The TGA has proposed a major overhaul of the medical device industry
In a set of sweeping proposed changes to the medical device industry, the TGA has backed mandatory reporting of adverse events by doctors and plans to put barcodes on packaging so each device can be tracked.
The TGA’s action plan, released earlier this month, is a response to the wave of concerns around transvaginal mesh implants, which have caused serious, and often traumatic, adverse events in women and were the subject of a Senate inquiry last year.
Under the current system, reporting of adverse events is mandatory for industry, but voluntary for doctors and patients.
But, as the transvaginal mesh story has demonstrated, there is a “need to access more complete data on adverse events … and to take quicker action”, the TGA said.
To speed up the reporting process, the TGA is considering making it compulsory for doctors and surgeons to report adverse events related to medical devices.
This would require legislative changes as the TGA currently has no regulatory authority to mandate medical practitioners to report adverse events under the Therapeutic Goods Act 1989.
The TGA is also planning to introduce smartphone apps so that patients can immediately report any problems with medical devices.
Unlike prescription medications (which are registered on the Australian Register of Therapeutic Goods), medical devices are not catalogued by the TGA, so it is difficult for patients to know where the device comes from, when it expires and what materials it contains.
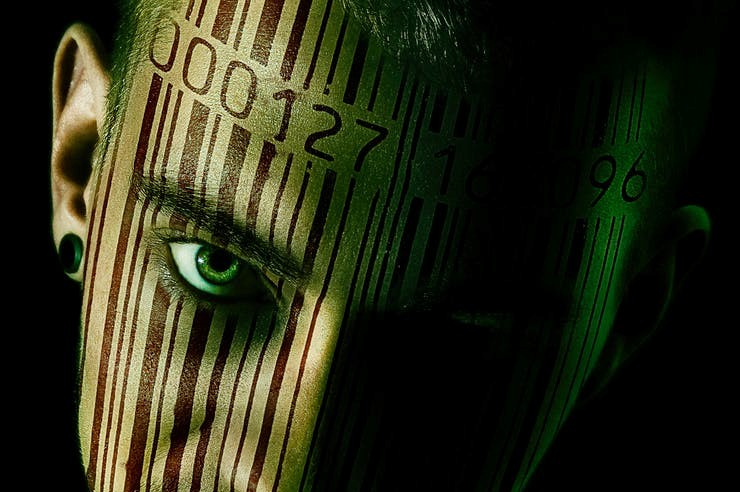
Under the TGA’s plan, medical devices will have an individual barcode (or unique device identifier) on their packaging. This barcode would make it easier for patients to access specific information about the device. It would also help regulators to track the product through the healthcare system. The federal government has already approved the introduction of a pilot pelvic mesh register.
This was one of the 13 recommendations made by the Senate inquiry into transvaginal mesh implants, and was supported in principle by the government in its response last year.
The TGA has committed to a one-year timeline to push through the public consultation period and introduce the necessary legislative changes.
The proposed changes were welcomed by the Public Health Association of Australia and the Medical Technology Association of Australia (MTAA).
“With the increasing sophistication of medical intervention comes a need for more sophisticated regulation,” Terry Slevin, the CEO of the Public Health Association of Australia, said. “This plan is important to respond to the changing medical landscape.”
Ian Burgess, the CEO of the MTAA, said Australia’s medical device regulation was “among the most stringent globally” and that a balance needed to be struck between ensuring that patients had timely access to new technology and ensuring that devices were appropriately scrutinised before they were placed on the market.
While manufacturers were legally obliged to report adverse events, once the device was in the hands of doctors, it was often difficult for manufacturers to capture and report that data, he said.
“We do agree that anything that improves the ability to be directly be reporting their concerns or what they consider to be adverse events and also anything that improves and encourages healthcare professionals to be reporting that’s in the best interest of patients,” he said.
The MTAA also supported the roll out of unique barcodes on medical device packaging.
“It will improve being able to track the actual device but also for patients to have much more readily accessible information around what is the device they have,” Mr Burgess said.