While influenza is clearly a real threat to public health, annual vaccinations do little to protect the population against serious illness, says Professor Chris del Mar
Professor Chris del Mar has questioned the value of population-wide flu vaccinations in a controversial presentation at the inaugural GPs Down Under conference.
While influenza was clearly a real threat to public health, annual flu vaccinations did little to protect the population against serious illness, Professor del Mar, a public health expert at Bond University, said.
“It seems to me that public health is overselling the influenza vaccine,” he said.
Speaking at GPDU18, which was held on the Gold Coast May 30 to June 1, Professor del Mar acknowledged the influenza vaccine usually decreased the risk of infection by about 50%, but said the absolute risk reduction was quite low.
He quoted a recently-updated Cochrane review which showed the flu vaccine only reduced the rate of laboratory-confirmed influenza from 2% to 1%.
The meta-analysis of RCTs revealed that nine out of 1,000 people who were vaccinated caught the flu compared with 23 out of 1,000 people who were not vaccinated.
“That’s a very, very small difference,” said Professor del Mar. “For an individual, it probably means you have to be immunised 50 years in a row to save you getting one infection,” Professor Peter Collignon, an infectious disease physician at ANU, told The Medical Republic.
Professor Collignon, who did not speak at GPDU18, questioned the wisdom of pushing everyone in the population, particularly children, to be immunised every year.
There was even some evidence that being infected by wild influenza provided better protection against pandemic flu than yearly vaccinations, he said.
“Having said that, for high-risk people with significant underlying disease, it’s still worth getting the influenza vaccine,” he said. “It may not be perfect, but it’s probably better than nothing.”
The “other side to the coin” was that the influenza vaccine caused febrile convulsions in around one in 100 children who were vaccinated in Australia, and had been linked with at least two deaths, Professor del Mar said.
The Cochrane review, which included 40 years’ worth of data from tens of thousands of healthy adults across North America, South America, and Europe, also showed that the influenza vaccine did not significantly decrease the rate of hospital admissions or deaths from flu.
“So the next question is, if we are not going to promote influenza vaccine, is there anything else we can do instead?” Professor del Mar asked.
Tamiflu might help individual symptoms but it was “pretty hopeless” as a public health response, he said.
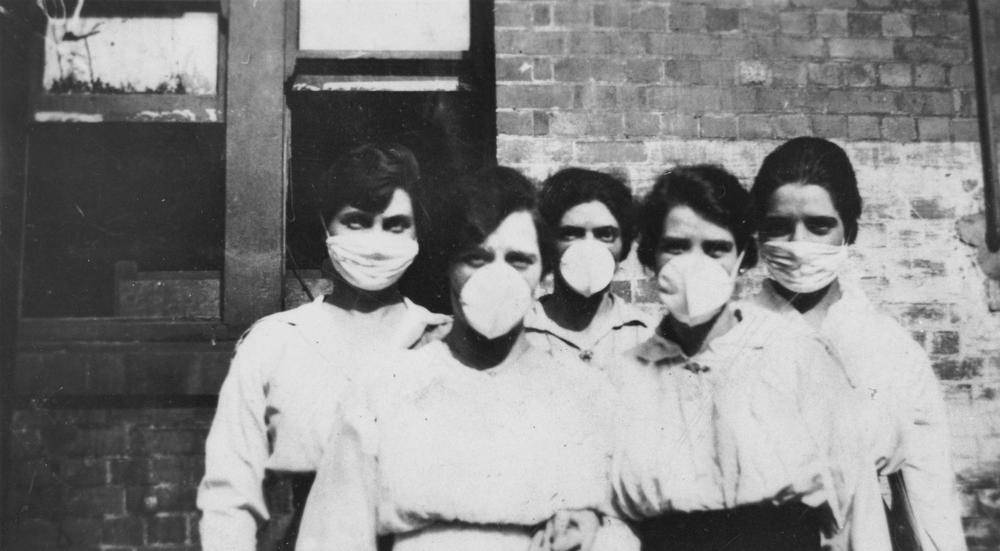
Professor Collignon said the most effective intervention against the spread of influenza was hand washing and face masks, which provided around 70 to 80% protection.
But these common-sense measures were not as popular as medications or vaccines. “One of the problems with the modern world is we want an instant answer for everything,” he said.
Allen Cheng, a professor in infectious disease epidemiology at Monash University, told The Medical Republic that the 1 to 2% rate for influenza infections reported by Cochrane was at odds with other studies, which placed the annual global incidence rate of influenza at around 10 to 15%.
PCR-confirmed influenza was also the “tip of an iceberg of illness”, and many people with influenza never visited a GP, he said.
“The 233,000 flu notifications last year [in Australia] almost certainly is an underestimate of the true burden of disease,” he said. The Cochrane review only included healthy adults, who were much less vulnerable than elderly people to complications from influenza, Professor Cheng said.
“I don’t think anyone is arguing against hand washing and masks, but (a) these are more complex and expensive interventions at a population level than a single $10 vaccine and (b) there’s no reason why we can’t do both,” he said.