A GP’s initial clinical suspicion is the key to an early diagnosis and appropriate management in women with this condition.
Pelvic congestion syndrome is a chronic pain syndrome due to venous reflux causing pelvic venous congestion.
The pain is typically deep in the pelvis and is exacerbated by upright posture and physical activities.
Chronic pelvic pain is prevalent and is present in 15% of women. It is estimated that pelvic congestion syndrome accounts for 13 to 31% of chronic pelvic pain in women.1 Yet pelvic congestion syndrome is still often overlooked and underdiagnosed.
The aim of this article is to raise awareness of this condition so that early diagnosis can be made, and effective treatment can be offered to women.
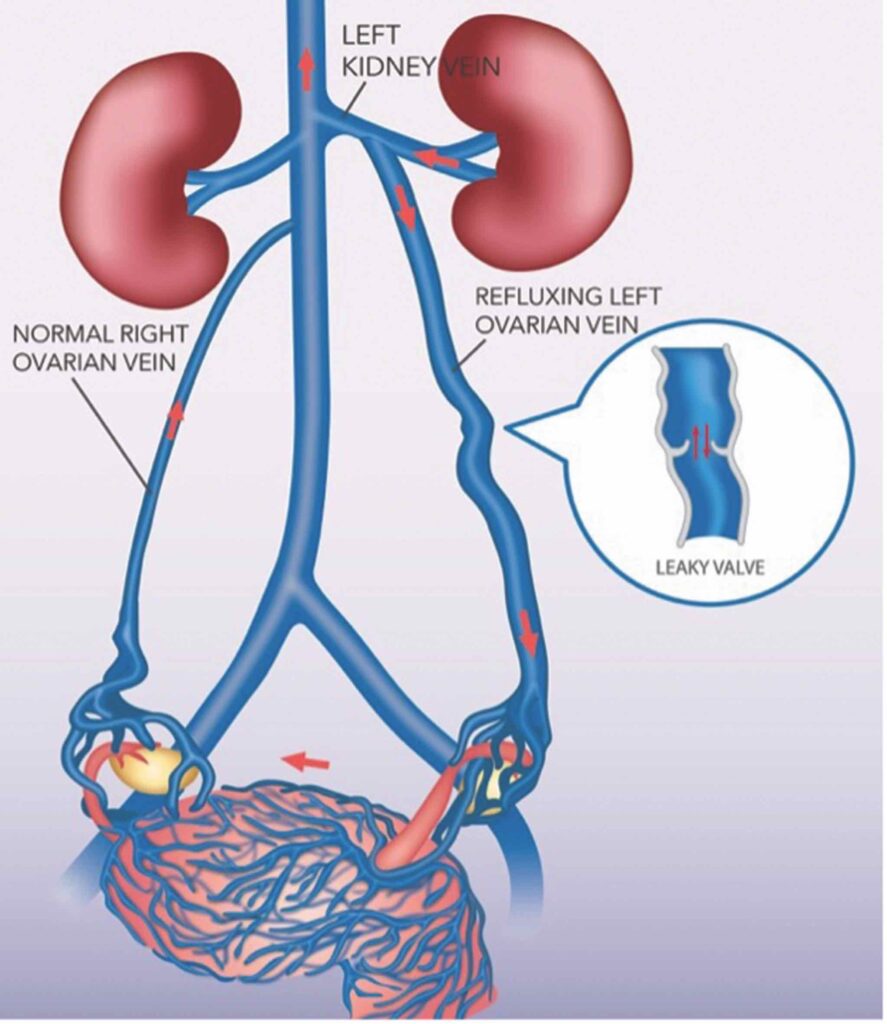
What is the pathophysiology?
Reflux and retrograde flow in the ovarian veins and iliac vein tributaries result in excessive flow and pressure causing congestion of the pelvic venous plexus.
