Research shows patients with cirrhosis are not having their support needs met.
Cirrhosis, which is the advanced stage of a range of chronic liver diseases, causes significant morbidity and mortality, with deaths and hospital admissions due to cirrhosis increasing.[1]
Leading causes of cirrhosis include alcohol-related liver disease, chronic hepatitis B and C, and non-alcoholic fatty liver disease (NAFLD). Cirrhosis is also the greatest risk factor for primary liver cancer (hepatocellular carcinoma), which is the most rapidly rising cause of cancer death in Australia.[2]
Newly published research by QIMR Berghofer Medical Research Institute and The University of Queensland has revealed 88 per cent of patients with cirrhosis are not having their supportive care needs met, which could affect how patients manage their cirrhosis and its impact on their quality of life.[3]
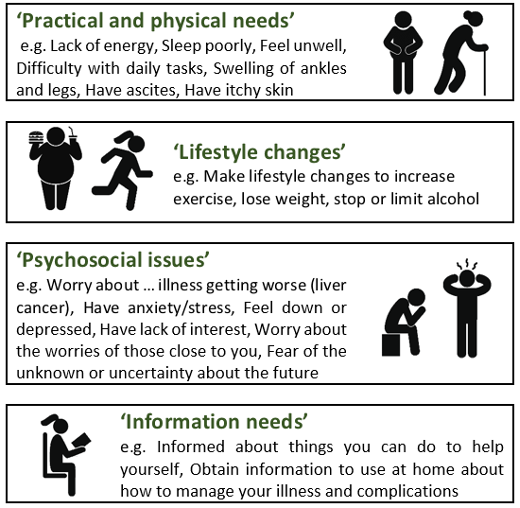
The researchers used a 39-item validated tool, the Supportive Needs Assessment tool for Cirrhosis (SNAC),[4] to collect data about the types and levels of supportive care needs of 458 Australian adults with cirrhosis. The SNAC tool sought to identify the needs of patients with cirrhosis in four areas, namely practical and physical needs, lifestyle changes, psychological issues, and information needs.
The study revealed 88 per cent of patients reported that they needed ‘A little’, ‘Some’, or ‘A lot’ of help with at least one item in the SNAC tool. Twenty per cent of patients indicated a moderate-to-high need for help (‘Some’, or ‘A lot’) with at least 16 items in the SNAC tool. Almost all patients (98 per cent) with advanced cirrhosis indicated a moderate-to-high need for help with at least one item.
“We found a range of unmet needs that were not being identified during patient consultations with their clinicians and that could have a negative impact on a patient’s adherence to treatment,” lead researcher, Professor Patricia Valery from QIMR Berghofer’s Cancer and Chronic Disease research group said.
“The study identified that the need for help with practical and physical issues increased with progressive severity of cirrhosis. In particular, patients indicated a moderate-to-high need for help with common, debilitating symptoms of cirrhosis. More than one-in-three patients reported they weren’t getting the help they needed from their health care providers to address their lack of energy, tiredness, and poor sleep, 31 per cent reported need for help with feeling unwell, and one in four patients indicated that they needed help with tasks around the house,” Professor Valery said.
“We also found that patients with more advanced cirrhosis had nearly twice the rate of need for help with psychosocial issues such as worries about illness getting worse and liver cancer, anxiety, stress, feeling down or depressed, and lack of interest, compared to patients in the early stages of cirrhosis.”
Moreover, the researchers found the level and type of unmet needs differed according to the patient age and liver disease aetiology, irrespective of liver disease severity.
Younger patients and those of working age (18-64 years) had increased need for help with practical and physical issues, psychosocial issues, and making lifestyle changes compared to patients aged 65 years or older.
“Even though our study did not investigate reasons for these differences in need according to age, younger patients may have fewer comorbidities and for that reason may be less experienced in navigating the health system and dealing with the practicalities of living with cirrhosis when compared to older patients,” Professor Valery said.
“Younger patients may have a dependent family, which would have an effect on the financial and practical burden of cirrhosis (e.g. taking time off work to attend hospital appointments for treatment). Lack of energy, poor sleep, and feeling unwell were the most commonly reported moderate-to-high unmet needs in patients aged 18-64 years. These issues may have far more impact in younger employed individuals than a retired person. The rate of practical and physical needs was 61 per cent higher among younger patients included in the study when compared to older patients.”
Patients with NAFLD had a higher rate of unmet needs than other liver disease aetiologies, specifically in the areas of lifestyle change and practical and physical needs.
