmune disorder was approximately 7 and 12%, respectively. Four cases of MDS were diagnosed (2%), all of which were in older patients.19
Dr Kenny Tang is currently in his fourth year of advanced training in haemotology at Westmead Hospital in Sydney
References:
Gaydos LA, Freireich EJ, Mantel N. The quantitative relation between platelet count and hemorrhage in patients with acute leukemia. N Engl J Med. 1962; 266:905-909.
Gauer, Robert L., and Michael M. Braun. “Thrombocytopenia.” American family physician 85.6 (2012).
Stasi, Roberto. “How to approach thrombocytopenia.” ASH Education Program Book 2012.1 (2012): 191-197.
Terrell, Deirdra R., et al. “The incidence of immune thrombocytopenic purpura in children and adults: a critical review of published reports.” American journal of hematology85.3 (2010): 174-180.
Despotovic, Jenny M., and Amanda B. Grimes. “Pediatric ITP: is it different from adult ITP?.” ASH Education Program Book2018.1 (2018): 405-411.
Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115(2):168-186.
Page EE, Kremer Hovinga JA, Terrell DR, Vesely SK, George JN. Thrombotic thrombocytopenic purpura: diagnostic criteria, clinical features, and long-term outcomes from 1995 through 2015. Blood Adv. 2017;1(10):590-600.
Scully, Marie, et al. “Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies.” British journal of haematology 158.3 (2012): 323-335.
Lowe, Sandra A., et al. “SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014.” Australian and New Zealand Journal of Obstetrics and Gynaecology 55.5 (2015).
Killick, Sally B., et al. “Guidelines for the diagnosis and management of adult aplastic anaemia.” British journal of haematology 172.2 (2016): 187-207.
Van den Bemt PM, Meyboom RH, Egberts AC. Drug-induced immune thrombocytopenia. Drug Saf. 2004;27(15):1243-1252.
Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007;357(6):580-587.
Kenney B, Stack G. Drug-induced thrombocytopenia. Arch Pathol Lab Med. 2009;133(2):309-314.
Ballard HS. Hematological complications of alcoholism. Alcohol Clin Exp Res. 1989;13:706–720.
Boehlen F, Hohlfeld P, Extermann P, et al. Platelet count at term pregnancy: a reappraisal of the threshold. Obstet Gynecol. 2000;95(1):29-33.
Gernsheimer T, James AH, Stasi R, How I treat thrombocytopenia in pregnancy. Blood. 2013;121(1):38-47
Myers, Bethan. “Thrombocytopenia in pregnancy.” The Obstetrician & Gynaecologist 11.3 (2009): 177-183.
Webert KE, Mittal R, Sigouin C, Heddle NM, Kelton JG. A retrospective 11-year analysis of obstetric patients with idiopathic thrombocytopenic purpura. Blood. 2003;102(13):4306-4311.
Stasi R, Amadori S, Osborn J, Newland AC, Provan D. Long-term outcome of otherwise healthy individuals with incidentally discovered borderline thrombocytopenia. PLoS Med. 2006;3(3):e24.
Slichter SJ. Evidence-based platelet transfusion guidelines. Hemotology Am Soc Hematol Educ Program.:172-178.