The characteristic severe dull aching pain of pelvic congestion syndrome is thought to be a direct result of the presence of ovarian and pelvic varicosities, much like the leg pain resulting from lower extremity varicose veins.2
Blood pooling in the pelvic and ovarian veins may cause further engorgement, thrombosis, and mass effect on nearby nerves, collectively contributing to pelvic pain.3
Multiparous women seem to be predisposed to develop pelvic congestion syndrome. There is significant increase in intravascular volume during pregnancy. Venous distension can render the valves incompetent. The weight gain and anatomical changes in the pelvic structures during pregnancy may also cause chronic intermittent venous obstruction.2
Since the majority of women affected are premenopausal, and a relationship between pelvic congestion syndrome and endogenous oestrogen levels has been suggested, as oestrogen is known to weaken the vein walls.2
How to diagnose?
Pelvic pain in women is a complex issue. There can be more than one source of pain. Uterine fibroids, adenomyosis, endometriosis, pelvic inflammatory disease, adhesions related to previous pelvic surgery and Caesarean sections are prevalent and can often co-exist with pelvic congestion syndrome, which is also prevalent.
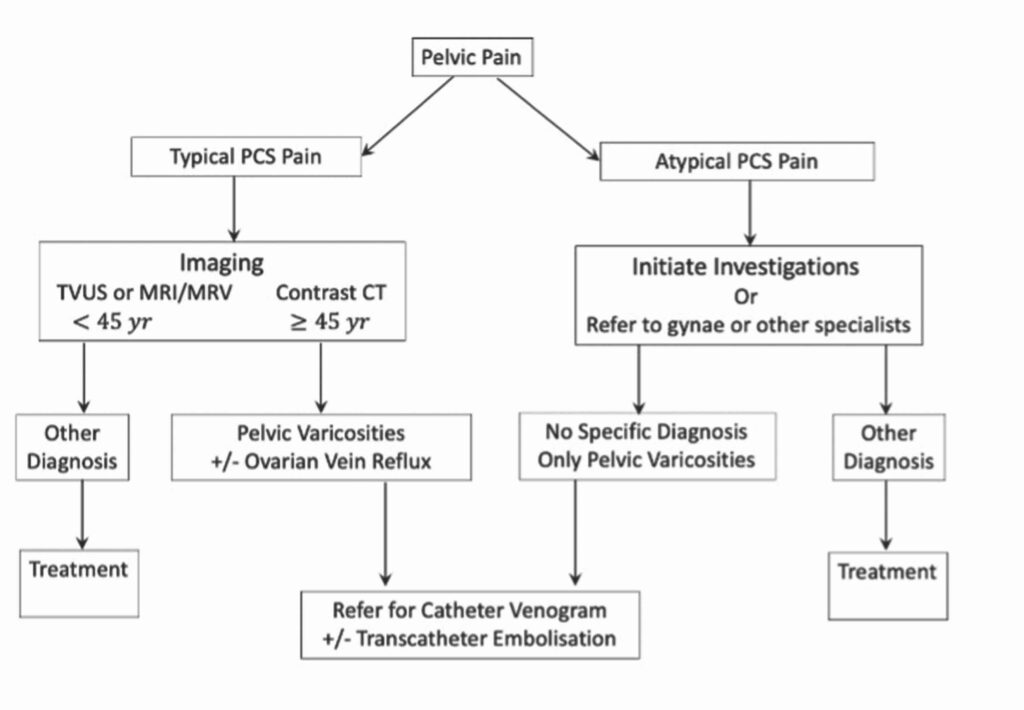
The most important factor in reaching an early diagnosis of pelvic congestion syndrome is clinical history. Women can present with very typical symptoms highly suggestive of pelvic congestion syndrome then the diagnosis can be easily established with supportive imaging findings of pelvic varicosities and ovarian vein reflux.
Other women might present with atypical symptoms that might have suggested alternative diagnoses, then further investigations and referral to specialists might be needed to exclude other pathologies.
Certainly, not every case of dilated veins in the pelvis represents pelvic congestion syndrome, and their mere presence does not relieve the clinician of the need for careful workup to exclude other possible coexistent causes of pelvic pain. (See flow chart)
What are the symptoms?