These patients reported an increased need for help with lack of energy, difficulty with daily tasks, swelling of ankles and legs, making lifestyle changes and experiencing side effects of treatment, compared to patients with alcohol induced or chronic hepatitis induced cirrhosis. For example, the rate of moderate-to-high unmet needs with making lifestyle changes was 81 per cent higher among patients with NAFLD when compared to patients with alcohol induced cirrhosis.
The Queensland-led research concurs with findings from previous studies that identified a significant impairment of physical health-related patient reported outcomes in people with NASH and advanced fibrosis or cirrhosis, when compared to people with chronic hepatitis C [5], as well as lower quality of life when compared to people with NASH without cirrhosis.[6]
Director of the network Centre for Liver Disease Research at The University of Queensland, and Princess Alexandra Hospital Hepatologist, Professor Elizabeth Powell, said the complexity of the disease and the associated psychological and social impacts of a diagnosis of cirrhosis posed challenges for clinicians.
“Cirrhosis is characterised by an early phase where complications are absent and a ‘decompensated’ phase which is marked by the development of serious complications that require patients to have frequent hospital visits and admissions,” Professor Powell said.
“Moreover, many patients with cirrhosis need to follow complex medication and dietary regimens that may affect activities of daily living and quality of life. Some of these effects may resolve over time due to individual personal coping resources, or social and professional support, but as disease progresses some needs may emerge later or increase over time.
“Accurate assessment of the supportive needs of patients with cirrhosis is important to improve care and we believe the validated Supportive Needs Assessment tool for Cirrhosis (SNAC)[4] that we developed, and was used in this study, could help to identify those needs. This information is important in clinical practice, to help adapt strategies to promote patient-centred care and facilitate timely interventions or referral to appropriate support services.”
Supportive care embraces the full range of services and health providers such as general practitioners, social workers, dieticians, psychological support (e.g. psychiatrist, psychologist), exercise physiologist, and respite care. Supportive care interventions aim to help patients cope with their disease and maintain their quality of life. To be effective, supportive care must match up with a patient’s needs within the context of his or her unique situation.[7]
“From a clinical perspective, the use of the SNAC tool in the clinic could provide health professionals with a clear understanding of what patients need and assist them in providing the optimal support and care in the treatment of their cirrhosis.
From a research perspective, it’s also important that we get a better understanding of why patient needs are not being met, whether it be due to lack of needs assessment before patient management or because the available resources are inadequate or not being used. Such data can inform health planners (e.g. planning of resources and support services) and help researchers know what areas of research they should next embark on (e.g. build better tools),” Professor Valery said.
The study findings have been published in the journal Hepatology Communications.
The study was funded by the 2020 Queensland Metro South Health Research Support Scheme Project (Women in Health Research).
Professor Patricia Valery is the head of the Cancer and Chronic Disease research group at QIMR Berghofer Medical Research Institute. Her research focus includes the epidemiology and management of chronic liver disease and liver cancer.
Professor Elizabeth Powell is a Hepatologist and Senior Staff Specialist in the Department of Gastroenterology and Hepatology, Princess Alexandra Hospital. She is also Professor, School of Medicine, The University of Queensland and Director of the network Centre for Liver Disease Research.
References
1. Powell EE, Skoien R, Rahman T, Clark PJ, O’Beirne J, Hartel G, Stuart KA, McPhail SM, Gupta R, Boyd P, Valery PC. Increasing Hospitalization Rates for Cirrhosis: Overrepresentation of Disadvantaged Australians. EClinicalMedicine. 2019 Jun 13;11:44-53.
2. MacLachlan JH, Cowie BC. Liver cancer is the fastest increasing cause of cancer death in Australians. Med J Aust 2012; 197: 492–493.
3. Valery PC, Bernardes CM, Mckilen B, Amarasena S, Stuart KA, et al. The patient’s perspective in cirrhosis: Unmet supportive care needs differ by disease severity, etiology, and age. Hepatol Communications 2021 in press
4. Valery PC, Bernardes CM, Stuart KA, Hartel GF, McPhail SM, Skoien R, et al. Development and evaluation of the supportive needs assessment tool for cirrhosis (SNAC). Patient Prefer Adherence 2020;14:599-611.
5. Younossi ZM, Stepanova M, Lawitz EJ, Reddy KR, Wai-Sun Wong V, Mangia A, Muir AJ, et al. Patients With Nonalcoholic Steatohepatitis Experience Severe Impairment of Health-Related Quality of Life. Am J Gastroenterol 2019;114:1636-1641.
6. McSweeney L, Breckons M, Fattakhova G, Oluboyede Y, Vale L, Ternent L, Balp MM, et al. Health-related quality of life and patient-reported outcome measures in NASH-related cirrhosis. JHEP Rep 2020;2:100099.
7. Fitch MI. Supportive care framework. Can Oncol Nurs J 2008;18:6-24.