Typical pelvic congestion syndrome pain is:
- Heaviness and dull aching in nature
- Located deep in the pelvis and on the left
- Exacerbated by upright position (standing or sitting) and exercise (walking, running, weightlifting)
- Worse towards the end of the day
- Worse after sexual intercourse
- Worse when bladder is full
- Chronic and insidious onset
Atypical pelvic congestion syndrome pain is:
- Constant pain not related to time of day, upright posture or physical activities
- Pain worse premenstrually and during menstrual periods
- More on the right than the left
- Acute and sudden onset
- Sharp or colicky in nature
What are the physical signs?
Physical examination is often unremarkable other than non-specific adnexal and parametrial tenderness. Associated venous conditions might be noted, such as lower limb varicose veins; haemorrhoids; labial, vulvar and gluteal varicosities.
What is the best imaging test for evaluation?
The purpose of imaging is to look for pelvic varicosities and to demonstrate presence of ovarian vein reflux, if possible.
All non-invasive imaging like ultrasound, CT and MRI can detect pelvic varicosities. The key role for the GPs is to alert the imaging technicians and specialist to look out for pelvic varicosities and to report them. Since imaging is performed in the supine position, the degree of pelvic varicosities might be underestimated by all these modalities.
Ovarian vein reflux however is not always demonstrated on non-invasive imaging. Doppler ultrasound may sometimes demonstrate ovarian reflux but is often limited by patient physique and operator experience. MR venogram maybe more reliable to demonstrate ovarian vein reflux but is more expensive and not funded by Medicare for this purpose.
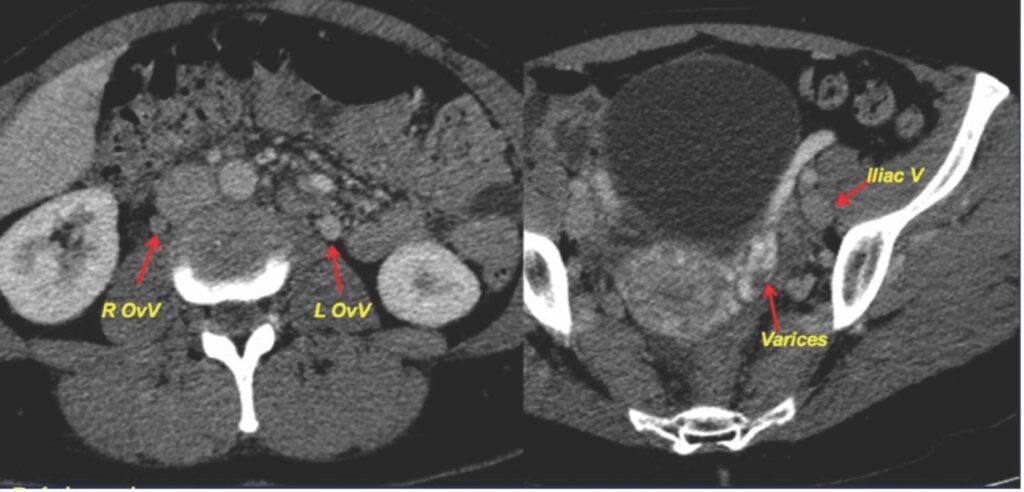
CT with contrast can easily demonstrate left ovarian vein reflux and pelvic varicosities, with earlier contrast arrival than iliac veins and infrarenal IVC. However, CT involves some radiation that is best avoided if possible, in women younger than 40 years.
CT can demonstrate venous anatomy in exquisite detail, at the left ovarian-renal vein junction and right ovarian-IVC junction and therefore is useful for embolisation planning, potentially reducing fluoroscopic time and contrast usage during ovarian vein embolisation procedure.
Nutcracker Syndrome (left renal vein compression) and May-Thurner Syndrome (left iliac vein compression) can also be detected by CT.
CT is also useful to exclude other pathologies not demonstrated by pelvic ultrasound.
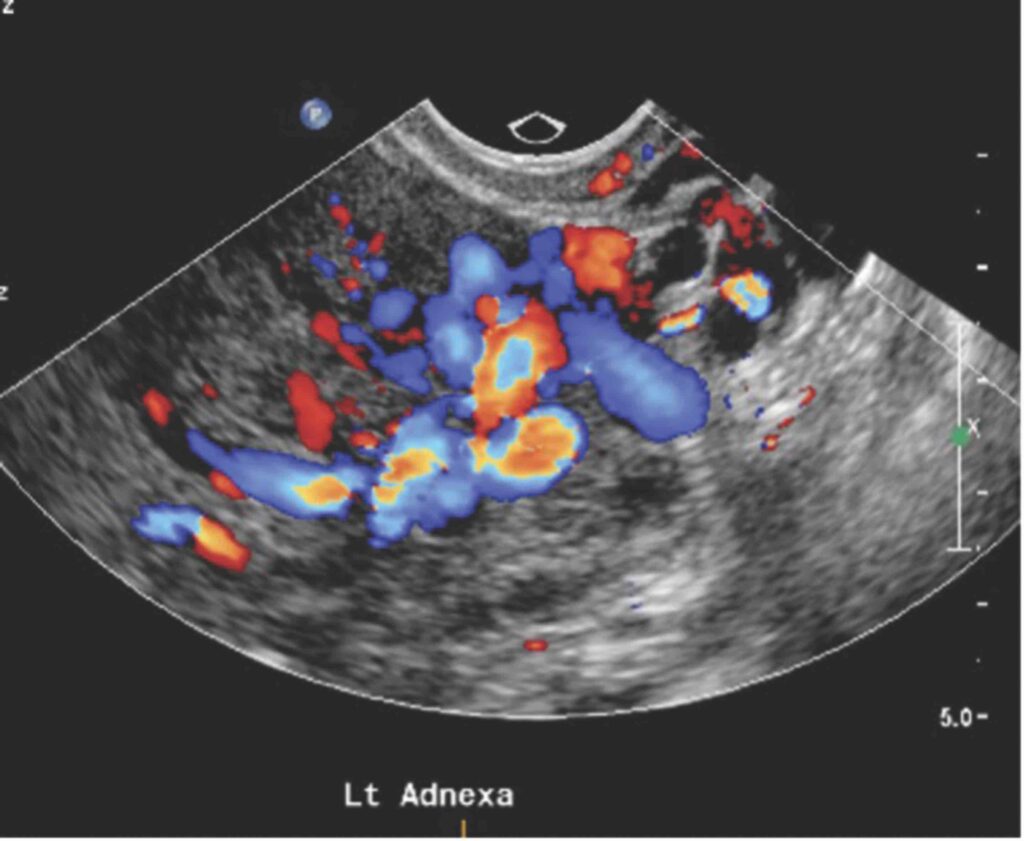
What are the sonographic features?
On transabdominal ultrasound, ovarian vein dilatation of more than 5mm might be seen and caudal flow might be demonstrated.
On transvaginal ultrasound (TVUS), dilated and tortuous pelvic venous plexus of more than 6mm may be noted.
A dilated intrauterine arcuate vein (> 5mm) crossing the midline is seen in 25% of cases.
Polycystic appearance of the ovaries may be present in 50% of patients.
Variable doppler flow changes with Valsalva have been noted, some showing reversed flow direction, other showing abrupt disappearance of flow or initial accentuation.4
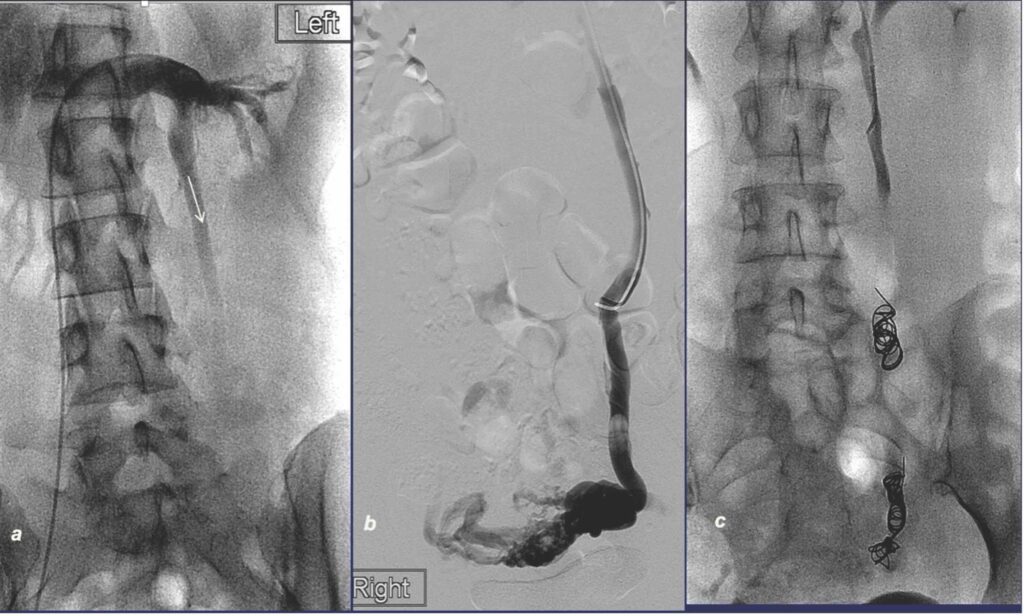
What is the role of catheter venogram?
Contrast venogram remains the gold standard to demonstrate reflux in the ovarian veins and tributaries of the internal iliac veins, as well the extent of pelvic varicosities fed by these refluxing veins. It is nowadays very rarely performed just for diagnostic purpose, but rather as part of a planned embolisation procedure. Refluxing ovarian veins are typically larger than 6mm in diameter, feeding dilated tortuous pelvic varicosities showing stagnation of contrast.
The procedure requires radiation, iodine contrast, and is minimally invasive. It provides dynamic flow information. Reflux can be elicited with Valsalva or by using a tilting table.
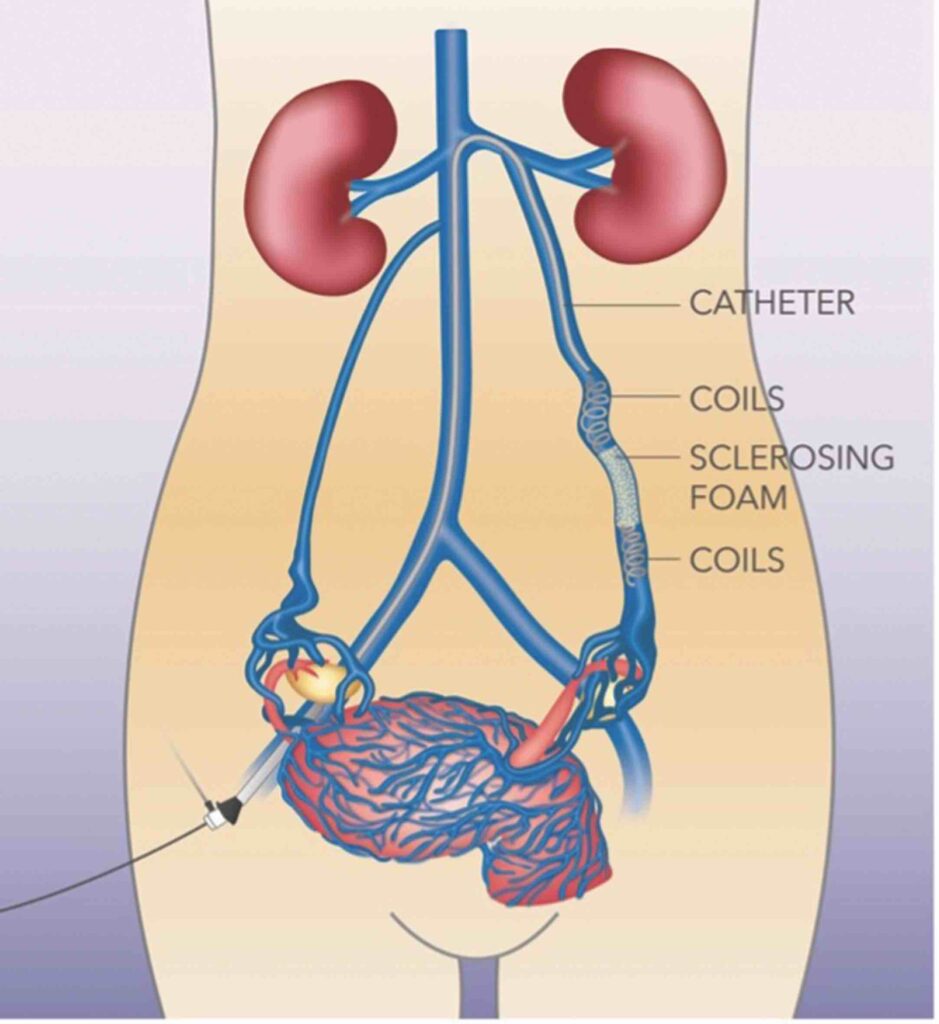
Transcatheter embolisation
Since the root cause of venous congestion is due to reflux, or retrograde flow, permanently blocking these refluxing veins will stop the inflow into the congested pelvic venous plexus, whose drainage is overwhelmed by the abnormal backflow.
Transcatheter embolisation is performed with conscious sedation under local anaesthetic, as a day procedure. It is one of the safest embolisation procedures, with no significant adverse post-embolisation symptoms or recovery issues, and no down time. The procedure risks are minimal and major complications very rare.
Access can be from punctures in the femoral vein, basilic vein in the arm or jugular vein in the neck. Venogram is first performed, to demonstrate reflux and venous anatomy. Once reflux is demonstrated, then the refluxing vein is then embolised with coils and a sclerosing agent. Left ovarian, right ovarian, and tributaries of the internal iliac veins are checked, and embolised if reflux is confirmed.
The procedure is very well tolerated. Some might experience loin pain related to the sclerosing agent injection. Others might have pelvic pain post-procedure, probably related to thrombophlebitis associated with the embolisation. This can be treated with non-steroidal anti-inflammatory drugs for a few days.
Some feel the relief of pelvic congestion syndrome symptoms soon after embolisation, while others might have to wait for the thrombophlebitis to settle before appreciating the result. It is best to wait for four to six weeks to judge the effectiveness of this treatment.
Technical success is generally very high. Complications are often minor, usually puncture site bruising and minor haematoma. Venous perforation from guidewire and catheter manipulation is uncommon, but is usually self-limiting for veins in the retroperitoneum, and is inconsequential if the vein was targeted for embolisation anyway.
Inadvertent coil migration into pulmonary artery or into the left renal vein has been reported, usually as a technical error during procedure. The misplaced coils can be retrieved using a snare or be left in the pulmonary circulation as an embolus, if small.
There are many case series reporting the clinical outcome of transcatheter embolisation since 1993. However, there are no randomised control trials to compare with any other treatment. This may reflect the absence of any other contender that is potentially less invasive or more effective than transcatheter embolisation.
Therefore, transcatheter embolisation should be regarded as the standard of care for women with pelvic congestion syndrome.
It is important to note that despite a very high technical success rate, clinical effectiveness is just over 80% in most case series.5,6
This probably reflects the complex nature of pelvic pain in women (there is likely to have more than one source of pain).
Uterine fibroids, adenomyosis, endometriosis, pelvic inflammatory disease, adhesions related to previous pelvic surgery and caesarean sections, are prevalent and can co-exist with pelvic congestion syndrome. Therefore, it is important to identify all possible causes of pelvic pain in a particular woman, weigh up their significance in contributing to the pain, and approach treatment selection from least invasive to most invasive options.
For example, if a woman has pelvic congestion syndrome as well as endometriosis, yet her day-to-day pain is bothering her more than her period pain, then perhaps she should consider transcatheter embolisation to treat her pelvic congestion syndrome first, and depending on symptom improvement, consider laparoscopic treatment of her endometriosis as a second step.
Does embolisation affect future pregnancies?
Some follow-up data suggest no negative effects on menstrual cycle, fertility, or ovarian hormone levels.7
A small case series has shown that pregnancies are safe after embolisation for pelvic congestion syndrome.8 However, women need to be warned that there is a high recurrence rate of pelvic congestion syndrome after subsequent pregnancy, therefore definitive treatment should perhaps be deferred till all desired pregnancies are complete.
What are less common causes?
Most of the pelvic congestion syndrome is caused by left ovarian vein reflux, less commonly also by refluxing right ovarian vein and internal iliac vein tributaries. These venous refluxes can all be treated with transcatheter embolisation.
Other less common causes are extrinsic compression by abdominal or pelvic masses, such as fibroids and malignant tumours.
There two rare venous compressive syndromes that may cause pelvic congestion syndrome.
The Nutcracker Syndrome is defined as compression of the left renal vein between the superior mesenteric artery and the aorta. Patients with this condition can present with low back or left flank pain and micro- or macrohaematuria. Compression of renal vein diverts the venous drainage of the left kidney into the pelvis via gonadal vein, leading to pelvic venous hypertension and pelvic congestion syndrome. If the patient’s symptoms are pelvic pain rather than loin pain and haematuria, one approach is to treat pelvic congestion syndrome with transcatheter embolisation which is minimally invasive. If left renal vein hypertension becomes symptomatic, then surgical transposition of the left renal vein is recommended and favoured over stenting.9
Non-thrombotic compression of the left common iliac vein by the right common iliac artery, referred to as the May-Thurner syndrome, can also lead to pelvic venous congestion.
Transcatheter placement of a stent in the left common iliac vein is the treatment of choice.9
What is the role of diagnostic laparoscopy?
Laparoscopy is often performed to diagnose and treat endometriosis and adhesions. As it is performed with the patient in supine or Trendelenburg position, and with the use of CO2 for abdominal distention, veins are often collapsed, and pelvic varicosities can be missed.
Should the surgeon suspect pelvic varicosities, reverse Trendelenburg position and easing off CO2 distention might allow the dilated veins to fill.
Since pelvic varicosities and ovarian reflux can be demonstrated with non-invasive imaging, diagnostic laparoscopy should not be performed just for suspected pelvic congestion syndrome.
Are there medical therapies?
Phlebotonics are often used for pelvic congestion syndrome, however their value in this condition has not been evaluated.9
These are venoactive drugs that are usually natural or synthetic flavonoids. They may improve venous tone and decrease capillary hyperpermeability. However, the mechanism of action is not scientifically well established. In the setting of treating lower limb chronic venous insufficiency,
Cochrane review 2020 concluded that they have limited efficacy for oedema and other symptoms and made little or no difference in quality of life.10
Treatment with medroxyprogesterone acetate or the gonadotropin-releasing hormone analog goserelin acetate may provide short-term relief of symptoms; however, recurrence is common and therefore not typically used for long-term.9,11,12 Pelvic congestion syndrome is a chronic disease which will not get better with time and therefore more definitive treatment should be sought.
Will hysterectomy cure PCS?
Hysterectomy will not cure pelvic congestion syndrome.
Residual pain post hysterectomy is seen in 33% of patients13 and a 20% symptom recurrence rate has been reported.14
The uterus is the victim of pelvic congestion but not the root cause of the pelvic congestion syndrome. Removing the uterus does not eliminate the pelvic venous plexus which can still be engorged post hysterectomy. This can be explained anatomically by the fact that the uterine veins drain directly into the internal iliac vein, as well as the ovarian vein by an arcade of anastomoses. Removing the uterus does not therefore necessarily significantly change the amount of blood flowing into the ovarian vein and does not correct the anatomical problem.
How about laparoscopic ligation of
ovarian veins?
This procedure reduces symptom in 80% of patients treated.15 It can be performed using a transperitoneal or retroperitoneal approach. It does not have better efficacy than transcatheter embolisation.16
This procedure is rarely performed because it is more invasive than transcatheter embolisation, requiring a general anaesthetic, and longer recovery period. Given that surgical ligation can only interrupt the refluxing pathway at a limited number of locations, recurrences may be more common.9
GPs play pivotal role in early diagnosis
GPs are often the first medical professional that a woman might complain to, about their pelvic pain. It is important that the GPs recognise the typical symptoms of pelvic congestion syndrome, and clearly indicate that suspicion on the imaging request, to alert the sonographers and imaging specialists to look for pelvic varicosities and ovarian vein reflux. Valsalva during scanning might be considered, to demonstrate reflux in such cases.
If the suspicion is not raised, pelvic varicosities might be overlooked and under-reported by imaging specialists. Subsequently, women with chronic pelvic pain are likely to be referred to specialists for further evaluations.
Gynaecologists quite likely will have to perform laparoscopy to exclude endometriosis and adhesions; gastroenterologists/general surgeons might have to perform endoscopy/colonoscopy to exclude bowel pathologies; pain specialists might have to perform various nerve blocks; and psychiatrists might have to be involved to manage pain-associated depression.
Therefore, GPs’ initial clinical suspicion is the key to an early diagnosis and appropriate management in women with pelvic congestion syndrome.
Of course, not all women with pelvic varicosities have pelvic congestion syndrome which is a pain syndrome, but presence of pelvic varicosities on imaging in a woman with typical symptoms of pelvic congestion syndrome should be sufficient to make the diagnosis and to refer on for further management with catheter venogram and transcatheter embolisation.
Dr Eisen Liang is an interventional radiologist and Dr Bevan Brown is an obstetrician gynaecologist. Together they have collaborated for more than 10 years and founded Sydney Fibroid Clinic to help women to resolve menstrual issues and pelvic pain. For further information, please visit Drs’ Resources on our website: www.sydneyfibroidclinic.com.au
References:
- Hobbs JT The Pelvic Congestion Syndrome. Br J Hosp Med 1990; 43:2
- Ignacio, E, et al Pelvic Congestion Syndrome: Diagnosis and Treatment Seminars in interventional radiology, 2008-12, Vol.25 (4), p.361-368
- Stones RW. Pelvic vascular congestion: half a century later. Clin Obstet Gynecol 2003;46(4):831–836
- Park et al Diagnosis of Pelvic Congestion Syndrome Using Transabdominal and Transvaginal Sonography AJR 2004;182:683–688
- Se Hwan Kwon, Joo Hyeong Oh, Kyung Ran Ko, Ho Chul Park, Joo Yup Huh Transcatheter Ovarian Vein Embolization Using Coils for the Treatment of Pelvic Congestion Syndrome Cardiovasc Intervent Radiology (2007) 30:655–661
- Kim HS, Malhotra AD, Rowe PC, Lee JM, Venbrux AC (2006) Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol 17(2 Pt 1):289–297
- Chiara Borghi, Lucio Dell’Atti Pelvic congestion syndrome: the current state of the literature Arch Gynecol Obstet (2016) 293:291–301
- Dos Santos, Scott J ; Holdstock, Judy M ; Harrison, Charmaine C ; Whiteley, Mark S The effect of a subsequent pregnancy after transjugular coil embolisation for pelvic vein reflux Phlebology, 2017-02, Vol.32 (1), p.27-33
- Javier L. Monedero, Santiago Z. Ezpeleta, Neil M. Khilnani Treatment options for pelvic congestion syndrome Phlebolymphology – Vol 23. No. 3. 2016
- Phlebotonics for venous insufficiency Maria José Martinez-Zapata, et al Version published: 03 November 2020 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003229.pub4/full?highlightAbstract=phlebotonics%7Cphleboton
- Gangar, K.F., Stones, R.W., Saunders, D. et al. (1993) An alternative to hysterectomy? GnRH analogue combined with hormone replacement therapy. Br. J. Obstet. Gynaecol., 100, 360–364.
- Soysal ME, Soysal S, Vidcan K, Ozer S. A randomized controlled trial of goserelin and medroxyprogesterone acetate I in the treatment of pelvic congestion. Hum Reprod 2001; 16(5):931–939
- Beard RW, Kennedy RG, Gangar KF, et al. Bilateral oophorectomy and hysterectomy in the treatment of intractable pelvic pain associated with pelvic congestion. Br J Obstet Gynaecol 1991;98(10):988–992
- Carter JE. Surgical treatment for chronic pelvic pain. JSLS 1998;2(2):129–139
- Gargiulo T, Mais V, Brokaj L, Cossu E, Melis GB. Bilateral laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndrome. J Am Assoc Gynecol Laparosc 2003;10(4):501–504
- Chung M-H, Huh C-Y. Comparison of treatments for pelvic congestion syndrome. Tohoku J Exp Med 2003;201:131–138


